Abstract
Background
Clinical outcome after unplanned extubation (UE) in patients admitted to the surgical intensive care unit (SICU) has not been fully investigated. In this study we assessed in-hospital mortality of patients with UE and determined whether UE is a predictor of in-hospital mortality. Finally, we sought to identify predictors of reintubation after UE in mechanically ventilated patients in the SICU.
Methods
Medical charts of patients (n = 4,407) admitted to the SICU between October 2007 and December 2011 were reviewed retrospectively.
Results
Eighty-five episodes of UE occurred in 81 patients. Patients with UE required emergency surgery more frequently and had higher ICU and hospital mortality rates, reintubation rate, and APACHE II scores and longer mechanical ventilation (MV) and ICU stay than patients without UE (P < 0.05 for all associations). Multivariate analysis revealed that reintubation (odds ratio [95 % confidence interval]: 4.14 [2.58–6.67]; P < 0.001), APACHE II scores (1.14 [1.12–1.17]; P < 0.001), emergency surgery (1.73 [1.18–2.53]; P = 0.005), and chronic neurologic disease (2.11 [1.30–3.41]; P = 0.002) were associated with hospital mortality. Reintubation was necessary in 17 patients. On multivariate analysis, a score on the Richmond Agitation–Sedation Scale (RASS, 0.48 [0.31–0.76]; P = 0.001), PaO2/FiO2 ratio (0.99 [0.99–1.00]; P = 0.048), and MV duration before UE (1.46 [1.08–1.98]; P = 0.014) were independently associated with reintubation after UE.
Conclusions
Our results indicated that although patients with UE had high in-hospital mortality, UE was not directly associated with in-hospital mortality. Reintubation, chronic neurologic disease, emergency operation, and higher APACHE II score were related to increased in-hospital mortality. A low RASS score, a low PaO2/FiO2 ratio, and long MV duration before UE were related to reintubation after UE.
Similar content being viewed by others
Introduction
Unplanned endotracheal extubation (UE) is a serious adverse event in the intensive care unit (ICU), the incidence of which has been reported to be 0.7–15.9 % [1, 2]. UE can result in life-threatening complications such as arterial hypoxemia and respiratory insufficiency. UE also increases the need for mechanical ventilation (MV) and ICU care [3]. With respect to clinical outcomes, UE is not necessarily associated with increased ICU or in-hospital mortality rates [3–6]. However, most of the cited studies were conducted in medical or mixed ICUs, few were conducted in surgical ICUs, and hospital mortality rates in patients with UE and those without UE were not compared [7–9].
Reintubation can often lead to hemodynamic and airway complications [10]. Furthermore, patients requiring reintubation have been reported to have higher mortality and morbidity rates [2, 11]. Thus, it is important to identify factors predictive of the need for reintubation in patients with UE. Although previous reports showed that pneumonia, age, and the amount of ventilatory support were significantly associated with reintubation after UE [4, 12, 13], factors predicting reintubation after UE are not well established, especially in surgical populations, because of insufficient data.
We hypothesized that in-hospital mortality is higher in patients with UE than in those without UE, and UE is associated with in-hospital mortality. In this study we assessed the in-hospital mortality of mechanically ventilated patients with UE in a tertiary-care surgical ICU and determined whether UE is a predictor of in-hospital mortality. Finally, we sought to identify predictors for reintubation after UE.
Methods
Study design and setting
After approval by the human studies committee, a retrospective exploratory design was used. The study was carried out on patients in a tertiary-care surgical intensive care unit (SICU) that consisted of up to 32 beds (October 2007–December 2008, 24 beds; January–July 2009, 28 beds; August 2009–December 2011, 32 beds), and who were operated on with an open system. The ICU was staffed by an intensive care specialist, an intensive care medicine fellow, and a senior anesthesia resident, who provided coverage during the daytime beginning in March 2008. Duty staffs or senior residents of each surgical department were in charge of the intensive care of their patients on nights and weekends. Nursing staff worked in three shifts: 8 am–4 pm, 4 pm–11 pm, and 11 pm–8 am, with a usual patient-to-nursing staff ratio of 2:1, and 1:1 in the case of severe critically ill patients.
Data collection
Electronic medical charts of patients admitted to the SICU between October 2007 and December 2011 were reviewed. Since March 2009, data were collected in a prospective fashion.
Two data sets were collected. One was used to compare clinical outcomes in patients with UE and those without UE and included demographics, emergent operation, acute physiology and chronic health care (APACHE) II score, the need for reintubation, MV duration, days in the ICU and length of hospital stay, ICU and in-hospital mortality rates, and postoperative complications. The other data set was used to identify predictors of reintubation after UE. The data consisted of Richmond Agitation–Sedation Scale (RASS) scores, MV duration before UE, history of sedation in the 2 h preceding UE, the use of physical restraints, nurse-to-patient ratio, the extent of MV support, the ability to communicate at the time of UE, and PaO2/FiO2 ratio (PF ratio) before UE.
Exclusion criteria
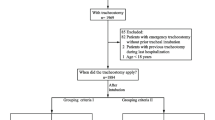
Patients with noninvasive positive-pressure ventilation (NIPPV) or without mechanical ventilation, aged younger than 18, and brain dead waiting for organ transplantation were excluded from the study. Post cardiac surgery patients were also excluded because they were admitted to a separate post cardiac surgical ICU. Medical patients admitted to the SICU due to lack of space in the MICU were also excluded. Patients with no extubation trial were excluded (Fig. 1). Patients admitted to the SICU from a general ward or the emergency room due to postoperative complications or events were also excluded to focus on immediate postoperative patients. If a patient experienced more than one episode of UE during the study period, only the first was included in the analysis.
Definitions
Accidental extubation was defined as the unintentional removal of an endotracheal tube by a health-care staff member. RASS score, as described previously [14], is as follows: +4 = combative, +3 = very agitated, +2 = agitated, +1 = restless, 0 = alert and calm, −1 = drowsy, −2 = light sedation, −3 = moderate sedation, −4 = deep sedation, and −5 = not able to be aroused.
Patients were considered to be in a weaning trial when there was a progressive reduction in respiratory rate or inspiratory pressure/volume from an initial MV setting or were placed on a T-piece. Conversely, patients were considered to be in full MV if a weaning trial was not begun.
Reintubation was defined as reinsertion of the endotracheal tube within 72 h after the UE. The usual criteria for reintubation were the development of increased signs of respiratory work, inability to protect the airway, persistent low SaO2 <90 % with FiO2 ≥50 %, or severe arterial blood gas deterioration. If NIPPV was applied in the postextubation phase, reintubation was needed in patients with NIPPV failure.
Statistical analysis
For continuous variables, values were compared using Student’s t test for independent samples. Differences in proportions were compared using the Chi square or Fisher’s exact test when the cell size was small. To determine independent risk factors for hospital mortality and reintubation after UE, the univariate logistic regression method was used to screen for significant risk factors, then risk factors with P < 0.20 in univariate analysis were entered into stepwise forward binary logistic regression. All tests were two-tailed and P < 0.05 was considered to indicate statistical significance.
Results
A total of 10,551 patients were admitted to the SICU during the study period (Fig. 1). Of them, 5,300 patients received MV, of which 893 patients were excluded (Fig. 1). Finally, 4,407 immediate postoperative patients were included in the data analysis.
Eighty-five episodes of UE (3 accidental extubation and 82 self-extubation) occurred in 81 patients. Two episodes of UE occurred in two patients and three episodes of UE occurred in one patient. The incidence of UE was 1.41 per 100 ventilated days.
Patients with UE had more frequent initial emergent surgery, higher ICU and in-hospital mortality rates, a higher reintubation rate, and a more prolonged MV duration and ICU stay than patients without UE (Table 1). The incidence of respiratory, renal, and neurologic complications during the ICU stay was higher in patients with UE.
On univariate analysis, UE, reintubation, initial emergency surgery, high APACHE II score, chronic neurologic and cardiac diseases, and older age were related to in-hospital mortality (Table 2). On multivariate analysis, reintubation (odds ratio [OR] 4.14; 95 % confidence interval [CI] 2.58–6.67; P < 0.001), high APACHE II score (OR 1.14; 95 % CI 1.12–1.17; P < 0.001), initial emergency surgery (OR 1.73; 95 % CI 1.18–2.53; P = 0.005), and chronic neurologic disease (OR 2.11; 95 % CI 1.30–3.41; P = 0.002) were associated with in-hospital mortality (Table 3).
Of the 81 patients with UE, NIPPV was applied in 3 patients in the postextubation phase. One patient required reintubation because of NIPPV failure due to facial mask intolerance, and two patients did not require reintubation because of NIPPV success. Finally, reintubation was necessary in 17 patients. Compared with UE patients without reintubation, UE patients with reintubation had more initial emergent surgery, higher tracheostomy and in-hospital mortality rates, and longer MV and ICU stays (Table 4). UE patients with reintubation had a higher incidence of pneumonia within 3 days of postextubation.
Of the 81 patients with UE, 7 received sedatives (5 had midazolam, 2 had propofol + fentanyl) 2 h before UE. Daily sedation interruption was used in five patients and light sedation was maintained in two patients. The reintubation rate was higher in patients with initial emergency surgery, lower RASS score and PF ratio, a weaning trial from MV, and long MV duration before UE (Table 5). On multivariate logistic regression, a low PF ratio (OR 0.99; 95 % CI 0.99–1.00; P = 0.048) and RASS score (OR 0.48; 95 % CI 0.31–0.76; P = 0.001) and long MV duration before extubation (OR 1.46; 95 % CI 1.08–1.98; P = 0.014) were associated with reintubation after UE (Table 6).
Discussion
The major findings of this study were as follows: (1) UE was associated with increased ICU and in-hospital mortality rates, more frequent postoperative complications, and more prolonged MV duration and ICU stays compared to no UE. (2) UE patients who required reintubation had significantly higher in-hospital mortality, longer ICU and hospital stays, and more prolonged MV duration than patients who remained extubated after UE. (3) The PaO2/FiO2 ratio before UE, the RASS, and MV duration before UE were associated with reintubation after UE.
This study is the first to compare clinical outcomes in surgical ICU populations, including ICU and in-hospital mortality rates, between patients with UE and those without. Interestingly, our findings suggest that ICU and in-hospital mortality rates were higher in patients with UE than in those without UE. This is inconsistent with the results of previous studies in which the ICU and in-hospital mortality rates of patients with UE and those without were comparable in mixed-patient populations [5, 15]. Moreover, other studies demonstrated that patients with UE, compared with patients without UE, had a lower mortality rate in mixed-patient populations [3, 4, 6, 13]. In contrast, a recent study of medical ICU patients reported higher ICU mortality in patients with UE than in those with planned extubation [11]. Such discrepancies in ICU/in-hospital mortality can, in part, be explained by differences in the study populations.
With respect to in-hospital mortality, this study showed that reintubation, a high APACHE II score, emergency surgery, and chronic neurologic disease were independent risk factors. UE was a predictor of in-hospital mortality in univariate analysis but it was not associated with in-hospital mortality after adjusting for confounding factors. However, in this study, patients with UE, compared with those without UE, were sicker and had more frequent emergency surgery and reintubation, which contribute to unfavorable clinical outcomes. Such findings suggest that although UE is not directly related to in-hospital mortality, UE can affect in-hospital mortality by increasing other risk factors associated with it.
Various factors, including a lower sedation level, use of restraints, orotracheal intubation, insufficient endotracheal tube fixation, and higher tube position relative to the carina, have been reported as risk factors for UE [2, 8, 11, 16–18]. In this study, we did not focus on identification of risk factors for UE. However, interestingly, we showed that the proportion of emergency surgery was significantly higher in patients with UE than in those without UE. A possible reason for this is that in our hospital, a detailed explanation of ICU circumstances, especially the need for postoperative ventilatory support and a warning regarding UE, was given to all patients with planned ICU admissions on the day before surgery, whereas a full explanation likely was not given to those admitted to the ICU unexpectedly. A further study is needed to verify the association of emergency surgery with UE.
Our findings indicate that among the patients with UE, those who required reintubation had a significantly higher in-hospital mortality rate and prolonged MV duration than patients who remained extubated after UE. This agrees with the results of previous studies in which ICU and in-hospital mortality rates were significantly higher in patients with reintubation than in those without reintubation after UE [2, 4, 9, 19]. A recent study reported that reintubation after UE can cause pronounced clinical deterioration by worsening the sequential organ failure assessment scores for 72 h after UE [11]. Our results also suggested an increased risk of developing respiratory complications, especially pneumonia within 3 days after UE, in reintubated patients. In agreement with our result, a previous study [4] reported that the rate of ICU-acquired infections such as ventilator-associated pneumonia was higher in UE patients with reintubation than those without.
In this study, the reintubation rate after UE was about 21 %. This is lower than that reported previously in surgical ICU patients in which the reintubation rate after UE was 36–58 % [7–9]. Various factors, including male gender, APACHE II score of 17 or greater, chronic obstructive pulmonary disease, restlessness/agitation, lower sedation level, higher consciousness level, and use of physical restraints, have been reported as predictors of reintubation after UE [20]. Our data suggest that MV duration before UE was an independent risk factor of reintubation after UE. In this study, 73 % of UE occurred within the first day of MV. This is consistent with a previous report in which 50 % of UE occurred among patients due to be extubated electively in the next few hours [1]. Such results suggest that most of the events are preventable, and staff vigilance and a concern about early extubation are necessary, especially in surgical populations. Some studies reported that reintubation after UE was associated with higher FiO2 or low PaO2/FiO2 before UE [2, 9, 19, 21]. Consistent with these, our results showed that reintubation after UE was observed more frequently in patients with low PaO2/FiO2. We showed that the RASS score was one of the risk factors associated with reintubation after UE. The frequency of reintubation after UE was higher in patients with a negative RASS score. This is supported by a study in which patients who needed reintubation had higher mean Ramsay scores than those who did not [8]. Although the sedation scale used was different, such findings suggest that deep sedation is associated with reintubation after UE. Bouza et al. [3] reported that reintubated patients showed a significant trend toward sedation under full MV. As seen in our results, because reintubation after UE was significantly associated with increased in-hospital mortality and prolonged MV duration, it is the best strategy to avoid UE if possible. Therefore, great attention should be paid to prevent UE in patients with risk factors of reintubation.
This study has some limitations. It was conducted retrospectively at a single center. Additionally, the small sample size may affect the ability to detect significant findings in some instances. Also, we analyzed the data on immediate postoperative patients admitted to a surgical ICU. The type and location of the facility in which the study was conducted may limit the generalizability of the results.
In conclusion, in surgical ICU patients, patients with UE had a higher in-hospital mortality rate. However, reintubation, chronic neurologic disease, emergency surgery, and higher APACHE II score rather than UE were related to increased in-hospital mortality. Because reintubation after UE is associated with unfavorable clinical outcomes, special attention is given to patients with a low RASS score, a low PaO2/FiO2 ratio, and long MV duration to prevent reintubation after UE.
References
Kapadia FN, Bajan KB, Raje KV (2000) Airway accidents in intubated intensive care unit patients: an epidemiological study. Crit Care Med 28:659–664
Chevron V, Menard JF, Richard JC et al (1998) Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 26:1049–1053
Bouza C, Garcia E, Diaz M et al (2007) Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung 36:270–276
Krinsley JS, Barone JE (2005) The drive to survive: unplanned extubation in the ICU. Chest 128:560–566
Epstein SK, Nevins ML, Chung J (2000) Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med 161:1912–1916
de Groot RI, Dekkers OM, Herold IH et al (2011) Risk factors and outcomes after unplanned extubations on the ICU: a case–control study. Crit Care 15:R19
Christie JM, Dethlefsen M, Cane RD (1996) Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 8:289–293
Curry K, Cobb S, Kutash M et al (2008) Characteristics associated with unplanned extubations in a surgical intensive care unit. Am J Crit Care 17:45–51
Razek T, Gracias V, Sullivan D et al (2000) Assessing the need for reintubation: a prospective evaluation of unplanned endotracheal extubation. J Trauma 48:466–469
Mort TC (1998) Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg 86:1171–1176
Thille AW, Harrois A, Schortgen F et al (2011) Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med 39:2612–2618
Chen CZ, Chu YC, Lee CH et al (2002) Factors predicting reintubation after unplanned extubation. J Formos Med Assoc 101:542–546
Betbese AJ, Perez M, Bak E et al (1998) A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 26:1180–1186
Sessler CN, Gosnell MS, Grap MJ et al (2002) The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 166:1338–1344
de Lassence A, Alberti C, Azoulay E et al (2002) Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 97:148–156
Chang LY, Wang KW, Chao YF (2008) Influence of physical restraint on unplanned extubation of adult intensive care patients: a case–control study. Am J Crit Care 17:408–415 quiz 416
Boulain T (1998) Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Reanimateurs du Centre-Ouest. Am J Respir Crit Care Med 157:1131–1137
Tanios MA, Epstein SK, Livelo J et al (2010) Can we identify patients at high risk for unplanned extubation? A large-scale multidisciplinary survey. Respir Care 55:561–568
Phoa LL, Pek WY, Syap W et al (2002) Unplanned extubation: a local experience. Singapore Med J 43:504–508
da Silva PS, Fonseca MC (2012) Unplanned endotracheal extubations in the intensive care unit: systematic review, critical appraisal, and evidence-based recommendations. Anesth Analg 114:1003–1014
Whelan J, Simpson SQ, Levy H (1994) Unplanned extubation. Predictors of successful termination of mechanical ventilatory support. Chest 105:1808–1812
Acknowledgments
This study was solely supported by the Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, Seoul, Korea.
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JH., Lee, HC., Jeon, YT. et al. Clinical Outcomes After Unplanned Extubation in a Surgical Intensive Care Population. World J Surg 38, 203–210 (2014). https://doi.org/10.1007/s00268-013-2249-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2249-5