Abstract
Background
Although the role of prophylactic central neck lymph node dissection (CNLD) in the treatment of papillary thyroid carcinoma (PTC) is controversial, many surgeons perform routine prophylactic CNLD. The present study compares local recurrence rates in PTC patients undergoing total thyroidectomy with and without prophylactic CNLD.
Materials and Methods
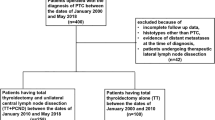
A retrospective review of 206 patients undergoing thyroidectomy for PTC was conducted at two tertiary referral centers. Of these, 81 patients had total thyroidectomy for PTC and a follow-up between 2 and 9 years with a mean of 3.1 years. Of these 81 patients, 45 underwent routine prophylactic CNLD and 36 did not. For those two groups, demographics, clinical and pathologic findings, radioactive iodine (RAI) treatment, and the incidence of recurrence were compared. Univariate statistical analysis was performed.
Results
There was no significant difference in age, gender, multifocality, or extrathyroidal extension for the two groups. Patients with CNLD had an average tumor size of 1.4 cm versus 2 cm in the group without CNLD (p < 0.05). Patients who underwent CNLD had an average of 8 nodes removed, and positive nodes were found in 33%. Patients with CNLD received a higher dose of RAI, 102.7 mCi versus 66.3 mCi (p < 0.05). The incidence of positive nodes correlated with an increased RAI dose (r = 0.55). Rates of parathyroid removal and autotransplantation were higher in the CNLD group, 36 and 16% in the CNLD group versus 22 and 3% in the group without CNLD (p = 0.4 and p = 0.07). Rates of temporary hypocalcemia were higher in the CNLD group (31 versus 5%; p = 0.001), however rates of permanent hypocalcemia were similar, 1/35 in the no CNLD group versus 0/45 in the CNLD group (p = 0.4). There was a higher recurrence rate among patients without CNLD 6/36 (16.7%) versus 2/45 (4.4%), although this difference was not statistically significant (p = 0.13).
Conclusions
Routine CNLD as an adjunct to total thyroidectomy identifies positive nodes in over 30% of patients with PTC. The discovery of positive nodes is associated with higher doses of RAI for postoperative ablation, and there is a trend toward decreased recurrence in patients undergoing CNLD.
Similar content being viewed by others
References
Rotstein L (2009) The role of lymphadenectomy in the management of papillary carcinoma of the thyroid. J Surg Oncol 99:186–188
Mazzaferri E, Jhiang S (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
DeGroot L, Kaplan E, McCormick M et al (1990) Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71:414–424
Sato N, Oyamatsu M, Koyama Y et al (1998) Do the level of nodal disease according to the TNM classification and the number of involved cervical nodes reflect prognosis in patients with differentiated carcinoma of the thyroid gland? J Surg Oncol 69:151–155
Scheumann G, Gimm O, Wegener G et al (1994) Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg 18:559–567 (discussion 567–558)
Shah J, Loree T, Dharker D et al (1992) Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg 164:658–661
Lundgren C, Hall P, Dickman P et al (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106:524–531
Tisell L, Nilsson B, Mölne J et al (1996) Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg 20:854–859
Cooper D, Doherty G, Haugen B et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Hughes C, Shaha A, Shah J et al (1996) Impact of lymph node metastasis in differentiated carcinoma of the thyroid: a matched-pair analysis. Head Neck 18:127–132
Sawka A, Brierley J, Tsang R et al (2008) An updated systematic review and commentary examining the effectiveness of radioactive iodine remnant ablation in well-differentiated thyroid cancer. Endocrinol Metab Clin North Am 37:457–480
White M, Gauger P, Doherty G (2007) Central lymph node dissection in differentiated thyroid cancer. World J Surg 31:895–904
Leboulleux S, Rubino C, Baudin E et al (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 90:5723–5729
Hay I, Bergstralh E, Grant C et al (1999) Impact of primary surgery on outcome in 300 patients with pathologic tumor-node-metastasis stage III papillary thyroid carcinoma treated at one institution from 1940 through 1989. Surgery 126:1173–1181 (discussion 1181–1172)
Bonnet S, Hartl D, Leboulleux S et al (2009) Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endocrinol Metab 94:1162–1167
Hackshaw A, Harmer C, Mallick U et al (2007) 131I activity for remnant ablation in patients with differentiated thyroid cancer: a systematic review. J Clin Endocrinol Metab 92:28–38
Dionigi G, Dionigi R, Bartalena L et al (2006) Surgery of lymph nodes in papillary thyroid cancer. Expert Rev Anticancer Ther 6:1217–1229
Palestini N, Borasi A, Cestino L et al (2008) Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbeck’s Arch Surg 393:693–698
Acknowledgment
The authors are grateful to Ben Umunna for his contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moo, TA., McGill, J., Allendorf, J. et al. Impact of Prophylactic Central Neck Lymph Node Dissection on Early Recurrence in Papillary Thyroid Carcinoma. World J Surg 34, 1187–1191 (2010). https://doi.org/10.1007/s00268-010-0418-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0418-3