Abstract
Background
Prospective studies comparing the efficacy of selective versus nonselective alpha blockers for preoperative preparation of pheochromocytoma (PCC) are lacking. In this prospective nonrandomized study, we compared the outcome of preoperative preparation with phenoxybenzamine (PBZ) and prazosin (PRZ) in terms of perioperative hemodynamic alterations.
Methods
The study was conducted at a tertiary referral center from July 2010 to December 2012. Thirty-two patients with PCC underwent operation after adequate preparation with PBZ (n = 15) or PRZ (n = 17). Five pediatric and adolescent patients were excluded because of different hemodynamics in this population. Perioperative monitoring was done for pulse rate (PR) and blood pressure (BP) alterations, occurrence of arrhythmias, and time taken to achieve hemodynamic stability. Groups were compared with the Mann–Whitney test, Student’s t test, and the χ 2 test as applicable.
Results
Patients in the two groups were similar in age, gender, 24 h urinary metanephrine and normetanephrine levels, and type of procedure. Patients prepared with PRZ had significantly more intraoperative episodes of transient hypertension (systolic BP ≥ 160 mmHg) and hypertensive urgency (BP > 180/110 mmHg) (p 0.02, 0.03, respectively). More patients receiving PRZ suffered from transient severe hypertension (SBP ≥ 220 mmHg) (p 0.03). The PRZ group also had more median maximum SBP (233 mmHg vs PBZ 181.5 mmHg) (p = 0.01) and lesser median minimum SBP (71 mmHg vs PBZ 78 mmHg) (p 0.03). No significant differences were found between the study groups for changes in PR, postoperative BP alterations, occurrence of arrhythmias, and time taken to achieve hemodynamic stability.
Conclusions
PBZ was found superior to PRZ in having fewer intraoperative hemodynamic fluctuations.
Similar content being viewed by others
Introduction
Pheochromocytoma (PCC) and paraganglioma are tumors arising from catecholamine-producing chromaffin cells in the adrenal medulla or extra-adrenal sympathetic/parasympathetic ganglia, respectively [1]. Surgery is the only available curative treatment. Tumor manipulation during operation can release excess catecholamines that may lead to potentially lethal hypertensive crises and arrhythmias. This release of catecholamines can be seen in normotensive and asymptomatic patients as well [2]. Therefore it is recommended that all patients receive appropriate preoperative medical management to block the effects of circulating catecholamines [3]. This preoperative preparation is usually in the form of α-blockers that can be nonselective or selective. However, there is no recommendation for the preferred drug for preoperative preparation. Prospective studies that compare the α-blockers of choice are lacking in the literature. Therefore we designed this prospective study to find which of the following two commonly used drugs for preoperative α-blockade, i.e., phenoxybenzamine (PBZ) (nonselective) and prazosin (PRZ) (selective) is better in terms of preventing perioperative hemodynamic alterations in PCC.
Methods
This prospective nonrandomized study was conducted at the departments of Endocrine Surgery and Endocrinology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, during July 2010 to Dec 2012 after approval from the Institutional Ethics Committee. All consecutive patients with biochemical diagnosis of PCC during the study period were enrolled. Patients who were not proven to have PCC on histopathology or who did not undergo surgery were excluded. Demographic and clinical profiles of the patients were recorded for age, gender, weight, and body mass index (BMI); levels of 24 h urinary metanephrine and normetanephrine; tumor size, number, and location (adrenal/extra-adrenal); associated familial syndromes; cardiomyopathy; and blood pressure (BP) status (normotensive/hypertensive). As per the department protocol, normotensive patients were also given α-blockade for preoperative preparation.
All patients underwent operation after adequate preparation with an α-blocker, either PBZ or PRZ. The selection of α-blocker was done based on individual surgeon and endocrinologist preference. Patients were advised to take liberal fluids and salt during the preoperative period. Adequacy of preparation was defined as all systolic blood pressure (SBP) recordings <160 mmHg on the day before surgery with no hypertensive surges [4]. Prolonged blockade (>4 weeks) was needed in some patients receiving PRZ, all for logistic reasons. Beta-blockers (propranolol, metoprolol, atenolol) were used in all but one patient. Other anithypertensives like calcium channel blockers (amlodipine), ACE inhibitors (ramipril), or angiotensin II inhibitors (telmisartan) were used when BP control was not achieved after 1 week of α-blockers. Side effects were recorded in the form of first dose hypotension and nasal stuffiness.
All patients underwent operation under general anesthesia by expert endocrine surgeons. Surgeons had enough expertise to perform all kinds of procedures either open or endoscopic (transperitoneal or retroperitoneal). The following intraoperative factors were recorded: surgical approach, duration of surgery, number of antihypertensives and vasopressors required per patient, number of patients requiring antihypertensives or vasopressors, intravenous (IV) fluids (crystalloids and colloids) infused, BP and heart rate (HR) fluctuations, occurrence of arrhythmias and other adverse events. Recordings for BP and HR were done to the nearest 5 min. Hypertension was defined as SBP ≥ 160 mmHg, and severe hypertension was defined as SBP ≥ 180 mmHg. Hypotension was defined as SBP < 80 mmHg [5]. Intraoperative tachycardia and bradycardia were defined as HR > 120/min and <60/min, respectively. Fluctuations in SBP and HR (severe hypertension, hypotension, tachycardia, bradycardia) were defined as transient (when fluctuation was present for <10 min) and prolonged (when fluctuation was present for >10 min) [5]. Transient hypertensive episodes were graded into various classes: SBP 160–179, 180–199, 200–219, and ≥ 220 mmHg. We followed the general criteria defined by Hebert and Vidt [6] for hypertensive urgency as BP > 180/110 mmHg and hypertensive emergency as BP > 220/140 mmHg, and we used those criteria for intraoperative recordings. There was no uniform protocol followed by the anesthetists to control intraoperative hypertension and hypotension. Intraoperative hypertension was managed by antihypertensive drugs like nitroprusside, nitroglycerine, metoprolol, labetalol, or MgSO4, and hypotension was managed by intravenous fluids and vasopressor drugs like noradrenaline, adrenaline, dobutamine, phenylephrine, or vasopressin.
Postoperative hemodynamic stability was defined as HR between 60 and 100/min, SBP between 80 and 160 mmHg, and when there was no need for vasopressor, ventilator, or intensive care unit (ICU) support. The following postoperative data were recorded: time taken to achieve hemodynamic stability, duration of ventilator support, duration of ICU stay, postoperative hypotension, and quantity of IV fluids (crystalloids and colloids) infused. The primary end point of the study was taken as the time when the patient had achieved hemodynamic stability in the postoperative period. The secondary end point was the time of discharge from the hospital, indicating that the patient was doing well and had no need for further hospitalization.
Student’s t test was used to compare parametric variables. The Mann–Whitney U-test was used to assess significance when distribution was not normal. Categorical variables were compared with the χ 2 test with the Yates correction for continuity when applicable. Values <0.05 (two-tailed) were considered significant. Data analysis was performed with SPSS 15.0 software (SPSS Inc., Chicago, IL).
Results
Thirty-four patients during the study period were divided in two groups (PBZ: 16 patients; PRZ: 18 patients) in a nonrandomized manner. Initially we planned to include all patients; however, five pediatric and adolescent patients (1 receiving PBZ and 4 receiving PRZ) were excluded during data analysis because the hemodynamics of this population differ from those of adults. One patient with a right suprarenal mass and hypertension had 24 h urinary normetanephrine 1,099 μg/day (normal: 0–600 μg/day). He was prepared with PRZ and underwent operation, but the lesion was later found on histopathology to be a renal cell carcinoma arising from the superior pole of the kidney. For this reason, this patient was excluded from analysis. One patient prepared with PBZ had cardiomyopathy and congestive heart failure. His condition did not improve even after starting PBZ, and he died of congestive heart failure after 5 days on PBZ and thus was excluded from analysis. After these exclusions, 27 patients were included in the final data analysis (14 PBZ patients and 13 PRZ patients).
Most patients had one tumor. However, four patients on PBZ and three on PRZ had more than one tumor; all had bilateral tumors except for one in each group. Associations with familial syndromes were seen in six patients in the PBZ group and two patients in the PRZ group. All patients were hypertensive except for three in the PBZ group. Two of these patients were diagnosed with incidentaloma; one was later proved to be part of the multiple endocrine neoplasia type 2 (MEN 2A) syndrome, and the third patient was a sibling of a MEN 2A patient, diagnosed on screening.
Two patients had arrhythmias (both atrial fibrillation) before starting α-blockers (1 received PBZ, and 1 received PRZ) and were managed with digoxin that was continued during the period of preoperative preparation by α-blocker as well.
Clinical profile and surgical approaches in the two groups were comparable, as shown in Table 1. All patients were operated by consultant surgeons and were assisted by trainees. All patients underwent operation by the transperitoneal approach (open and laparoscopic) except for two patients in the endoscopy group who were receiving PBZ and were operated on by the retroperitoneal approach. There was no difference between the types of endoscopic procedures when subset analysis was done by comparing transperitoneal laparoscopy and retroperitoneal endoscopy.
A summary of the drugs used for preoperative preparation is shown in Table 2. Both drugs were well tolerated by the patients, and side effects were comparable in the two groups. Duration of α-blockade was significantly greater with PRZ; however, it was due to logistic reasons only. Time taken to achieve adequate blockade was greater with PRZ, although the difference was not significant. A significantly greater number of patients in the PRZ group needed antihypertensive drugs in addition to α and β blockers (p 0.03). Also, the number of additional drugs required per patient to control BP was significantly higher with PRZ (p 0.04). These additional drugs were the antihypertensive drugs other than α and β-blockers.
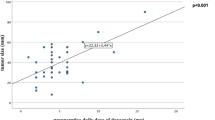
Drugs used for induction of anesthesia were various combinations of midazolam, fentanyl, propofol, and thiopentone. Vecuronium was used as muscle relaxant in all patients. Intraoperative hemodynamic events are illustrated in Tables 3, 4, 5. Eleven patients in each group developed intraoperative hypertension. Patients prepared with PRZ experienced a significantly higher number of hypertensive episodes (p 0.02). More patients receiving PRZ suffered from a higher grade of severe transient hypertension, i.e., SBP ≥ 220 mmHg (p 0.03). More patients prepared with PRZ developed prolonged hypertension and hypertensive urgency, although the difference was not significant. However, among those patients who developed hypertensive urgency, a significantly greater number of episodes were seen in patients receiving PRZ (p 0.03). Hypertensive emergency occurred only in the PRZ group. Median maximum SBP (233 vs 181.5 mmHg) was also significantly higher (p 0.01) with PRZ.
Hypotension after adrenal vein ligation was seen in 18 patients (8 in the PBZ group and 10 in the PRZ group). No significant differences were seen in hypotensive episodes between the study groups. However, the minimum median SBP (71 mmHg vs 78.5 mmHg) was significantly lower with PRZ (p 0.03). The range of SBP was also greater in the PRZ group (48–305 mmHg) as compared to the PBZ group (58–225 mmHg). Prolonged bradycardia was seen more often with PBZ but not significant. Other HR fluctuations were also not significant.
Intraoperative medications and fluids are shown in Table 6. PRZ group required more number of antihypertensive drugs during surgery, though not significant (p 0.16). On the other hand, number of vasopressors required with PBZ was more but not significant (p 0.19). PBZ group required more IV fluids, but the differences was not significant. Two patients (both PRZ) developed intraoperative arrhythmias (p 0.43). One of them had pre-existing atrial fibrillation, and the other patient developed junctional arrhythmia. These patients were managed with digoxin and atropine, respectively.
Postoperative parameters are summarized in Table 7. Hypotension was not seen in either group, as patients were maintained on vasopressors. There was no significant difference in the fluid requirements and need of support (ICU, ventilator, vasopressors, and antihypertensives) between the study groups.
Three patients in the PBZ group developed surgical site infections that were evident when patients were hemodynamically stable and shifted out of the ICU. One patient in the PBZ group had postoperative bleeding on day 1 due to disseminated intravascular coagulation and required packed RBC transfusions. Patients who had undergone bilateral adrenalectomy (3 receiving PBZ and 2 receiving PRZ) underwent operation under perioperative steroid cover and were discharged on oral steroids (prednisolone and fludrocortisone). Persistent hypercatecholaminemia was seen in three patients (2 receiving PBZ, 1 receiving PRZ).
Postoperative estimation of 24 h fractionated urinary metanephrine was not done in two patients from each group. The rest of patients (12 receiving PBZ and 11 receiving PRZ) had biochemical cure following surgery.
Discussion
PCC surgery has been associated with high perioperative mortality owing to massive sudden release of catecholamines intraoperatively and profound hypotension and shock after tumor removal. To overcome these effects, perioperative use of α-blockers and volume expansion was suggested. PBZ is a long-acting nonselective α-blocker that has been used since the early 1950s [7]. PRZ was first used by Wallace and Gill [8] in 1978. Since then PBZ or PRZ or other selective α1-blockers have been used for preoperative management of PCC. However, the efficacy of a particular drug over the others has not been studied prospectively, although a few retrospective studies can be found in the literature.
Weingarten et al. [9] compared different types of preoperative preparation by using selective and nonselective α-blockers and other drugs and found better results with PBZ in controlling intraoperative hypertension episodes and minimizing use of intraoperative IV fluids. We also found fewer intraoperative hypertension episodes with PBZ but no difference in IV fluids. However, the groups in the study by Weingarten et al. [9] were not homogeneous regarding preoperative preparation, as in the selective α-blocker group many other drugs were also administered with or without selective α-blockers. Hence, on the basis of their result, no conclusion can be reached for the superiority of types of α-blockers.
In another study, Russell et al. [10] claimed superiority of PBZ over PRZ, but there was heterogeneity in the number of patients (12 received PBZ and 1 received PRZ); hence the results cannot be generalized. Kocak et al. [11] found intraoperative hypertension in a significant number of their patients (80 %). In subgroup analysis, 81 % on PBZ, 73 % on PRZ, and 82 % on doxazosin had suffered intraoperative hypertension, but there was no statistical significance [11].
We had significantly different maximum SBP between our two groups (181.5 vs 233 mmHg) when compared to the study of Prys-Roberts and Farndon, who observed a greater maximum SBP with PBZ when compared to another selective α-blocker, doxazosin (185 mmHg vs 178 mm Hg) [12]. Their PBZ patients also had significantly higher HR intraoperatively, but postoperatively HR was seen to be greater with doxazosin. Significantly lower SBP was seen with PBZ in the immediate postoperative period [12]. Their results were not confirmed in our study, and there was no difference in intraoperative and postoperative HR and postoperative SBP.
In another study, Bruynzeel et al. [13] did not find a significant difference in postoperative SBP in patients receiving PBZ and doxazosin, which is similar to our results, but their postoperative mean arterial pressure was significantly greater with PBZ. They also reported prolonged changes in SBP with doxazosin, although the difference was not significant. Zhu et al. [14] favored doxazosin over PBZ as they had significantly fewer episodes of postoperative hypotension and fewer intraoperative SBP fluctuations with doxazosin.
We also compared our results with studies using single alpha-blockers without any comparative groups. Walz et al. [15] prepared patients with PBZ; only 8 % had SBP > 200 mmHg as compared to 29 % in our study. Similarly, 79 and 57 % of our patients experienced intraoperative SBP ≥ 160 mmHg and <80 mmHg, respectively, as compared to 58 and 41 %, respectively, from the report of Virseda Rodriguez et al. [16]. We achieved adequate preparation with lesser median dose of PBZ (27.5 mg) as compared to Kazic et al. [17] (40 mg) and had fewer patients with SBP > 220 mmHg (14 % vs 27 %). Maximum SBP in our patients on PBZ was lower (225 mmHg) than that of Kazic et al. [17] (290 mmHg). However, the same was comparable to Mihai et al. [2] (230 mmHg). Prolonged hypotension was almost three times higher than in the study by Kazic et al. [17] (21 % vs 7.5 %).
Scholten et al. [18] prepared their patients with doxazosin only but attributed intraoperative hemodynamic instability to preoperative tumor size. Toniato et al. [19] also used doxazosin exclusively but had less intraoperative hypertension (45 %) and hypotension (20 %) than our patients (85 and 77 %, respectively). Kasahara et al. [20] used PRZ or doxazosin, and 29 % of their patients had intraoperative SBP > 200 mmHg, much less than ours (69 %). Their frequency of intraoperative hypotension was also less than ours (59 vs 77 %) [20]. Results from the study of Tauzin-Fin et al. [21] (PRZ followed by urapidil) showed intraoperative hypertension in 67 % and hypotension in 22 % of patients, less than our results (85 and 77 %, respectively) [21].
Conclusions
In summary, blockade with PBZ was found to be superior to blockade with PRZ. Patients prepared with PBZ had lesser requirement for additional drugs in the preoperative period. They also had a lower frequency of intraoperative hypertensive and hypotensive events when compared with the PRZ group. Patients taking either drug had comparable fluid and drug requirements during surgery and in the postoperative period, and they had comparable postoperative hemodynamic profiles.
Our study has certain limitations. We could not perform randomization, which would have provided more strength to the study. Study groups were also small, but they were carefully selected, and by removing children and adolescents from our study, we maintained a homogeneous study population. A further randomized trial is necessary to confirm our results. In view of the relative rarity of these tumors, multicenter trials would be ideal.
References
Lloyd RV, Tischler AS, Kimura N et al (2004) Adrenal tumors: introduction. In: Delellis RA, Lloyd RV, Heitz PU, Eng Charis (eds) World Health Organization classification of tumors, pathology and genetics of tumors of endocrine organs. IARC Press, Lyon, p 138
Mihai R, Sadler GP, Bridge H (2008) Adrenergic blockade with phenoxybenzamine and propranolol in a cohort of 60 patients undergoing surgery for pheochromocytoma. Eur J Anaesthesiol 25:508–510
Pacak K, Eisenhofer G, Ahlman H et al (2007) Pheochromocytoma: recommendations for clinical practice from the First International Symposium. Nat Clin Pract Endocrinol Metab 3:92–102
Witteles RM, Kaplan EL, Roizen MF (2000) Safe and cost-effective preparation of patients with pheochromocytoma. Anesth Analg 91:302–304
Kinney MAO, Warner ME, vanHeerden JA et al (2000) Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesth Analg 91:1118–1123
Hebert CJ, Vidt DG (2008) Hypertensive crises. Prim Care 35:475–487
Prys-Roberts C (2000) Phaeochromocytoma—recent progress in its management. Br J Anaesth 85:44–57
Wallace JM, Gill DP (1978) Prazosin in the diagnosis and treatment of pheochromocytoma. JAMA 240:2752–2753
Weingarten TN, Cata JP, O’Hara JF et al (2010) Comparison of two preoperative medical management strategies for laparoscopic resection of pheochromocytoma. Urology 76:508e6–508e11
Russell WJ, Metcalfe IR, Tonkin AL et al (1998) The preoperative management of phaeochromocytoma. Anaesth Intensive Care 26:196–200
Kocak S, Aydintug S, Canakci N (2002) Alpha blockade in preoperative preparation of patients with pheochromocytomas. Int Surg 87:191–194
Prys-Roberts C, Farndon JR (2002) Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World J Surg 26:1037–1042. doi:10.1007/s00268-002-6667-z
Bruynzeel H, Feelders RA, Groenland TH et al (2010) Risk factors for hemodynamic instability during surgery for pheochromocytoma. J Clin Endocinol Metab 95:678–685
Zhu Y, He HC, Su TW et al (2010) Selective α1-adrenoceptor antagonist (controlled release tablets) in preoperative management of pheochromocytoma. Endocrine 38:254–259
Walz MK, Peitgen K, Neumann HP et al (2002) Endoscopic treatment of solitary, bilateral, multiple, and recurrent pheochromocytomas and paragangliomas. World J Surg 26:1005–1012. doi:10.1007/s00268-002-6632-x
Virseda Rodriguez JA, Martinez Ruiz J, Carrion Lopez P et al (2010) Pheochromocytoma: more than a decade of experience. Review of the literature. Actas Urol Esp 34:888–892
Kazic MR, Zivaljevic VR, Milan ZB et al (2011) Perioperative risk factors, morbidity, and outcome of 145 patients during pheochromocytoma resection. Acta Chir 111:223–227
Scholten A, Vriens MR, Cromheecke GJ et al (2011) Hemodynamic instability during resection of pheochromocytoma in MEN versus non-MEN patients. Eur J Endocrinol 165:91–96
Toniato A, Boschin IM, Opocher G (2007) Is laparoscopic adrenalectomy for pheochromocytoma the best treatment? Surgery 141:723–727
Kasahara T, Nishiyama T, Takahashi K (2009) Laparoscopic adrenalectomy for pheochromocytoma: evaluation of experience and strategy at a single institute. BJU Int 103:218–222
Tauzin-Fin P, Sesay M, Gosse P et al (2004) Effects of perioperative alpha1 block on hemodynamic control during laparoscopic surgery for pheochromocytoma. Br J Anaesth 92:512–517
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agrawal, R., Mishra, S.K., Bhatia, E. et al. Prospective Study to Compare Peri-operative Hemodynamic Alterations following Preparation for Pheochromocytoma Surgery by Phenoxybenzamine or Prazosin. World J Surg 38, 716–723 (2014). https://doi.org/10.1007/s00268-013-2325-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2325-x