Abstract
Introduction
Despite advances in trauma care, hemorrhage continues to be the leading cause of preventable mortality in trauma. The evidence to support its use in non-trauma patients is limited. We aim to report our experience with prehospital blood product transfusion. We hypothesize that it is safe, appropriately utilized, and that our protocol, which was designed for trauma patients, is adaptable to fit the needs of non-trauma patients.
Methods
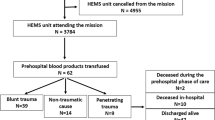
Patients transfused with blood products, packed red blood cells (pRBCs) or plasma, in the prehospital environment between 2002 and 2014 were included. Trauma patients were compared to non-trauma patients using descriptive statistics.
Results
A total of 857 patients (n = 549 trauma and n = 308 non-trauma) were transfused with pRBCs (76 %, n = 654, mean 1.6 ± 1.1 units en route), plasma (53 %, n = 455, mean 1.7 ± 0.7 unit), or both (29 %, n = 252) during ground (12 %) or air (84 %) critical care transport. Mean age was 60.8 ± 21.6 years with 60.1 % (n = 515) males. Subsequently, in-hospital blood transfusions were performed in 80 % of patients, operations in 44 %, and endoscopy in 31 %. Five percent (n = 41) of patients did not require any of these interventions. Thirty-day mortality rate was 18 %, and one patient (<0.01 %) had a transfusion reaction. The majority of patients were non-trauma (n = 549, 64 %). Of the non-trauma patients, 219 (40 %) were surgical, 193 (35 %) gastrointestinal bleeds, and 137 (25 %) medical.
Conclusion
Both non-trauma and trauma patients require blood products for life threatening hemorrhage and the majority required further interventions. Further research on the benefits of transfusion among non-trauma patients is warranted.

Similar content being viewed by others
Abbreviations
- INR:
-
International normalized ratio
- LOS:
-
Length of stay
- pRBC:
-
Packed red blood cells
- PTT:
-
Partial thromboplastin time
References
Kauvar DS, Wade CE (2005) The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care 9(Suppl 5):S1–S9
Teixeira PGR, Inaba K, Hadjizacharia P et al (2007) Preventable or potentially preventable mortality at a mature trauma center. J Trauma 63:1338–1346 discussion 1346–1347
Gonzalez EA, Moore FA, Holcomb JB et al (2007) Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma 62:112–119
Berns KS, Zietlow SP (1998) Blood usage in rotor-wing transport. Air Med J 17:105–108
Higgins GL, Baumann MR, Kendall KM et al (2012) Red blood cell transfusion: experience in a rural aeromedical transport service. Prehosp Disaster Med 27:231–234
Jenkins D, Stubbs J, Williams S et al (2014) Implementation and execution of civilian remote damage control resuscitation programs. Shock 41:84–89
Riskin DJ, Tsai TC, Riskin L et al (2009) Massive transfusion protocols: the role of aggressive resuscitation versus product ratio in mortality reduction. J Am Coll Surg 209:198–205
Mitra B, Mori A, Cameron PA et al (2010) Fresh frozen plasma (FFP) use during massive blood transfusion in trauma resuscitation. Injury 41:35–39
Pidcoke HF, Aden JK, Mora AG et al (2012) Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom. J Trauma Acute Care Surg 73:S445–S452
Hooper TJ, Nadler R, Badloe J et al (2014) Implementation and execution of military forward resuscitation programs. Shock 41(Suppl 1):90–97
Bhangu A, Nepogodiev D, Doughty H, Bowley DM (2013) Meta-analysis of plasma to red blood cell ratios and mortality in massive blood transfusions for trauma. Injury 44:1693–1699. doi:10.1016/j.injury.2012.07.193
del Junco DJ, Holcomb JB, Fox EE et al (2013) Resuscitate early with plasma and platelets or balance blood products gradually: findings from the PROMMTT study. J Trauma Acute Care Surg 75:S24–S30
Novak DJ, Bai Y, Cooke RK et al (2015) Making thawed universal donor plasma available rapidly for massively bleeding trauma patients: experience from the Pragmatic, Randomized Optimal Platelets and Plasma Ratios (PROPPR) trial. Transfusion 55:1331–1339
Bodnar D, Rashford S, Hurn C et al (2013) Characteristics and outcomes of patients administered blood in the prehospital environment by a road based trauma response team. Emerg Med J 31:583–588
Kim BD, Zielinski MD, Jenkins DH et al (2012) The effects of prehospital plasma on patients with injury. J Trauma Acute Care Surg 73:S49–S53
Zielinski MD, Smoot DL, Stubbs JR et al (2013) The development and feasibility of a remote damage control resuscitation prehospital plasma transfusion protocol for warfarin reversal for patients with traumatic brain injury. Transfusion 53:59S–64S
Bodnar D, Rashford S, Williams S et al (2012) The feasibility of civilian prehospital trauma teams carrying and administering packed red blood cells. Emerg Med J 31:93–95
Lucas DJ, Ejaz A, Haut ER et al (2014) Interhospital transfer and adverse outcomes after general surgery: implications for pay for performance. J Am Coll Surg 218:393–400
Abbenbroek B, Duffield CM, Elliott D (2014) The intensive care unit volume-mortality relationship, is bigger better? An integrative literature review. Aust Crit Care 27:157–164 quiz 165
Ferraris VA, Hochstetler M, Martin JT et al (2015) Blood transfusion and adverse surgical outcomes: the good and the bad. Surgery 158:608–617
Ejaz A, Frank SM, Spolverato G et al (2015) Potential economic impact of using a restrictive transfusion trigger among patients undergoing major abdominal surgery. JAMA Surg 150:625–630
Shaw RE, Johnson CK, Ferrari G et al (2014) Blood transfusion in cardiac surgery does increase the risk of 5-year mortality: results from a contemporary series of 1714 propensity-matched patients. Transfusion 54:1106–1113
Acknowledgments
This study was supported by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery (Thiels, Glasgow, and Habermann); grant from the National Heart, Lung, and Blood Institute T32 HL105355 (Aho); and CTSA Grant KL2 TR000136 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH) (Zielinski). These funders had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the article.
Author contributions
Thiels, Habermann, Zietlow, and Zielinski contributed to the conception and design. Thiels, Aho, Fahy, Berns, and Parker contributed to the acquisition of data. Thiels, Glasgow, and Zielinski contributed to the analysis and interpretation of the data. The authors participated in writing the manuscript and critical revision and have approved of the final version.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Thiels, C.A., Aho, J.M., Fahy, A.S. et al. Prehospital Blood Transfusions in Non-Trauma Patients. World J Surg 40, 2297–2304 (2016). https://doi.org/10.1007/s00268-016-3572-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3572-4