Abstract
Background
Little is known about the breadth and quality of nonobstetric surgical care delivered by nonphysician clinicians (NPCs) in low-resource settings. We aimed to document the scope of NPC surgical practice and characterize outcomes after major surgery performed by nonphysicians in Tanzania.
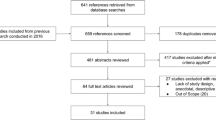
Methods
A retrospective records review of major surgical procedures (MSPs) performed in 2012 was conducted at seven hospitals in Pwani Region, Tanzania. Patient and procedure characteristics and level of surgical care provider were documented for each procedure. Rates of postoperative morbidity and mortality after nonobstetric MSPs performed by NPCs and physicians were compared using multivariate logistic regression.
Results
There were 6.5 surgical care providers per 100,000 population performing a mean rate of 461 procedures per 100,000 population during the study period. Of these cases, 1,698 (34.7 %) were nonobstetric MSPs. NPCs performed 55.8 % of nonobstetric MSPs followed by surgical specialists (28.7 %) and medical officers (15.5 %). The most common nonobstetric MSPs performed by NPCs were elective groin hernia repair, prostatectomy, exploratory laparotomy, and hydrocelectomy. Postoperative mortality was 1.7 % and 1.5 % in cases done by NPCs and physicians respectively. There was no significant difference in outcomes after procedures performed by NPCs compared with physicians.
Conclusions
Surgical output is low and the workforce is limited in Tanzania. NPCs performed the majority of major surgical procedures during the study period. Outcomes after nonobstetric major surgical procedures done by NPCs and physicians were similar. Task-shifting of surgical care to nonphysicians may be a safe and sustainable way to address the global surgical workforce crisis.


Similar content being viewed by others
References
Medical Association of Tanzania (2010) Proceedings of the 43rd annual general meeting. http://www.mat-tz.org. Accessed 6 Jun 2012
American College of Surgeons Health Policy Research Institute (2011) United States Atlas of the Surgical Workforce. http://www.acshpri.org/atlas. Accessed 28 Apr 2013
Mkony CA (2012) Emergence of a university of health sciences: health professions education in Tanzania. J Public Health Policy 33:S45–S63
McCord C, Mbaruku G, Pereira C et al (2009) The quality of emergency obstetrical surgery by assistant medical officers in Tanzanian district hospitals. Health Aff 28:w876–w885
Mullan F, Frehywot S (2007) Non-physician clinicians in 47 African countries. Lancet 360:2158–2163
World Health Organization (2008) Treat, train, retain. Task-shifting: global recommendations and guidelines. http://www.who.int/healthsystems/taskshifting/en. Accessed 23 Jul 2013
Kruk ME, Wladis A, Mbembati N et al (2010) Human resource and funding constraints for essential surgery in district hospitals in Africa: a retrospective cross-sectional survey. PLoS Med 7(3):e1000242
Pereira C, Bugalho A, Bergstrom S et al (1996) A comparative study of cesarean deliveries by assistant medical officers and obstetricians in Mozambique. Br J Obstet Gynaecol 103:508–512
National Bureau of Statistics and Coast Regional Commissioners Office (2007) United Republic of Tanzania Coast Region socioeconomic profile. http://www.tanzania.go.tz/regions/COAST.pdf. Accessed 29 May 2013
World Health Organization (2013) Tool for situational analysis to assess emergency and essential surgical care. http://www.who.int/surgery/publications/QuickSitAnalysisEESCsurvey.pdf. Accessed 28 Apr 2013
Weiser TG, Regenbogen SE, Thompson KD et al (2008) An estimation of the global volume of surgery: a modeling strategy based on available data. Lancet 372:139–144
United Republic of Tanzania Ministry of Health (2000) Curriculum for Assistant Medical Officer. http://www.almc.habari.co.tz/amo/AMO_Curriculum.pdf. Accessed 17 Sept 2012
Aust JB, Henderson W, Khuri S et al (2005) The impact of operative complexity on patient risk factors. Ann Surg 241:1024–1028
Walker IA, Obua AD, Mouton F et al (2010) Paediatric surgery and anesthesia in south-western Uganda: a cross sectional survey. Bull World Health Organ 88:897–906
Galakunde M, von Schreeb J, Wladis A et al (2010) Essential surgery at the district hospital: a retrospective descriptive analysis in three African countries. PLoS Med 7(3):e10000243
Mbah N (2007) Morbidity and mortality associated with inguinal hernia in northwestern Nigeria. West Afr J Med 26:288–292
Wilhelm TJ, Thawe IK, Mwatibu B et al (2011) Efficacy of major general surgery performed by non-physician clinicians at a central hospital in Malawi. Trop Dr 41:71–75
Renner RM, Brahmi D, Kapp N (2013) Who can provide effective and safe termination of pregnancy care? A systematic review. BJOG 120(10):23–31
Dulisse B, Cromwell J (2010) No harm found when nurse anesthetists work without supervision by physicians. Health Aff 8:1469–1475
Acknowledgments
We received funding for this project from the UCSF Department of Surgery.
Conflict of interest
JHB, LBO, LA, AM, CAM, and RAD have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beard, J.H., Oresanya, L.B., Akoko, L. et al. Surgical Task-Shifting in a Low-Resource Setting: Outcomes After Major Surgery Performed by Nonphysician Clinicians in Tanzania. World J Surg 38, 1398–1404 (2014). https://doi.org/10.1007/s00268-013-2446-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2446-2