Abstract
Background
Studies have claimed that in the surgical treatment of pancreas body and tail cancer, radical antegrade modular pancreatosplenectomy (RAMPS) is associated with effective tangential margin and extensive lymph node dissection. In the present study, the authors have compared the surgical outcomes between RAMPS and conventional distal pancreatosplenectomy (DPS) in patients with adenocarcinoma of the pancreas body and tail, and also identified prognostic factors associated with survival after surgery.
Methods
Retrospective review of 92 consecutive patients who underwent surgical resection for pancreas body and tail adenocarcinoma with curative intent between 1995 and 2010. Median follow-up duration was 16.1 months.
Results
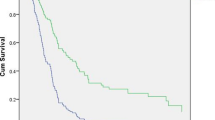
Of the 92 patients, 38 patients received RAMPS and 54 patients received DPS. Patients who underwent RAMPS had a greater number of retrieved lymph nodes than patients undergoing DPS [median 14 (5–52) vs. 9 (1–36), p < 0.05]. Conventional DPS, no adjuvant chemoradiation therapy (CRT), and non-curative resection were associated with poor overall survival (OS) on univariate analysis. After multivariate analysis for these variables, only the lack of adjuvant CRT and resection margin status were found to adversely affect OS.
Conclusions
While the RAMPS procedure is effective in performing an extensive LN dissection, it is not associated with better retroperitoneal resection margin or retrieval of more positive LNs, and it does not lead to better curability or OS survival compared to DPS. Lack of adjuvant CRT and resection margin status are poor prognostic factors in patients with pancreas body and tail cancer.


Similar content being viewed by others
References
Harrison LE, Klimstra DS, Brennan MF (1996) Isolated portal vein involvement in pancreatic adenocarcinoma. A contraindication for resection? Ann Surg 224:342–347 discussion 347–349
Jimenez RE, Warshaw AL, Rattner DW et al (2000) Impact of laparoscopic staging in the treatment of pancreatic cancer. Arch Surg 135:409–414 discussion 414–405
Johnson CD, Schwall G, Flechtenmacher J et al (1993) Resection for adenocarcinoma of the body and tail of the pancreas. Br J Surg 80:1177–1179
Kalser MH, Barkin J, MacIntyre JM (1985) Pancreatic cancer. Assessment of prognosis by clinical presentation. Cancer 56:397–402
Nakase A, Matsumoto Y, Uchida K et al (1977) Surgical treatment of cancer of the pancreas and the periampullary region: cumulative results in 57 institutions in Japan. Ann Surg 185:52–57
Strasberg SM, Linehan DC, Hawkins WG (2007) Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg 204:244–249
Mitchem JB, Hamilton N, Gao F et al (2012) Long-term results of resection of adenocarcinoma of the body and tail of the pancreas using radical antegrade modular pancreatosplenectomy procedure. J Am Coll Surg 214:46–52
Strasberg SM, Drebin JA, Linehan D (2003) Radical antegrade modular pancreatosplenectomy. Surgery 133:521–527
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Shimada K, Sakamoto Y, Sano T et al (2006) Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery 139:288–295
Christein JD, Kendrick ML, Iqbal CW et al (2005) Distal pancreatectomy for resectable adenocarcinoma of the body and tail of the pancreas. J Gastrointest Surg 9:922–927
Shoup M, Conlon KC, Klimstra D et al (2003) Is extended resection for adenocarcinoma of the body or tail of the pancreas justified? J Gastrointest Surg 7:946–952 discussion 952
Kimura W, Han I, Furukawa Y et al (1997) Appleby operation for carcinoma of the body and tail of the pancreas. Hepatogastroenterology 44:387–393
Yeo CJ, Cameron JL, Lillemoe KD et al (1995) Pancreaticoduodenectomy for cancer of the head of the pancreas. 201 patients. Ann Surg 221:721–731 discussion 731–723
Bradley EL 3rd (2008) Long-term survival after pancreatoduodenectomy for ductal adenocarcinoma: the emperor has no clothes? Pancreas 37:349–351
Sasson AR, Hoffman JP, Ross EA et al (2002) En bloc resection for locally advanced cancer of the pancreas: is it worthwhile? J Gastrointest Surg 6:147–157 discussion 157–148
Lim JE, Chien MW, Earle CC (2003) Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Ann Surg 237:74–85
Shimada K, Sakamoto Y, Nara S et al (2010) Analysis of 5-year survivors after a macroscopic curative pancreatectomy for invasive ductal adenocarcinoma. World J Surg 34:1908–1915. doi:10.1007/s00268-010-0570-9
Brennan MF, Moccia RD, Klimstra D (1996) Management of adenocarcinoma of the body and tail of the pancreas. Ann Surg 223:506–511 discussion 511–512
Kang CM, Kim DH, Lee WJ (2010) Ten years of experience with resection of left-sided pancreatic ductal adenocarcinoma: evolution and initial experience to a laparoscopic approach. Surg Endosc 24:1533–1541
Yamamoto J, Saiura A, Koga R et al (2010) Improved survival of left-sided pancreas cancer after surgery. Jpn J Clin Oncol 40:530–536
You DD, Lee HG, Heo JS et al (2009) Prognostic factors and adjuvant chemoradiation therapy after pancreaticoduodenectomy for pancreatic adenocarcinoma. J Gastrointest Surg 13:1699–1706
Neoptolemos JP, Dunn JA, Stocken DD et al (2001) Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet 358:1576–1585
Klinkenbijl JH, Jeekel J, Sahmoud T et al (1999) Adjuvant radiotherapy and 5-fluorouracil after curative resection of cancer of the pancreas and periampullary region: phase III trial of the EORTC gastrointestinal tract cancer cooperative group. Ann Surg 230:776–782 discussion 782–774
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs. Hyo Jun Park and Dong Do You are equally contributed to this work.
Rights and permissions
About this article
Cite this article
Park, H.J., Do You, D., Choi, D.W. et al. Role of Radical Antegrade Modular Pancreatosplenectomy for Adenocarcinoma of the Body and Tail of the Pancreas. World J Surg 38, 186–193 (2014). https://doi.org/10.1007/s00268-013-2254-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2254-8