Abstract
Background
New strategies for selection and training of physicians are emerging. Previous studies have demonstrated a correlation between visual-spatial ability and visual working memory with surgical simulator performance. The aim of this study was to perform a detailed analysis on how these abilities are associated with metrics in simulator performance with different task content. The hypothesis is that the importance of visual-spatial ability and visual working memory varies with different task contents.
Methods
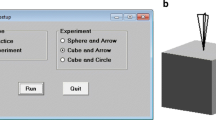
Twenty-five medical students participated in the study that involved testing visual-spatial ability using the MRT-A test and visual working memory using the RoboMemo computer program. Subjects were also trained and tested for performance in three different surgical simulators. The scores from the psychometric tests and the performance metrics were then correlated using multivariate analysis.
Results
MRT-A score correlated significantly with the performance metrics Efficiency of screening (p = 0.006) and Total time (p = 0.01) in the GI Mentor II task and Total score (p = 0.02) in the MIST-VR simulator task. In the Uro Mentor task, both the MRT-A score and the visual working memory 3-D cube test score as presented in the RoboMemo program (p = 0.02) correlated with Total score (p = 0.004).
Conclusions
In this study we have shown that some differences exist regarding the impact of visual abilities and task content on simulator performance. When designing future cognitive training programs and testing regimes, one might have to consider that the design must be adjusted in accordance with the specific surgical task to be trained in mind.

Similar content being viewed by others
References
Paice AG, Aggarwal R, Darzi A (2010) Safety in surgery: is selection the missing link? World J Surg 34(9):1993–2000
Sturm LP, Windsor JA, Cosman PH et al (2008) A systematic review of skills transfer after surgical simulation training. Ann Surg 248:166–1792
Gurusamy KS, Aggarwal R, Palanivelu L et al (2009) Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 1:CD006575
Grantcharov TP (2008) Is virtual reality simulation an effective training method in surgery? Nat Clin Pract Gastroenterol Hepatol 5:232–233
Enochsson L, Isaksson B, Tour R et al (2004) Visuospatial skills and computer game experience influence the performance of virtual endoscopy. J Gastrointest Surg 8:876–882 discussion 882
Hedman L, Strom P, Andersson P et al (2006) High-level visual-spatial ability for novices correlates with performance in a visual-spatial complex surgical simulator task. Surg Endosc 20:1275–1280
Strom P, Kjellin A, Hedman L et al (2004) Training in tasks with different visual-spatial components does not improve virtual arthroscopy performance. Surg Endosc 18:115–120
Baddeley AD (2001) Is working memory still working? Am Psychol 56:851–864
Hedman L, Klingberg T, Enochsson L et al (2007) Visual working memory influences the performance in virtual image-guided surgical intervention. Surg Endosc 21:2044–2050
Van Herzeele I, Aggarwal R, Neequaye S et al (2008) Cognitive training improves clinically relevant outcomes during simulated endovascular procedures. J Vasc Surg 48:1223–1230 1230 e1221
Peters M, Laeng B, Latham K et al (2000) A redrawn Vanderberg and Kuse mental rotation test: different versions and factors that affect performance. Brain Cogn 28:39–58
Klingberg T, Fernell E, Olesen PJ et al (2005) Computerized training of working memory in children with ADHD - a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry 44:177–186
Cushieri A, Francis N, Crosby J et al (2001) What do master surgeons think of surgical competence and revalidation? Am J Surg 182:110–116
Ringsted C, Skaarup AM, Henriksen AH et al (2006) Person-task-context: a model for designing curriculum and in-training assessment in postgraduate education. Med Teach 28:70–76
Sedlack RE, Kolars JC (2004) Computer simulator training enhances the competency of gastroenterology fellows at colonoscopy: results of a pilot study. Am J Gastroenterol 99:33–37
Park J, MacRae H, Musselman LJ et al (2007) Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg 194:205–211
Schlickum MK, Hedman L, Enochsson L et al (2009) Systematic video game training in surgical novices improves performance in virtual reality endoscopic surgical simulators: a prospective randomized study. World J Surg 33:2360–2367
Acknowledgments
This study was fully supported by unrestricted research grants from the Karolinska Institutet and the Marianne and Marcus Wallenberg Foundation. We gratefully acknowledge Torkel Klingberg for providing RoboMemo and Per Näsman for his excellent and valuable statistical assistance.
Disclosures
Drs. Schlickum, Hedman, Enochsson, Henningsohn, Kjellin, and Felländer-Tsai have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlickum, M., Hedman, L., Enochsson, L. et al. Surgical Simulation Tasks Challenge Visual Working Memory and Visual-Spatial Ability Differently. World J Surg 35, 710–715 (2011). https://doi.org/10.1007/s00268-011-0981-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-0981-2