Abstract
Background
Postoperative ileus, a common complication in patients after abdominal surgery, brings no benefit to the recovery of postoperative patients, and treatment targeted at restoring gastrointestinal motility may shorten the hospital stay. Studies have shown that escin accelerates gastrointestinal transit in mice and improves gastrointestinal motility in patients after abdominal surgery. A pilot study of escin’s effect on the recovery of gastrointestinal motility was conducted in colorectal cancer patients in anticipation of a multiple-center randomized controlled trial.
Methods
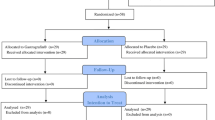
A total of 72 postoperative colorectal cancer patients were randomly assigned to four parallel groups on the basis of sealed envelopes—escin 5 mg group (E5 mg), escin 15 mg group (E15 mg), escin 25 mg group (E25 mg), and placebo group—with 18 patients in each group. Escin or placebo was diluted in 500 ml 5% dextrose injection, which was given once daily through the subclavian vein. The first injection took place 6 h after completion of the surgery. The treatment continued for 7 days or stopped at the time of the patient’s first bowel movement. Time to recovery of passage of gas (TRPG), time to recovery of gastrointestinal sounds (TRGS), and time to recovery of bowel movements (TRBM) were recorded to evaluate the efficacy of escin.
Results
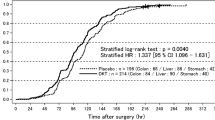
The TRPGs of the three escin treatment groups were 76.78 + 28.81 h (E5 mg), 72.06 + 14.65 h (E15 mg), and 65.50 + 26.70 h (E25 mg), respectively, with differences of 6.03 ± 7.64 h (p = 0.436; E5 mg), 10.75 ± 4.92 h (p = 0.036; E15 mg), and 17.31 ± 7.20 h (p = 0.022; E25 mg) compared with the placebo group. The TRGSs of the three escin treatment groups were 45.28 ± 26.15 h (E5 mg), 41.22 ± 16.98 h (E15 mg), and 40.33 ± 14.09 h (E25 mg), respectively, with differences of 4.33 ± 7.12 h (p = 0.547; E5 mg), 8.39 ± 5.36 h (p = 0.127; E15 mg), and 9.28 ± 4.87 h (p = 0.065; E25 mg) compared with the placebo group. The TRBMs of the three escin treatment groups were 89.25 ± 23.77 h (E5 mg), 84.83 ± 27.91 h (E15 mg), and 84.44 ± 19.74 h (E25 mg), respectively, with differences of 19.03 ± 10.13 h (p = 0.069; E5 mg), 23.44 ± 10.70 h (p = 0.035; E15 mg), and 23.83 ± 9.63 h (p = 0.019; E25 mg) compared with the placebo group.
Conclusion
The results of this pilot Postoperative Ileus Study of Escin (PISE) showed that escin can shorten the time to recovery of gastrointestinal motility in cancer patients after colorectal surgery.




Similar content being viewed by others
References
Holte K, Kehlet H (2000) Postoperative ileus: a preventable event. Br J Surg 87:1480–1493
Miedema BW, Johnson JO (2003) Methods for decreasing postoperative gut dysmotility. Lancet Oncol 4:365–372
Baig MK, Wexner SD (2004) Postoperative ileus: a review. Dis Colon Rectum 47:516–526
Guillaume M, Padioleau F (1994) Veinotonic effect, vascular protection, antiinflammatory and free radical scavenging properties of horse chestnut extract. Arzneimittelforschung 44:25–35
Liang DC, Yang HL (2004) A randomized controlled trial of escin in patients after surgery of lumber disc herniation. Chin J Spine Spinal Cord 40:617–618
Yan WC, Gao KS (2005) A randomized, controlled trial of escin for the treatment of acute cerebral infarction in senior patients. Chin J Gerontol 25:272–273
Dong GX, Wang ZG, Liang FQ et al (2003) The effect of escin on chronic venous insufficiency: a randomized controlled multi-centered clinical trial. Chin J Gen Surg 18:206–208
Matsuda H, Li Y, Yoshikawa M (2000) Possible involvement of dopamine and dopamine2 receptors in the inhibitions of gastric emptying by escin Ib in mice. Life Sci 67:2921–2927
Matsuda H, Li Y, Yoshikawa M (2000) Roles of endogenous prostaglandins and nitric oxide in inhibitions of gastric emptying and accelerations of gastrointestinal transit by escins Ia, Ib, IIa, and IIb in mice. Life Sci 66:PL41–PL46
Matsuda H, Li Y, Yoshikawa M (1999) Effects of escins Ia, Ib, IIa, and IIb from horse chestnuts on gastrointestinal transit and ileus in mice. Bioorg Med Chem 7:1737–1741
Matsuda H, Li Y, Yoshikawa M (2000) Possible involvement of 5-HT and 5-HT2 receptors in acceleration of gastrointestinal transit by escin Ib in mice. Life Sci 66:2233–2238
Fu FH, Hou YZ, Jiang WL et al (2005) Escin: inhibiting inflammation and promoting gastrointestinal transit to attenuate formation of postoperative adhesions. World J Surg 29:1614–1620
Hellerg K, Ruschewski W, De Vivie R (1975) Drug induced acute renal failure after heart surgery. Thoraxchirurgie 23:396–399
Holte K, Kehlet H (2000) Postoperative ileus: a preventable event. Br J Surg 87:1480–1493
Brown TA, McDonald J, Williard W (1999) A prospective, randomized, double-blinded, placebo-controlled trial of cisapride after colorectal surgery. Am J Surg 177:399–401
Lander A, Redkar R, Nicholls G et al (1997) Cisapride reduces neonatal postoperative ileus: randomized placebo controlled trial. Arch Dis Child 77:F119–F122
Cheatham ML, Chapman WC, Key SP et al (1995) A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg 221:469–476
Sagar PM, Kruegener G, MacFie J (1992) Nasogastric intubation and elective abdominal surgery. Br J Surg 79:1127–1131
Rao SS, Beaty J, Chamberlain M et al (1999) Effects of acute graded exercise on human colonic motility. Am J Physiol 276:G1221–G1226
Waldhausen JH, Schirmer BD (1990) The effect of ambulation on recovery from postoperative ileus. Ann Surg 212:671–677
Allen C, Glaszious P, Del Mar C (1999) Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet 354:1229–1233
Schilder JM, Hurteau JA, Look KY et al (1997) A prospective controlled trial of early postoperative oral intake following majaor abdominal gynecologic surgery. Gymecol Oncol 67:235–240
Stewart BT, Woods RJ, Collopy BT et al (1998) Early feeding after elective open colorectal resections:a prospective randomized trial. Aust N Z Surg 68:125–128
Helslin MJ, Latkany L, Leung D et al (1997) A prospective, randomized trial of early enteral feeding after resection of upper gastrointestinal malignancy. Ann Surg 226:567–577
Watters JM, Kirkpatrick SM, Norris SB (1997) Immediate postoperative enteral feeding results in impaired respiratory mechanics and decreased mobility. Ann Surg 226:369–377
Tonini M, De Ponti F, Di Nucci A et al (1999) Review article: cardiac adverse effects of gastrointestinal prokinetics. Aliment Pharmacol Ther 13:1585–1591
Bonacini M, Quiason S, Reynolds M et al (1993) Effect of intravenous erythromycin on postoperative ileus. Am J Gastroenterol 88:208–211
Wang MY, Li HC, Shi HP (1999) Experimental research on prevention of postoperative intestinal adhesion by sodium aescinate. Chin J Surg Integrated Traditional Western Med 5:382–384
Castedal M, Bjornsson E, Abrahamsson H (2000) Effects of midazolam on small bowel motility in humans. Aliment Pharmacol Ther 14:571–577
Wang SJ, Tsai SC, Lin WY et al (2000) A simple method for preparing radioactive capsules in colon transit study. Eur J Nucl Med 27:857–860
Altman DG, Bland JM (1995) Absence of evidence is not evidence of absence. BMJ 311:485
Shakespeare TP, Gebski VJ, Veness MJ et al (2001) Improving interpretation of clinical studies by use of confidence levels, clinical significance curves, and risk-benefit contours. Lancet 357:1349–1353
Li BH, Zhang J, Huang RZ et al (2006) Effect of pH adjustment of intravenous injection of sodium aescinate after addition of sodium bicarbonate to prevent phlebitis. Zhonghua Hu Li Za Zhi 41:113–115
Acknowledgments
The authors express their sincere gratitude to the participating investigators and their staff at the two study centers. The contributions of Dr. Peng Guo, Dr. Kai Shen, and Dr. Deepak Singh Mouni are much appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xie, Q., Zong, X., Ge, B. et al. Pilot Postoperative Ileus Study of Escin in Cancer Patients After Colorectal Surgery. World J Surg 33, 348–354 (2009). https://doi.org/10.1007/s00268-008-9816-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9816-1