Abstract
Background
Primary hyperparathyroidism (1° HPT) is reported most often in women over the age of 50. Beyond that, little is known about the epidemiology of this condition, and no studies have specifically examined the age and gender distribution of patients with 1° HPT.
Methods
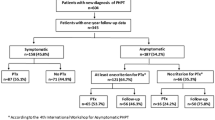
We analyzed patients from the Nationwide Inpatient Sample (NIS), a 20% random sample of all hospital stays from 2000–2004, and also from the University of Michigan endocrine surgery database from 1999–2005. Surgically treated 1° HPT was used as a surrogate marker for 1° HPT. An age- and sex-based frequency distribution was computed for each dataset.
Results
A total of 7,513 females and 2,677 males who underwent surgery for 1° HPT in the 5-year period 2000 through 2004 were reported in the NIS. At the University of Michigan from 1999 through 2005, 790 females and 276 males underwent parathyroidectomy for 1° HPT. In both datasets, the frequency of 1° HPT began to rise slowly in both sexes at age 11 and increased more rapidly among females than males beginning at age 21–25 (NIS) and 26–30 (UM). Incidence curves for both women and men in both databases were similar in shape and unipolar in configuration. Peak incidence was at age 56–60 (NIS) and 61–65 (UM) in females and age 56–60 in males (both datasets). The female:male ratio was noted to rise steadily among the NIS patients until perimenopausal age, after which it became stable for the next 20 years before decreasing again. No change in the female:male ratio over time was seen among the UM patients.
Conclusions
Primary HPT occurs more frequently in females than in males at all ages. The incidence increases steadily after age 25 in both sexes. The female:male ratio does not change during the peri- and postmenopausal years. This information should stimulate new hypotheses to explain the difference in the incidence of 1°HPT between men and women.


Similar content being viewed by others
References
Heath H III, Hodgson SF, Kennedy M (1980) Primary hyperparathyroidism: incidence, morbidity and potential economic impact in a community. N Engl J Med 302:189–193
Melton LJ III (1991) Epidemiology of primary hyperparathyroidism. J Bone Miner Res 6(Suppl 2):S25–S30
Wermers RA, Khosla S, Atkinson EJ (1997) The rise and fall of primary hyperparathyroidism: a population-based study in Rochester, Minnesota 1965–1992. Ann Intern Med 126:433–440
Melton LJ III (2002) The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res 17(Suppl 2):N12–17
Wermers RA, Khosla S, Atkinson EJ et al. (2006) Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993–2001: an update on the changing epidemiology of disease. J Bone Miner Res 21:171–177
Bilezikian JP, Silverberg SJ (2000) The clinical spectrum of primary hyperparathryoidism. Rev Endocr Metab Disord 1:237–245
Adami S, Marcocci C, Gatti D (2002) Epidemiology of hyperparathyroidism in Europe. J Bone Miner Res 17–2:N18–23
Ljunghall S, Hellman P, Rastad J et al. (1991) Primary hyperparathyroidism: epidemiology, diagnosis and clinical picture. World J Surg 15:681–687
Joborn C, Ljunghall S, Larsson K et al. (1991) Skeletal responsiveness to parathyroid hormone in healthy females: relationship to menopause and estrogen replacement. Clin Endocrinol 34:335
HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2000–2001. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/nisoverview.jsp
Wells G, Tugwell P, Shea B et al. (2002) Metaanalyses of therapies for postmenopausal osteoporosis. V. Meta-analysis of the efficacy of hormone replacement therapy in treating and preventing osteoporosis in postmenopausal women. Endocr Rev 23:529–539
Wong C, Lai T, Hilly JM et al. (2002) Selective estrogen receptor modulators inhibit the effects of insulin-like growth factors in hyperparathyroidism. Surgery 132:998–1006; discussion 1006–1007
Kort KC, Schiller HJ, Numann PJ (1999) Hyperparathyroidism and pregnancy. Am J Surg 177:66–68
Rastad J, Ekbom A, Hultin H et al. (2001) Childbearing and the risk of parathyroid adenoma—a dominant cause for primary hyperparathyroidism. J Intern Med 250:43–49
HCUP State Ambulatory Surgery Databases (SASD). Healthcare Cost and Utilization Project (HCUP). 2000–2004. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/sasdoverview.jsp
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, B.S., Dimick, J., Wainess, R. et al. Age- and Sex-Related Incidence of Surgically Treated Primary Hyperparathyroidism. World J Surg 32, 795–799 (2008). https://doi.org/10.1007/s00268-007-9427-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9427-2