Abstract
Background
Heterogeneous antibiotic use has been suggested to limit the emergence of resistance, but determining the optimal strategy is difficult.
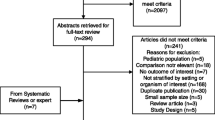
Methods
We developed a new strategy, termed “periodic antibiotic monitoring and supervision” (PAMS) program in a non-ICU surgical ward. The 2-year prospective study was divided into a 1-year observation period and a 1-year PAMS period. The use of four major classes of antibiotics in empirical therapy for Gram-negative rod (GNR) infections was supervised. During the PAMS program, recommended, restricted, and off-supervised classes of antibiotics were changed every 3 months according to the usage pattern of the antibiotics in the preceding term.
Results
Cefepime (45.5%) and imipenem/cilastatin (39.4%) were the most common antibiotics of choice during the observation period. The use of these antibiotics decreased significantly during the PAMS period, and that of fluoroquinolones and extended-spectrum penicillin/beta-lactamase inhibitor increased (4.8% vs. 21.4% and 2.4% vs. 21.4%, P < 0.01 respectively). Outcome analysis demonstrated a tendency toward reduction in the incidence of resistant GNR infections (P = 0.079) and that of Pseudomonas aeruginosa (P = 0.053). The incidence of resistant Gram-positive core infections did not decrease. Analysis of antibiotic susceptibility to GNR revealed no significant beneficial results for any antibiotics.
Conclusions
As significant changes were not observed, the PAMS program is not generally applicable and heterogeneous antibiotic use as a way of reducing infections with resistant GNR in non-ICU surgical wards was not established.


Similar content being viewed by others
References
Bukholm G, Tannaes T, Kjelsberg AB, et al. An outbreak of multidrug-resistant Pseudomonas aeruginosa associated with increased risk of patient death in an intensive care unit. Infect Control Hosp Epidemiol 2002;23:441–446
Cosgrove SE, Kaye KS, Eliopoulous GM, et al. Health and economic outcomes of the emergence of third-generation cephalosporin resistance in Enterobacter species. Arch Intern Med 2002;162:185–190
Kollef MH, Vlasnik J, Sharpless L, et al. Scheduled change of antibiotic classes; a strategy to decrease the incidence of ventilator-associated pneumonia. Am J Respir Crit Care Med 1997;156:1040–1048
Gruson D, Hilbert G, Vargas F, et al. Rotation and restricted use of antibiotics in a medical intensive care unit. Impact on the incidence of ventilator-associated pneumonia caused by antibiotic-resistant Gram-negative bacteria. Am J Respir Crit Care Med 2000;162:837–843
Raymond DP, Pelletier SJ, Crabtree TD, et al. Impact of a rotating empiric antibiotic schedule on infectious mortality in an intensive care unit. Crit Care Med 2001;29:1101–1108
Allegranzi B, Luzzati R, Luzzani A, et al. Impact of antibiotic changes in empirical therapy on antimicrobial resistance in intensive care unit-acquired infections. J Hosp Infect 2002;52:136–140
Gruson D, Hilbert G, Vargas F, et al. Strategy of antibiotic rotation: long-term effect on incidence and susceptibility of Gram-negative bacilli responsible for ventilator-associated pneumonia. Crit Care Med 2003;31:1908–1914
Gerding DN, Larson TA, Hughes RA, et al. Aminoglycosides resistance and aminoglycosides usage: ten years of experience in one hospital. Antimicrob Agents Chemother 1991;35:1284–1290
Kollef MH, Fraser VJ. Antibiotic resistance in the intensive care unit setting. Ann Intern Med 2001;134:298–314
Garner JS, Jarvis WR, Emori TG, et al. CDC definitions for nosocomial infections. Am J Infect Control 1988;16:128–140
ACCP/SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 1992;101:1644–1655
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; Fifteenth Informational Supplement M100-S12, NCCLS, Wayne, PA, 2002
Perez FJ, Gimeno C, Navarro D, et al. Meropenem permeation through the outer membrane of Pseudomonas aeruginosa can involve pathways other than the OprD porin channel. Chemotherapy 1996;42:210–214
Warren DK, Hill HA, Merz LR, et al. Cycling empirical antimicrobial agents to prevent emergence of antimicrobial-resistant Gram-negative bacteria among intensive care unit patients. Crit Care Med 2004;32:2450–2456
Evans HL, Milburn ML, Hughes MG, et al. Nature of gram-negative rod antibiotic resistance during antibiotic rotation. Surg Infect 2005;6:223–231
Ahmad M, Urban C, Mariano N, et al. Clinical characteristics and molecular epidemiology associated with imipenem-resistant Klebsiella pneumoniae. Clin Infect Dis 1999;29:352–355
Fridkin SK. Routine cycling of antimicrobial agents as an infection-control measure. Clin Infect Dis 2003;36:1438–1444
Acknowledgements
We thank Mr. Hideki Itaha and Mr. Makoto Onodera for the measurement of antibiotic susceptibility. This work was supported by Taisho Toyama Pharmaceutical Corporation Ltd. and Sumitomo Pharmaceuticals. There were no conflicts of interest in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takesue, Y., Ohge, H., Sakashita, M. et al. Effect of Antibiotic Heterogeneity on the Development of Infections with Antibiotic-resistant Gram-negative Organisms in a Non-intensive Care Unit Surgical Ward. World J. Surg. 30, 1269–1276 (2006). https://doi.org/10.1007/s00268-005-0781-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0781-7