Abstract
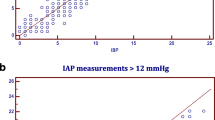
This study was designed to establish if clinical examination can accurately predict intraabdominal pressure (IAP). Between August 1998 and March 2000 a prospective blinded observational study of postoperative intensive care unit patients was undertaken at a major trauma center. IAP was measured using an intravesicular technique and compared with clinical evaluation. An IAP of at least 18 mmHg was considered elevated. The sensitivity, specificity, positive predicative value (npv), negative predictive value (npv), kappa score, and reliability analysis were calculated. A total of 110 patients provided 150 estimates of IAP, which was elevated in 21%. The kappa score was 0.37; sensitivity, 60.9%; specificity, 80.5%; ppv, 45.2%; npv, 88.6%. The mean difference in IAP values between intravesicular readings and clinical estimates was −1.0±4.1. Prediction of IAP using clinical examination is not accurate enough to replace intravesicular IAP measurements.
Résumé
Le but de cette étude a été d’établir si l’examen clinique peut prédire avec précision la pression intra-abdominale (PIA). Entre août 1998 et mars 2000 on a entrepris une étude observationnelle prospective à l’insu des patients post-opératoires en soins intensifs (SI) hospitalisés dans un centre de traumatologie majeure. La PIA a été mesurée par la technique intravésicale et comparée à l’évaluation clinique. On a considéré qu’une PIA ≥ 18 mmHg était «élevée». On a calculé la sensibilité (Se), la spécificité (Sp), la valeur prédictive positive (VPP), la valeur prédictive négative (VPN), le score kappa, et la fiabilité. On a estimé cliniquement la PIA 150 fois chez 110 patients. La PIA était élevée dans 21% des cas. Le score Kappa a été de 0.37, la Se de 60.9%, la Sp, de 80.5%, la VPP de 45.2%, la VPN, de 88.6%. La différence moyenne en PIA entre la valeur intra-vésicale et l’estimation clinique a été de −1.0±4.1. La prédiction de la PIA par examen clinique n’est pas suffisamment précise pour remplacer la mesure par pression intravésicale.
Resumen
El objetivo del estudio fue averiguar si la exploración clínica permite evaluar con exactitud la presión intraabdominal (IAP). Entre agosto de 1998 y marzo de 2000, se efectuó un estudio prospective ciego, durante el postoperatorio de pacientes ingresados en la UCI de un Centro Traumatológico de referencia. La IAP se midió mediante la técnica intravesical comparandose con los hallazgos clínicos obtenidos. Se consideró que la presión estaba elevada cuando la IAP era ≥18 mm Hg. Comprobamos: la sensibilidad, especificidad, valor predictivo positivo (ppv) y negativo (npv), la puntuación de Kappa y la fiabilidad de los análisis. La puntuación de Kappa fue de 0.37, la sensibilidad del 60.9%, especificidad 80.5%, ppv 45.2% y npv 88.6%. La diferencia media entre los valores de la IAP registrados mediante sonda intravesical y los estimados por la exploración clínica fueron de −1.0±4.1. La valoración clínica de la IAP no es lo suficientemente precisa como para reemplazar la medición intravesical.
Similar content being viewed by others
References
Sugrue M. Jones F, Deane SA. et al. Intra-abdominal hypertension is an independent cause of post-operative renal impairment. Arch. Surg. 1999; 134:1082
Cheatham ML, White MW. Sagraves SG, et al. Abdominal perfusion pressure; a superior parameter in assessment of intra-abdominal hypertension. J. Trauma 2000;49:621
Ivatury R, Porter J, Simon R, et al. Intra-abdominal hypertension after life-threatening penetrating abdominal trauma: prophylaxis, incidence, and clinical relevance to gastric mucosal pH and abdominal compartment syndrome. J. Trauma 1998;44:1016
Ertel W, Oberholzer A, Platz A, et al. Evidence and clinical pattern of abdominal compartment syndrome after “damage-control” laparotomy in 311 patients with severe abdominal or pelvic trauma. Crit. Care Med. 2000:28:1747
Sugrue M, Jones F. Lee A. et al. Intraabdominal pressure and gastric intramucosal pH: is there an association? World J. Surg. 1996;20:988
Kirkpatrick AW. Brenneman FD, McLean RF, et al. Is clinical examination an accurate indicator of raised intra-abdominal pressure in critically injured patients? Can. J. Surg. 2000;43:3:207
Castillo M, Lis RJ. Ulrich H. et al. Clinical estimate compared to intra-abdominal pressure measurement (abs). Crit. Care Med. 1998:26(Suppl):A78
Rapanos T, Boulanger B, McLean R, et al. Is clinical examination an accurate indicator of intra-abdominal pressure in ventilated patients. Crit. Care Med. 1998;25(Suppl):A133
Sugrue M, Buist MD, Lee A, et al. Intra-abdominal pressure measurement using a modified nasogastric tube: description and validation of a new technique. Intensive Care Med. 1995;20:588
Kron IL, Harman PK, Nolan SP. The measurement of intraabdominal pressure as a criterion for abdominal re-exploration. Ann. Surg. 1984;196:594
Fusco MA, Martin SR, Chang MC. Estimation of intra-abdominal pressure by bladder pressure measurement: validity and methodology. J. Trauma 2001;50:297–302
Platell C, Hall J, Dobb G. Impaired renal function due to raised intraabdominal pressure. Intensive Care Med. 1990;16:328
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307
Fairclough JA, Mintowt-Czyz J, Mackie I, et al. Abdominal girth; an unreliable measure of intra-abdominal bleeding. Injury 1984;6:85
Sugrue M, Buist MD, Hourihan F, et al. Prospective study of intra-abdominal hypertension and renal function after laparotomy. Br. J. Surg. 1995;82:235
Pusajo J, Bumaschny E, Agurrola A, et al. Post-operative intra-abdominal pressure: its relation to splanchnic perfusion, sepsis, multiple organ failure and surgical intervention. Int. Crit. Care Digest. 1994:13:2
Lacey JB, Brooks SP, Griswald J, et al. The relative merits of various methods of indirect measurement of intraabdominal pressure as a guide to closure of abdominal wall defects. J. Pediatr. Surg. 1987;22:1207
Sugrue M, Jones F, Janjua KJ, et al. Temporary abdominal closure: a prospective evaluation of its effects on renal and respiratory physiology. J. Trauma 1998:45:914
Sugrue M, Hillman K. Intraabdominal pressure and intensive care. In Vincent JL, editor, Yearbook of Intensive Care and Emergency Medicine, Berlin, Springer-Verlag, 1998:667–676
Sugrue M, D’Amours S. Secondary abdominal compartment syndrome. J. Trauma 2001;51:419
Author information
Authors and Affiliations
Additional information
Published Online: September 26, 2002
Rights and permissions
About this article
Cite this article
Sugrue, M., Bauman, A., Jones, F. et al. Clinical examination is an inaccurate predictor of intraabdominal pressure. World J. Surg. 26, 1428–1431 (2002). https://doi.org/10.1007/s00268-002-6411-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-002-6411-8