Abstract
Background
The beneficial effects of deep blockade are not fully known. In this study, we evaluated the effect of deep neuromuscular blockade on surgical conditions during laparoscopic cholecystectomy under low-pressure pneumoperitoneum.
Methods
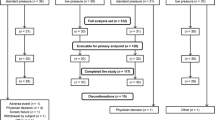
Patients undergoing elective laparoscopic cholecystectomy were randomized to either the moderate group (train-of-four count of 1 or 2) or deep group (posttetanic count of 1 or 2). Neuromuscular blockade was induced and maintained with rocuronium; it was reversed with sugammadex in the deep group and with neostigmine in the moderate group. At the beginning of surgery, the intra-abdominal pressure was set at 8 mmHg. The surgeon rated the surgical condition on a 4-point scale (1 = excellent, 2 = good, 3 = acceptable, 4 = poor) and was allowed to increase the pressure to 12 mmHg if it was determined that the surgical conditions were inadequate for the operation.
Results
A total of 64 patients completed the study. The rate of increasing intra-abdominal pressure to maintain optimal surgical conditions was 34.4 % in the moderate group and 12.5 % in the deep group (P = 0.039). The proportion of patients with a surgical condition score of 1 or 2 (excellent or good) was 34.4 % in the moderate group and 68.8 % in the deep group (P = 0.006).
Conclusion
The maintenance of intraoperative deep neuromuscular blockade was associated with a lower rate of conversion to standard pressure and higher surgeon satisfaction with the surgical conditions than was moderate blockade in patients undergoing low-pressure pneumoperitoneum laparoscopic cholecystectomy.


Similar content being viewed by others
References
Murphy GS, Szokol JW, Marymont JH et al (2008) Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg 107:130–137
Murphy GS, Szokol JW, Avram MJ, Greenberg SB et al (2011) Intraoperative acceleromyography monitoring reduces symptoms of muscle weakness and improves quality of recovery in the early postoperative period. Anesthesiology 115:946–954
Fuchs-Buder T, Meistelman C, Raft J (2013) Sugammadex: clinical development and practical use. Korean J Anesthesiol 65:495–500
Wallace DH, Serpell MG, Baxter JN et al (1997) Randomized trial of different insufflation pressures for laparoscopic cholecystectomy. Br J Surg 84:455–458
Gurusamy KS, Samraj K, Davidson BR (2009) Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev 2
Sarli L, Costi R, Sansebastiano G et al (2000) Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy. Br J Surg 87:1161–1165
Vijayaraghavan N, Sistla SC, Kundra P et al (2014) Comparison of standard-pressure and low-pressure pneumoperitoneum in laparoscopic cholecystectomy: a double blinded randomized controlled study. Surg Laparosc Endosc Percutaneous Tech 24:127–133
Fuchs-Buder T, Claudius C, Skovgaard LT et al (2007) Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockholm revision. Acta Anaesthesiol Scand 51:789–808
Dubois PE, Putz L, Jamart J et al (2014) Deep neuromuscular block improves surgical conditions during laparoscopic hysterectomy: a randomised controlled trial. Eur J Anaesthesiol 31:430–436
Geldner G, Niskanen M, Laurila P et al (2012) A randomised controlled trial comparing sugammadex and neostigmine at different depths of neuromuscular blockade in patients undergoing laparoscopic surgery. Anesthesia 67:991–998
Chambers D, Paulden M, Paton F et al (2010) Sugammadex for the reversal of muscle relaxation in general anesthesia: a systematic review and economic assessment. Health Technol Assess 14:1–211
Martini CH, Boon M, Bevers RF et al (2014) Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br J Anaesth 112:498–505
Barczynski M, Herman RM (2003) A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc 17:533–538
Joshipura VP, Haribhakti SP, Patel NR et al (2009) A prospective randomized, controlled study comparing low pressure versus high pressure pneumoperitoneum during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutaneous Tech 19:234–240
Matsuzaki S, Jardon K, Maleysson E et al (2012) Impact of intraperitoneal pressure of a CO2 pneumoperitoneum on the surgical peritoneal environment. Hum Reprod 27:1613–1623
Kirov K, Motamed C, Dhonneur G (2001) Differential sensitivity of abdominal muscles and the diaphragm to mivacurium: an electromyographic study. Anesthesiology 95:1323–1328
Donati F, Meistelman C, Plaud B (1991) Vecuronium neuromuscular blockade at the adductor muscles of the larynx and adductor pollicis. Anesthesiology 74:833–837
Fernando PU, Viby-Mogensen J, Bonsu AK et al (1987) Relationship between posttetanic count and response to carinal stimulation during vecuronium-induced neuromuscular blockade. Acta Anaesthesiol Scand 31:593–596
Ledowski T, Falke L, Johnston F et al (2014) Retrospective investigation of postoperative outcome after reversal of residual neuromuscular blockade: sugammadex, neostigmine or no reversal. Eur J Anaesthesiol 31:423–429
Watts RW, London JA, van Wijk RM et al (2012) The influence of unrestricted use of sugammadex on clinical anaesthetic practice in a tertiary teaching hospital. Anaesth Intensive Care 40:333–339
Acknowledgments
Supported by a Grant (02-2013-088) from the Seoul National University Bundang Hospital Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
none.
Additional information
Trial registration number: registered at cris.nih.go.kr (KCT0001090).
Rights and permissions
About this article
Cite this article
Koo, BW., Oh, AY., Seo, KS. et al. Randomized Clinical Trial of Moderate Versus Deep Neuromuscular Block for Low-Pressure Pneumoperitoneum During Laparoscopic Cholecystectomy. World J Surg 40, 2898–2903 (2016). https://doi.org/10.1007/s00268-016-3633-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3633-8