Abstract
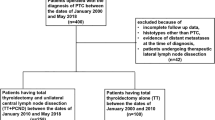
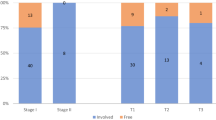
The indications for and extent of routine lymph node dissection in patients with papillary thyroid carcinoma (PTC) are unclear. The aim of this study was to investigate the association between the extent of central lymph node dissection (CLND) and the therapeutic effects and potential risks in patients with a small PTC. A total of 103 patients with a PTC <2 cm who underwent total thyroidectomy with routine CLND were divided into those who underwent routine bilateral CLND (group I) and those with ipsilateral CLND (group II). Therapeutic efficacy was evaluated by the extent of lymph node metastasis and postthyroidectomy serum thyroglobulin concentration. Patients with postoperative symptomatic hypocalcemia were considered to have postoperative hypoparathyroidism and received calcium/vitamin D therapy. Altogether, 12 of 21 patients (57.1%) in group I and 48 of 75 (64.0%) in group II had postthyroidectomy serum thyroglobulin concentrations <1.0 ng/ml; furthermore, 17 of 21 (81.0%) in group I and 60 of 75 (80.0%) in group II had concentrations <2.0 ng/ml. Hypocalcemia symptoms were identified in 12 of 25 patients (48.0%) in group I and in 16 of 78 (20.5%) in group II (p = 0.009). The extent of the CLND did not influence the therapeutic effects in patients with small PTCs, but those who underwent bilateral CLND showed an increased rate of transient hypoparathyroidism. These findings indicate that the more conservative routine CLND is as safe as more extensive CLND for patients with a small PTC.

Similar content being viewed by others
References
MacIver B, Hay ID (2001) Postoperative management of differentiated thyroid carcinoma. In: Doherty GM, Skogseid B (eds) Surgical Endocrinology. Lippincott Williams & Wilkins, Philadelphia, pp 87–108
Mazzaferri EL (1987) Papillary thyroid carcinoma: factors influencing prognosis and current therapy. Semin Oncol 14:315–332
Noguchi M, Kumoki T, Tariya T, et al. (1990) Bilateral cervical lymph node metastases in well differentiated thyroid cancer. Arch Surg 125:804–806
Scheumann GFW, Gimm O, Wegener O, et al. (1994) Prognostic significance and surgical management of loco regional lymph node metastases in papillary thyroid cancer. World J Surg 18:559–568
Simon D, Goretzki PE, Witte J, et al. (1996) Incidence of regional recurrence guiding radicality in differentiated thyroid carcinoma. World J Surg 20:860–866
Tisell LE, Nilsson B, Mölne J, et al. (1996) Improved survival of patients with papillary thyroid cancer after surgical micro dissection. World J Surg 20:854–859
Max MH, Scherm M, Bland KI (1983) Early and late complications after thyroid surgery. South Med J 76:977–980
Kim TY, Kim WB, Kim ES, et al. (2005) Serum thyroglobulin levels at the time of 131I remnant ablation just after thyroidectomy are useful for early prediction of clinical recurrence on low-risk patients with differentiated thyroid carcinoma. J Clin Endocrinol Metab 90:1440–1445
Frederick LG, David LP, Irvin DF, et al. (2002) AJCC Cancer Staging Manual. 6th edn. Springer-Verlag, New York, pp 77–87
Pereira JA, Jimeno J, Miguel J, et al. (2005) Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery 138:1095–1100
Noguchi S, Noguchi A, Murakami N (1970) Papillary carcinoma of the thyroid: developing pattern of metastases. Cancer 26:1053–1060
Noguchi S, Murakami N (1987) The value of lymph node dissection in patients with differentiated thyroid cancer. Surg Clin North Am 25:251–255
Hubert JP Jr, Kiernam PD, Beahrs OH (1980) Occult papillary carcinoma of the thyroid. Arch Surg 115:394–396
Hay ID, Grant CS, van Heerden JA (1992) Papillary thyroid microcarcinoma: a study of 535 cases observed in a 50-year period. Surgery 112:1139–1145
Hamming JF, Van de Velde CJH, Gosling CM, et al. (1985) Preoperative diagnosis and treatment of metastases to the regional lymph nodes in papillary carcinoma of the thyroid gland. Surg Gynecol Obstet 169:107–114
Rossi RC, Cady B, Silverman MC, et al. (1986) Current result of conservative surgery of differentiated thyroid carcinoma. World J Surg 10:612–622
Lundgren CI, Hall P, Dickman PW, et al. (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106:524–531
Hay ID (1990) Papillary thyroid carcinoma. Endocrinol Metab Clin North Am 19:545–551
McHenry CR, Rosen JB, Walfish PG (1991) Prospective management of nodal metastases in differentiated thyroid cancer. Am J Surg 162:353–356
Shah JP (1996) Cervical lymph nodes. Head and Neck Surgery. 2nd edn. Mosby-Wolfe, Barcelona, pp 355–392
Ito Y, Tomodo C, Uruno T, et al. (2006) Clinical significance of metastasis to the central compartment from papillary microcarcinoma of the thyroid. World J Surg 30:91–99
De Roy Van Zuidewijin DBW, Songun I, Kievit J, et al. (1995) Complications of thyroid surgery. Ann Surg Oncol 2:56–64
Harness JK, Fung L, Thompson NW, et al. (1986) Total thyroidectomy: complications and technique. World J Surg 10:781–786
Wingert DJ, Friesen SR, Iliopoulos JI, et al. (1986) Post-thyroidectomy hypocalcemia: incidence and risk factors. Am J Surg 152:606–610
Shara AR, Jaffe BM (1998) Parathyroid preservation during thyroid surgery. Am J Otolaryngol 19:113–117
McHenry CR, Speroff T, Wentworth D, et al. (1994) Risk factors for postthyroidectomy hypocalcemia. Surgery 116:641–647
Miller S (2004) Voice therapy for vocal fold paralysis. Otolaryngol Clin N Am 37:105–119
Bihari A, Meszaros K, Remenyi A, et al. (2006) Voice quality improvement after management of unilateral vocal cord paralysis with different techniques. Eur Arch Otorhinolaryngol 263:1115–1120
Crumley RL (1990) Repair of recurrent laryngeal nerve. Otolaryngol Clin N Am 23:553–563
O’Leary MA, Grillone GA (2006) Injection laryngoplasty. Otolaryngol Clin N Am 39:43–54
Hamdan AL, Mokarbei R, Dagher W (2004) Medialization laryngoplasty for the treatment of unilateral vocal cord paralysis: a perceptual, acoustic and stroboscopic evaluation. J Med Liban 52:136–141
Henry JF, Gramatica L, Denizot A, et al. (1998) Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg 383:167–169
Sywak M, Roach P, Stalberg P, et al. (2006) Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery 140:1000–1005
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, Y.S., Kim, S.W., Kim, S.W. et al. Extent of Routine Central Lymph Node Dissection With Small Papillary Thyroid Carcinoma. World J Surg 31, 1954–1959 (2007). https://doi.org/10.1007/s00268-007-9171-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9171-7