Abstract
The purpose of the study was to investigate whether examination for plasma β-d-glucan, a cell wall constituent of fungi, is useful for selecting surgical patients with Candida colonization who would benefit from empiric antifungal therapy. We administered fluconazole to postoperative patients with Candida colonization who have risk factors for candidemia and complained of persistent fever despite prolonged antibacterial therapy. We then analyzed the clinical outcomes regarding the number of sites colonized with Candida spp. and plasma β-d-glucan. Of the 32 patients positive for β-d-glucan, 15 (46.9%) responded to the empiric therapy; only 9% of those who were negative responded (p < 0.01). In the multiple logistic regression analysis, being positive for β-d-glucan was a significant factor predicting response, with an adjusted odds ratio of 12.9 in patients with Candida colonization [95% confidence interval (CI) 2.07–80.73) (p < 0.01). In addition, the number of sites colonized with Candida spp. was a significant factor predicting response, with an estimated exposure odds ratio of 7.57 for those who were colonized at three or more sites compared with those colonized at one site (95% CI 1.20–47.70) (p = 0.031). In patients with Candida colonization, assessment of β-d-glucan was useful for deciding whether to start empiric therapy for suspected candidiasis in surgical patients.
Similar content being viewed by others
To improve the outcome of invasive Candida infections, early empiric therapy, before a definitive diagnosis is established, is considered necessary [1, 2, 3, 4]. However, appropriate use of empiric therapy for suspected candidiasis in febrile nonneutropenic surgical patients has not been defined [5, 6]. According to the guidelines from the Infectious Diseases Society of America, empiric therapy of suspected candidiasis in this setting should be limited to patients with Candida colonization at multiple sites, multiple other risk factors, and an absence of any other causes of fever [5]. Pittet et al. [2] showed that a corrected colonization index, which takes into account both the density and the degree of colonization of Candida spp. recovered from semiquantitative cultures, is an independent factor that predicts subsequent candidal infection.
It may also be appropriate to commence empiric therapy on the basis of a positive serodiagnostic test [6]. β-d-glucan is a cell wall constituent of fungi that is supposedly a marker of fungal sepsis [7, 8, 9, 10, 11, 12, 13]. However, it has been shown that β-d-glucan can also be detected in patients without fungal infections [14, 15, 16, 17] (e.g., those on hemodialysis), and its positive predictive value is relatively low. The utilization of β-d-glucan alone to determine if fungal infection is present should therefore be avoided.
The aim of this study was to investigate whether an examination to determine the extent of Candida colonization combined with a plasma β-D-glucan assay are useful for selecting surgical patients who would benefit from empiric therapy with fluconazole before serious invasive Candida infection develops.
Patients and Methods
Patients
Inclusion criteria were as follows: subjects had undergone surgery within 2 months, subjects demonstrated colonization with Candida spp. before enrollment, subjects had risk factors for Candida infection, and subjects complained of persistent fever despite treatment with three or more antibacterial drugs or a fever duration of more than 7 days [18]. Fever was defined as either three oral-equivalent temperature elevations above 38.0°C during a 24-hour period or a single oral-equivalent temperature elevation to 38.3°C or higher. Risk factors for Candida infection were central venous nutrition, arterial line (> 7 days), artificial ventilatory assistance, Foley catheter (> 7 days), steroid therapy, multiple blood transfusion, stay in the intensive care unit (ICU) of more than 7 days, and hemodialysis [18, 19]. Dialyzers with polymethylmethacrylate, which does not cause a false-positive reaction of the β-D-glucan test [14], were used for hemodialysis.
Patients were excluded for the following reasons: a documented deeply invasive fungal infection, use of antifungal agents within 1 month before enrollment, use of antitumor polysaccharides [17], pregnancy, age younger than 12 years, a history of allergy or anaphylaxis to azole antifungal agents, neutrophil counts < 500/mm3, or a life expectancy of less than 72 hours.
The study was a prospective, multicenter trial conducted between January 15, 1999 and April 7, 2002. The participating centers were Hiroshima University Hospital, Hiroshima General Hospital, Hiroshima Memorial Hospital, Kure Mutual Aid Hospital, and Miyushi Central Hospital. All centers were similar with regard to the kind of surgery and surgical ICU availability. Before the study began, the details were explained to all subjects, and written informed consent was obtained. The study protocol was approved by an institutional review board or ethics committee at each of the five participating centers.
Intervention
As empiric therapy, fluconazole was administered intravenously at a daily dose of 400 mg. If the body weight was less than 50 kg, the daily dose was reduced to 200 mg. The patients continued to receive antifungal therapy for at least 7 days, and antibacterial agents administered immediately preceding enrollment were continued. Patients who underwent additional modalities of treatment such as drainage of an intraabdominal abscess, removal of a central venous line, or débridement of necrotic tissue during antifungal treatment were excluded from the analysis.
Before starting treatment, the plasma concentration of β-d-glucan was measured and, when possible, surveillance fungal cultures were prepared to determine the extent of colonization. Samples were obtained from the oropharynx, rectum, exudates from drainage material, bile, urine, and gastric aspirate (at least three sites) on the day of enrollment in the study. In patients with positive plasma β-d-glucan tests, serologic changes were assessed at the end of therapy.
Clinical Response
Patients were evaluated daily for vital signs, temperature, and symptoms of infection. In addition, the absolute neutrophil count and the plasma C-reactive protein (CRP) level were measured at least twice weekly during the treatment. Physical examination was performed frequently, and in patients with radiographic abnormalities a radiographic examination was performed at least once a week.
The clinical response to treatment was assessed at the end of therapy. The endpoint of therapy in this study was defervescence and normalized neutrophil counts and CRp values. We defined the clinical response based on criteria that had been validated in other studies of empiric antifungal therapy [20, 21, 22, 23, 24, 25].
Clinical response was categorized as one of the following four possible outcomes. A complete response was defined as a return to the afebrile state (oral-equivalent temperature of ≤ 37.6°C) within 1 week of fluconazole administration, with continuation of that response for at least 72 hours in the absence of any changes in antibacterial or antipyretic therapy. In addition to the patient’s temperature, we confirmed the resolution of all attributable symptoms, signs, or radiographic abnormalities present at the time of enrollment. A partial response was defined as a minimum of 3 consecutive days with fever (oral-equivalent temperature < 38.0°C) within 1 week of administration of fluconazole accompanied by an improvement in the absolute neutrophil count or plasma CRp value. Moreover, the patient’s symptoms and radiographic abnormalities that had been present at the time of enrollment were diminished. Stable disease was defined as minor or no improvement regarding symptoms, signs, or radiographic abnormalities after 7 days or more of therapy; these subjects continued on therapy without deterioration. Worsened condition was defined as deterioration in the symptoms, signs, and radiographic abnormalities necessitating alternative therapy or resulting in death.
A clinical response assessed as complete or partial was categorized as a successful intervention, and that assessed as stable disease or worsened condition was categorized as a failed intervention. Breakthrough fungal infection after the completion of therapy was not defined as a failure if the clinical response had been assessed as complete or partial at the end of therapy. The clinical response rate was analyzed from the number of nonblood, distinct body sites colonized by Candida spp. and the results of the plasma β-d-glucan assay.
Serologic Response
In patients positive for β-d-glucan, the serologic response was categorized as follows: normalized, return to normal values; improved, remained positive but with a clinically significant decrease compared to that at the time of enrollment in the study; unchanged, no clinically significant decrease from the time of enrollment; worsened, clinically significant increase compared to that at the time of enrollment. Patients assessed as normalized or improved were categorized as serologic responders.
Method for Detecting β-d-Glucan
(1→3)-β-d-Glucan is a major structural component of the fungal cell wall and has been reported to react with factor G, a coagulation enzyme of the Limulus amebocyte lysate. [17] The Limulus amebocyte lysate is composed of two coagulation pathways, as demonstrated by fractionation analysis [7]. The first pathway contains factors B and C, which are sensitive to endotoxin, whereas the second pathway contains factor G, which is sensitive to (1→3)-β-d-glucan. The Fungitec G test (Seikagaku Kogyo, Tokyo, Japan) is specific to (1→3)-β-d-glucan, as factors B and C are eliminated in the test [7]. Factor G is activated by (1→3)-β-d-glucan, leading to activation of the proclotting enzyme. In this test, the chromogenic substrate Boc-Leu-Gly-Arg-p-nitroanilide is cleaved by the activated clotting enzyme, followed by the release of p-nitroanilide. The released p-nitroanilide is determined at an absorbance at 405 nm.
A 5.0 μl plasma sample was pretreated with 20 μ l of the test solution containing 0.15 M KOH, 0.3 M KCl, and 0.1% polybrene; the mixture was then incubated for 10 minutes at 37°C. The pretreated sample was added to 100 μ l of factor G dissolved in HEPES buffer (0.1 M, ph 7.6) and incubated at 37°C for 30 minutes. The optical density at 405 nm was measured using the kinetic mode of a computerized well-reader (SK601; Seikagaku Kogyo). Pachyman, (1→3)-β-d-glucan from Poria cocos, was used as a standard. The coefficient of variation in the fungitec G test was < 5%. The time required to achieve the test result was 120 minutes, and the cost of the β-d-glucan test was 2900 Japanese yen. Duplicate assays were performed on each sample, and the average of the two tests was analyzed. The plasma cutoff value was 20 pg/ml [7].
Statistical Analysis
Baseline characteristics were compared between responders and nonresponders to the empiric therapy. Univariate comparisons of categorical variables were analyzed by Pearson’s χ2 test or Fisher’s exact test. Continuous variables were analyzed by Student’s t-test or analysis of variance. A value of p < 0.05 was considered significant on two-tailed testing. The clinical response rate was assessed according to the number of sites colonized with Candida spp. and the absence or presence of β-d-glucan. Multivariate analysis was done by stepwise logistic regression, and the limit for entering and removing variables was 0.2. Data were statistically analyzed using SPSS 10.0J (SPSS Japan, Tokyo, Japan).
Results
Patient Population
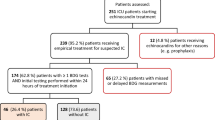
A total of 81 patients were enrolled in the study: 22 patients at Hiroshima University Hospital, 18 at Hiroshima General Hospital, 17 at Hiroshima Memorial Hospital, 13 at Kure Mutual Aid Hospital, and 11 at Miyoshi Central Hospital. Altogether, 64 patients were analyzed; 17 had been excluded from the analysis (4 patients did not meet the enrollment criteria). Plasma β-d-glucan was not measured by the Fungitec G test in three patients. In addition, four patients had proven fungal infection determined by cultures performed before enrollment. A central venous catheter was removed during antifungal thearapy in two patients. Three patients never received the study drug, and one patient died within 3 days after administration of fluconazole. There was no significant difference between responders and nonresponders to the empiric therapy with regard to the patients’ clinical characteristics, although the patient’s sex and the use of anticancer chemotherapy tended to be predictive of the response (Table 1).
Efficacy
Altogether, 11 patients responded completely, 7 responded partially, 39 had stable disease, and 7 had a worsened condition. The overall clinical success rate was 28.1%. The clinical success rate was 22.7% at Hiroshima University Hospital, 33.3% at Hiroshima General Hospital, 11.8% at Hiroshima Memorial Hospital, 23.1% at Kure Mutual Aid Hospital, and 18.2% at Miyushi Central Hospital. Thus there were no significant differences among participating centers.
Of the 26 patients positive for β-d-glucan, 16 responded serologically to empiric therapy (normalized 6; improved 10). In 12 of 15 patients positive for β-d-glucan who exhibited a clinical response, the plasma β-d glucan value decreased compared to that at the time of enrollment. The suspected sites or sources of fungal infection in patients undergoing empiric therapy were the peritoneum in 21 patients, mediastinum in 3, urinary tract in 8, respiratory tract in 6, and the vascular catheter in 5; enterocolitis was seen in 2 patients, and there was no obvious site in 19. One patient who had a positive clinical response had documented breakthrough fungal infections 12 days after the completion of treatment. Survival 1 month after the end of therapy was 76.1%. Of the 11 patients who died, 5 died of a progressive underlying neoplastic disease. Only 1 of 18 patients rated as a clinical success died compared to 10 of 46 patients with clinical failure; the difference was not significant (p = 0.159).
Isolated Candida spp. by Surveillance Culture
A total of 116 isolates were obtained from 46 patients. Among these isolates, 34 organisms were isolated from the oropharynx or trachea, 28 from rectum, 12 from surgical wounds, 21 from the peritoneum, 13 from urine, 5 from gastric aspirates, and 3 from bile. The Candida spp. isolated during screening included 49 strains of C. albicans, 26 strains of C. glabrata, 7 strains of C. tropicalis, 4 strains of C. parapsilosis, 1 strain of C. krusei, and 2 strains of other Candida spp. C. albicans and non-albicans Candida spp. were isolated simultaneously in 16 patients, and neither species’ colonization was significantly predictive of the response. In the analysis of exclusive isolation, only 2 of 13 patients colonized with non-albicans Candida spp. responded to treatment, whereas 11 of 33 patients colonized with C. albicans did respond.
Clinical Response from the Sites Colonized by Candida spp. and Results of the Plasma β-d-Glucan Test
A total of 209 body sites were tested (3.27 ± 0.51/patient, range 3–5/patient). The nonblood distinct body sites that screened positive for Candida spp. included one site in 26 patients, two sites in 18 patients, and three or more sites in 20 patients. The response rate to empiric therapy was 11.5% in patients who were colonized at one site, 33.0% in patients colonized at two sites, and 45.0% in patients colonized at three or more sites. There was a significant correlation between the response rate and the number of sites colonized with Candida spp. (p = 0.037, correlation coefficient 0.321).
There was a significant difference in the plasma β-d-glucan levels between patients who showed a positive response to treatment and those who did not (105.0 ± 127.5 vs. 26.7 ± 51.1 pg/ml, p = 0.020). Using a plasma cutoff value of 20 pg/ml, 32 of 64 patients were positive for β-d-glucan. Of these 32 patients, 15 (46.9%) who were positive for β-d-glucan responded to empiric therapy, whereas only 9% of those who were negative for β-d-glucan did so (p < 0.01).
In the logistic regression analysis, subjects who were colonized at three or more sites were almost six times more likely to respond to treatment than those colonized at one site. Adjusting for the other factors in the patients, the number of sites colonized with Candida spp. was a significant factor predicting response, with an estimated exposure odds ratio of 7.57 for those who were colonized at three or more sites compared with those colonized at one site [95% confidence interval (CI) 1.20–47.70] (p = 0.031). In addition, being positive for β-d-glucan was a significant factor predicting response, with an estimated exposure adjusted odds ratio of 12.92 (95% CI 2.07–80.73) (p < 0.01) (Table 2).
Based on these results, colonization with Candida at three or more sites (rule A) and being positive for β-d-glucan (rule B) were significant predictors of the clinical response to antifungal therapy. With rule A, the positive predictive value (PPV) was estimated to be 45.0%, and the negative predictive value (NPV) was 79.5%. With rule B, the PPV was estimated to be 46.9% and the NPV 90.6%.
The clinical response based on the number of sites colonized with Candida spp. and the results of the plasma β-d-glucan assay were analyzed (Fig. 1). A high clinical response rate was observed (55.6% and 58.3%, respectively) in patients positive for β-d-glucan who were colonized at two sites and those colonized at three or more sites. Among these patients 3 of 11 (27.3%) positive for β-d-glucan who were colonized at one site and 2 of 8 (25.0%) negative for β-d-glucan who were colonized at three or more sites responded to empiric therapy. There were no responders among patients negative for β-d-glucan who were colonized at one site.
Discussion
With a better understanding of the predisposing factors for candidemia [4, 18, 19], interest now centers on indications for early therapy, prior to the progression to serious disseminated infection with Candida spp. Although early empiric therapy is intuitively attractive, compelling data defining appropriate subsets of patients for such therapy are lacking [5]. The British Society for Antimicrobial Chemotherapy Working Party [6] stated that Candida antigenemia may be suggestive of the disease, but the methods currently available do not yet provide definitive results. It may be appropriate to commence therapy on the basis of a positive Candida serologic test, but this is regarded as empiric therapy; rather, it is treatment for established disease.
β-d-Glucan is a major structural component of the fungal cell wall and has been reported to react with factor G, a coagulation enzyme of the Limulus amebocyte lysate [17]. The Fungitec G test, which uses factor G, has been shown to be useful for the early, rapid diagnosis of deep-seated Candida infection [7, 8, 9, 10, 11, 12, 13]. Obayashi et al. [7] demonstrated that the PPV was 59% and the NPV 97%. It has been reported that the Fungitec G test showed false-positive reactions in patients undergoing hemodialysis (because of the cellulose-based filter membrane [14]) and in those being treated with human immunoglobulin products, which may contain factor G-reactive materials [15]. Immunoactive β-d-glucans such as lentinan, sceeroglucan, and schizophyllan share a common β-d-(1→3)-linkage glucopyronosyl backbone, so patients undergoing treatment with antitumor polysaccharides may give false-positive results [17]. Moreover, immediately after surgery there is a transitory rise in glucan influenced by the use of gauze during surgery [26], which must be kept in mind. The amount of β-d-glucan in the blood is thought to be related to the amount of Candida spp. in the body but does not necessarily reflect the severity of the disease. [10] Accordingly, this method is best used in conjunction with other tests and clinical symptoms when making a diagnosis of fungal infection. The utilization of β-d-glucan alone for serologic tests of candidiasis should therefore be avoided [11]. The combined assessment of β-d-glucan and extent of colonization with Candida spp. is thought to have the advantage of decreasing the likelihood of a false-positive β-d-glucan reaction.
In the present study, we administered fluconazole as empiric therapy to postoperative patients with Candida colonization who had risk factors for candidemia and who complained of persistent fever despite prolonged antibacterial therapy. We then analyzed clinical outcomes from both the number of sites colonized by Candida spp. and the plasma β-d-glucan test. In a multiple logistic regression analysis, subjects who were colonized at three or more sites were almost 8-fold more likely to respond to treatment than those colonized at one site. In addition, subjects who had a positive β-d-glucan test were almost 13-fold more likely to respond to empiric therapy than those who were negative for β-d-glucan. In patients positive for β-d-glucan with Candida colonization, the PPV was estimated at 46.9% and the NPV at 90.6%. Based on these results, colonization at three or more sites with Candida spp. (rule A) and the presence of β-d-glucan in plasma (rule B) were considered to be significant predictors of the clinical response to antifungal empiric therapy in patients with Candida colonization.
Because we assessed suspected Candida infection from the response to fluconazole treatment, Candida infections that did not respond to fluconazole therapy seem to be overlooked in the analysis. Fluconazole is shown to be less effective against infections caused by non-albicans Candida species [27]. However, because neither colonization with C. albicans nor colonization with non-albicans Candida spp. was significantly predictive of the response in our study, we did not consider the possibility of treatment failure in patients who were colonized with non-albicans Candida.
Prophylaxis of invasive candidiasis in high risk ICU patients is possible [28, 29, 30]. Pelz et al. [28] noted that the risk of fungal infection was reduced by 55% in the prophylaxis group in critically ill surgical patients with an ICU stay of at least 3 days. Winston et al. [29] reported that prophylactic fluconazole after liver transplantation decreases fungal colonization and prevents superficial and invasive fungal infections. However, no study demonstrated that antifungal prophylaxis improved overall survival [28, 29, 30]. It is possible that the widespread use of fluconazole to prevent fungal infections in the ICU may lead to an increase in the isolation of C. krusei and C. glabrata, which are often resistant to fluconazole. Therefore, in general, early initiation of prophylaxis is not considered good practice in ICU patients with a low incidence of invasive candidiasis.
Conclusions
In patients with Candida colonization, assessment by the β-d-glucan assay was useful for deciding whether to start empiric therapy for suspected candidiasis in febrile surgical patients. Improved serologic and molecular techniques for detecting Candida spp. is necessary to identify patients who are at risk for severe fungal infection in a timely manner.
Résumé
Le but de cette étude fut de rechercher si l’examen pour du glucane β-d de plasma sanguin, qui est une paroi cellulaire constitutive de fungie, est utile dans la sélection de patients chirurgicaux ayant une colonisation de Candida et qui pourraient bénéficier d’une thérapie antifongique. Nous avons administré postopérativement du fluconazole à des patients ayant une colonisation de Candida qui présentaient des risques de candidémie et qui se plaignaient d’une fièvre persistante malgré une thérapie antibactérienne, et effectué des résultats cliniques analysant à la fois le nombre de sites colonisés avec des variétés de Candida et le glucane β-d de plasma sanguin. Quinze des 32 patients (46.9%) qui étaient positifs pour du glucane β-d ont réagi à une thérapie antifongique, comparé à seulement 9% de ceux qui ont réagi négativement (p < 0.01). Lors d’analyses de régressions logistiques multiples, la positivité pour du glucane β-d présentait une réponse prévisible de facteurs significatifs, avec un taux déparié réglé de 12,9 patients présentant une colonisation de Candida (IC de 95%, 2.07 à 80.73) (p < 0.01). En outre, le nombre de sites colonisés avec des variétés de Candida présentait une réponse prévisible de facteurs significatifs, avec un taux déparié d’exposition estimée à 7.57 pour ceux qui étaient colonisés sur trois ou davantage de sites, comparé à ceux qui étaient colonisés sur un seul site (IC de 95%, 1.20 à 47.70) (p = 0.031). Chez les patients ayant une colonisation de Candida, une estimation de glucane β-D fut utile pour décider le début d’une thérapie antifongique pour des patients chirurgicaux suspects d’une candidose.
Resumen
El fin del estudio fue investigar si la examinación para β-d-glucan de plasma que fue un constituyente de pared de célula de hongos es útil para seleccionar pacientes quirúrgicos con colonización Cándida, quienes podrían beneficiarse de terapia antifungosa empírica. Nosotros administramos flunconazole a pacientes posoperativos con colonización Cándida quienes tienen factores peligrosos para candidemia, y se quejan de fiebre persistente a pesar de terapia antibacterial prolongada, y resultados clínicos analizados tanto el número de lugares colonizados con spp Cándida como β-d-glucan de plasma. Quince de 32 pacientes (46.9%) quienes fueron positivos para β-d-glucan respondieron a la terapia empírica, mientras que sólo el 9% de aquéllos que fueron negativos respondieron (p < 0.01). En el análisis de regresión logística múltiple, positivos para β-d-glucan fue un factor significante prediciendo respuesta, con una relación de probabilidades ajustadas de 12.9 en pacientes con colonización Cándida (95% CI, 2.07 a 80.73) (p < 0.01). Además, el número de lugares colonizados con spp. Cándida fue un factor significante prediciendo respuesta, con una relación de probabilidades de exposición estimada de 7.57 para aquéllos que fueron colonizados en tres o más lugares comparado con aquéllos colonizados en un lugar (95% CI, 1.20 a 47.70) (p = 0.031). En pacientes con colonización Cándida, valoración mediante β-d-glucan fue útil para decidir el comienzo de terapia empírica para candidiasis presunta en pacientes quirúrgicos.
References
JS Solomkin AB Flohr PG Quie et al. (1980) ArticleTitleThe role of Candida in intraperitoneal infections Surgery 88 524–530 Occurrence Handle1:STN:280:Bi6D3svgslQ%3D Occurrence Handle7423375
D Pittet M Monod PM Suter et al. (1994) ArticleTitleCandida colonization and subsequent infections in critically ill surgical patients Ann. Surg. 220 751–758 Occurrence Handle1:STN:280:ByqD2sjkslI%3D Occurrence Handle7986142
Solomkin JS. Timing of treatment for nonneutropenic patients colonized with Candida. Am. J. Surg. 1996;172(Suppl. 6A):44–48
DA Dean KW Burchard (1998) ArticleTitleSurgical perspective on invasive Candida infections World J. Surg. 22 127–134 Occurrence Handle10.1007/s002689900360 Occurrence Handle1:STN:280:DyaK1c7htl2jug%3D%3D Occurrence Handle9451927
JH Rex TJ Walsh JD Sobel et al. (2000) ArticleTitlePractice guideline for the treatment of candidiasis Clin. Infect. Dis. 30 662–678 Occurrence Handle10.1086/313749 Occurrence Handle1:STN:280:DC%2BD3czotl2iuw%3D%3D Occurrence Handle10770728
InstitutionalAuthorNameBritish Society for Antimicrobial Chemotherapy Working Party (1994) ArticleTitleManagement of deep Candida infection in surgical and intensive care unit patients Intensive Care Med. 20 522–528
T Obayashi M Yoshida T Mori et al. (1995) ArticleTitlePlasma (1→3)- β-d-glucan measurement in diagnosis of invasive deep mycosis and fungal febrile episodes Lancet 345 17–20 Occurrence Handle10.1016/S0140-6736(95)91152-9 Occurrence Handle1:STN:280:ByqD1MjmvVU%3D Occurrence Handle7799700
T Mori H Ikemoto M Matsumura et al. (1997) ArticleTitleEvaluation of plasma (1→3)-β-d-glucan measurement by the kinetic turbidimetric Limulus test, for the clinical diagnosis of mycotic infections Eur. J. Clin. Chem. Clin. Biochem. 35 553–560 Occurrence Handle1:CAS:528:DyaK2sXltVGmsLk%3D Occurrence Handle9263735
H Tamura S Tanaka T Ikeda et al. (1997) ArticleTitlePlasma (1→3)-β-d-glucan assay and immunohistochemical staining of (1→3)-β-d-glucan in the fungal cell walls using a novel horseshoe crab protein (T-GBP) that specifically binds to plasma (1→3)-β-d-glucan J. Clin. Lab. Anal. 11 104–109 Occurrence Handle10.1002/(SICI)1098-2825(1997)11:2<104::AID-JCLA6>3.3.CO;2-E Occurrence Handle1:CAS:528:DyaK2sXhvFGjt7o%3D Occurrence Handle9058244
T Kawagoe A Nakao T Kanbe et al. (1998) ArticleTitleMeasurement of (1→3)-β-d-glucan in an experimental model of systemic candidiasis Eur. Surg. Res. 30 290–296 Occurrence Handle10.1159/000008589 Occurrence Handle1:CAS:528:DyaK1cXkvVGltrg%3D Occurrence Handle9704756
S Kohno K Mitsutake S Maesaki et al. (1993) ArticleTitleAn evaluation of serodiagnostic tests in patients with candidemia: beta-glucan, mannan, candida antigen by Cand-Tec and d-arabinitol Microbiol. Immunol. 37 207–212 Occurrence Handle1:STN:280:ByyA3cbjtl0%3D Occurrence Handle8321149
MA Hossain T Miyazaki K Mitsutake et al. (1997) ArticleTitleComparison between Wako-WB003 and Fungitec G test for detection of (1→3)-β-d-glucan in systemic mycosis J. Clin. Lab. Anal. 11 73–77 Occurrence Handle10.1002/(SICI)1098-2825(1997)11:2<73::AID-JCLA1>3.0.CO;2-L Occurrence Handle1:CAS:528:DyaK2sXhvFGjt78%3D Occurrence Handle9058239
T Miyazaki S Kohno K Mitsutake et al. (1995) ArticleTitlePlasma (1→3)-β-d-glucan and fungal antigenemia in patients with candidemia, aspergillosis, and cryptococcosis J. Clin. Microbiol. 33 3115–3118 Occurrence Handle1:CAS:528:DyaK28XltlCitA%3D%3D Occurrence Handle8586684
H Kanda K Kubo K Hamasaki et al. (2001) ArticleTitleInfluence of various hemodialysis membranes on the plasma (1→3)-β-d-glucan level Kidney Int. 60 319–323 Occurrence Handle10.1046/j.1523-1755.2001.00802.x Occurrence Handle1:CAS:528:DC%2BD3MXltlKnu78%3D Occurrence Handle11422767
K Ikemura K Ikegami T Shimazu et al. (1989) ArticleTitleFalse-positive result in Limulus test caused by Limulus amebocyte lysate-reactive material in immunoglobulin products J. Clin. Microbiol. 27 965–968
FW Kahn JM Jones (1986) ArticleTitleLatex agglutination tests for detection of Candida antigens in sera of patients with invasive candidiasis J. Infect. Dis. 153 579–585 Occurrence Handle1:STN:280:BimC2c7pvV0%3D Occurrence Handle3950441
A Kakinuma T Asano H Torii et al. (1981) ArticleTitleGelation of Limulus amebocyte lysate by an antitumor (1→3)-β-d-glucan Biochem. Biophys. Res. Commun. 101 434–439 Occurrence Handle1:CAS:528:DyaL3MXlt1GqsLk%3D Occurrence Handle7306087
SB Wey M Mori MA Phaller et al. (1989) ArticleTitleRisk factors for hospital-acquired candidemia: a matched case-control study Arch. Intern. Med. 149 2349–2353 Occurrence Handle10.1001/archinte.149.10.2349 Occurrence Handle1:STN:280:By%2BD38rmtVY%3D Occurrence Handle2802900
VJ Fraser M Jones J Dunkel et al. (1992) ArticleTitleCandidemia in a tertiary care hospital: epidemiology, risk factors, and predictors of mortality Clin. Infect. Dis. 15 414–421 Occurrence Handle1:STN:280:By2A1M3pvVU%3D Occurrence Handle1520786
PA Pizzo KJ Robichaud FA Gill et al. (1982) ArticleTitleEmpiric antibiotic and antifungal therapy for cancer patients with prolonged fever and granulocytopenia Am. J. Med. 72 101–111 Occurrence Handle10.1016/0002-9343(82)90594-0 Occurrence Handle1:STN:280:Bi2C3s3ms1A%3D Occurrence Handle7058815
JE Karp WG Merz P Charache et al. (1991) ArticleTitleResponse to empiric amphotericin B during antileukemic therapy-induced granulocytopenia Rev. Infect. Dis. 13 592–599 Occurrence Handle1:STN:280:By2D383ht1M%3D Occurrence Handle1925275
HG Prentice IM Hann R Herbrecht et al. (1997) ArticleTitleA randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyremia of unknown origin in neutropenic patients Br. J. Haematol. 98 711–718 Occurrence Handle10.1046/j.1365-2141.1997.2473063.x Occurrence Handle1:CAS:528:DyaK2sXmt1KrtLY%3D Occurrence Handle9332329
C Viscoli E Castagnola MT Lint ParticleVan et al. (1996) ArticleTitleFluconazole versus amphotericin B as empirical antifungal therapy of unexplained fever in granulocytopenia cancer patients: a pragmatic, multicentre, prospective and randomized clinical trial Eur. J. Cancer 32A 814–820 Occurrence Handle10.1016/0959-8049(95)00619-2 Occurrence Handle1:CAS:528:DyaK28XjvFynt70%3D Occurrence Handle9081359
DJ Winston JW Hathorn MG Schuster et al. (2000) ArticleTitleA multicenter, randomized trial of fluconazole versus amphotericin B for empiric antifungal therapy of febrile neutropenic patients with cancer Am. J. Med. 108 282–289 Occurrence Handle10.1016/S0002-9343(99)00457-X Occurrence Handle1:CAS:528:DC%2BD3cXit1Gqt7g%3D Occurrence Handle11014720
IA Malik I Moid Z Aziz et al. (1998) ArticleTitleA randomized comparison of fluconazole with amphotericin B as empiric anti-fungal agents in cancer patients with prolonged fever and neutropenia Am. J. Med. 105 478–483 Occurrence Handle10.1016/S0002-9343(98)00326-X Occurrence Handle1:CAS:528:DyaK1MXjs1ynug%3D%3D Occurrence Handle9870832
Y Kimura A Nakao H Tamura et al. (1995) ArticleTitleClinical and experimental studies of the limulus test after digestive surgery Surg. Today 25 790–794 Occurrence Handle1:STN:280:BymC3cjnvVY%3D Occurrence Handle8555696
DP Kontoyiannis GP Bodey CS Mantzoros (2001) ArticleTitleFluconazole vs. amphotericin B for the management of candidaemia in adults: a meta-analysis Mycosis 44 125–135 Occurrence Handle10.1046/j.1439-0507.2001.00649.x Occurrence Handle1:CAS:528:DC%2BD3MXmtVOms7s%3D
RK Pelz CW Hendrix SM Swoboda et al. (2001) ArticleTitleDouble blind placebo-controlled trial of fluconazole to prevent candidal infections in critically ill surgical patients Ann. Surg. 233 542–548 Occurrence Handle10.1097/00000658-200104000-00010 Occurrence Handle1:STN:280:DC%2BD3M3kvVajtA%3D%3D Occurrence Handle11303137
DJ Winston A Pakrasi RW Busuttil (1999) ArticleTitleProphylactic fluconazole in liver transplant recipients a randomized, double-blind, placebo-controlled trial Ann. Intern. Med. 131 729–737 Occurrence Handle1:CAS:528:DyaK1MXnvFOgs78%3D Occurrence Handle10577295
P Eggimann P Francioli J Bille et al. (1999) ArticleTitleFluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients Crit. Care Med. 27 1066–1072 Occurrence Handle10.1097/00003246-199906000-00019 Occurrence Handle1:STN:280:DyaK1Mzitlegtw%3D%3D Occurrence Handle10397206
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takesue, Y., Kakehashi, M., Ohge, H. et al. Combined Assessment of β-d-Glucan and Degree of Candida Colonization before Starting Empiric Therapy for Candidiasis in Surgical Patients. World J. Surg. 28, 625–630 (2004). https://doi.org/10.1007/s00268-004-7302-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-004-7302-y