Abstract
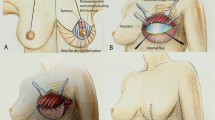
In patients with large breasts undergoing a subcutaneous mastectomy with immediate implant-based reconstruction, is necessary to perform a mastopexy. The combination of these procedures increases the complication rate. To reduce it, it is necessary to cover the lower pole of the implant. Our study aimed to compare the use of an autologous dermal flap and an absorbable breast mesh. A total of 64 patients without previous breast surgery were divided into 2 groups, each with 32 patients. In the 1st group, the implant was covered with an autologous caudally based dermal flap, sutured to the great pectoral muscle. In the 2nd group, the implant was covered with a fully absorbable breast mesh, fixed caudally in the inframammary fold and cranially to the great pectoral muscle. The incidence of complications, the aesthetic effect, and patient satisfaction were evaluated in a one-year follow-up. In the 1st group, there were 2 cases of seroma, 2 partial nipple-areola complex necrosis, 4 cases of dehiscence in the T-suture, and the malposition of the implant in 2 patients. In the 2nd group, there were 2 cases of seroma, 2 cases of T-junction dehiscence, and 1 case of full nipple-areola complex necrosis, which resulted in implant loss. There was no significant difference in patient satisfaction between the study groups. The dermal flap is more suitable for breasts with pronounced ptosis. The use of the synthetic mesh is suitable for smaller breasts, where the possible dermal flap would be too small to cover the implant.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.




Similar content being viewed by others
References
Freeman BS (1962) Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Reconstr Surg 30:676–682
Lalloo F, Baildam A, Brain A et al (2000) A protocol for preventative mastectomy in women with an increased lifetime risk of breast cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 26:711–713. https://doi.org/10.1053/ejso.2000.0986
Ross GL (2012) One stage breast reconstruction following prophylactic mastectomy for ptotic breasts: the inferior dermal flap and implant. J Plast Reconstr Aesthet Surg 65:1204–1208. https://doi.org/10.1016/j.bjps.2012.03.040
Wagner JL, Fearmonti R, Hunt KK et al (2012) Prospective evaluation of the nipple-areola complex sparing mastectomy for risk reduction and for early-stage breast cancer. Ann Surg Oncol 19:1137–1144. https://doi.org/10.1245/s10434-011-2099-z
De Vita R, Zoccali G, Buccheri EM et al (2017) Outcome evaluation after 2023 nipple-sparing mastectomies: our experience. Plast Reconstr Surg 139:345e–347e. https://doi.org/10.1097/PRS.0000000000003027
Kontos M, Lanitis S, Constantinidou A et al (2020) Nipple-sparing skin-reducing mastectomy with reconstruction for large ptotic breasts. J Plast Reconstr Aesthet Surg 73:690–695. https://doi.org/10.1016/j.bjps.2019.11.025
Rusby JE, Gui GPH (2010) Nipple-sparing mastectomy in women with large or ptotic breasts. J Plast Reconstr Aesthet Surg 63:e754–e755
Heidemann LN, Gunnarsson GL, Salzberg CA et al (2018) Complications following nipple-sparing mastectomy and immediate acellular dermal matrix implant-based breast reconstruction-a systematic review and meta-analysis. Plast Reconstr Surg Glob Open 6:e1625–e1625. https://doi.org/10.1097/GOX.0000000000001625
Komorowski AL, Zanini V, Regolo L et al (2006) Necrotic complications after nipple-and areola-sparing mastectomy. World J Surg 30:1410–1413. https://doi.org/10.1007/s00268-005-0650-4
Bernini M, Calabrese C, Cecconi L et al (2015) Subcutaneous direct-to-implant breast reconstruction: surgical, functional, and aesthetic results after long-term follow-up. Plast Reconstr surg Glob open 3:e574. https://doi.org/10.1097/GOX.0000000000000533
Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW (2000) The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 26:17–19. https://doi.org/10.1053/ejso.1999.0733
Sisco M, Yao KA (2016) Nipple-sparing mastectomy: a contemporary perspective. J Surg Oncol 113:883–890. https://doi.org/10.1002/jso.24209
Metcalfe KA, Cil TD, Semple JL et al (2015) Long-term psychosocial functioning in women with bilateral prophylactic mastectomy: does preservation of the nipple-areolar complex make a difference? Ann Surg Oncol 22:3324–3330. https://doi.org/10.1245/s10434-015-4761-3
Susarla SM, Ganske I, Helliwell L et al (2015) Comparison of clinical outcomes and patient satisfaction in immediate single-stage versus two-stage implant-based breast reconstruction. Plast Reconstr Surg 135:1e–8e. https://doi.org/10.1097/PRS.0000000000000803
Rebowe RE, Allred LJ, Nahabedian MY (2018) The evolution from subcutaneous to prepectoral prosthetic breast reconstruction. Plast Reconstr Surg Glob Open 6:e1797–e1797. https://doi.org/10.1097/GOX.0000000000001797
della Rovere GQ, Nava M, Bonomi R et al (2008) Skin-reducing mastectomy with breast reconstruction and sub-pectoral implants. J Plast Reconstr Aesthet Surg 61:1303–1308. https://doi.org/10.1016/j.bjps.2007.06.032
Mestak J, Sukop A, Mestak O (2011) Use of deepithelialized flap in mammoplasties: simple method with excellent results. Aesthet Plast Surg 35:1106–1111. https://doi.org/10.1007/s00266-011-9745-5
Carstensen L (2019) Visualized immediate breast reconstruction with dermal flap and implant. Gland Surg 8:S255–S261. https://doi.org/10.21037/gs.2019.03.07
Rochlin DH, Nguyen DH (2018) Deepithelialized skin reduction preserves skin and nipple perfusion in immediate reconstruction of large and ptotic breasts. Ann plast surg. https://doi.org/10.1097/SAP.0000000000001427
Hansson E, Jepsen C, Hallberg H (2018) Breast reconstruction with a dermal sling: a systematic review of surgical modifications. J Plast Surg Hand Surg. https://doi.org/10.1080/2000656X.2018.1533840
Eichler C, Schulz C, Thangarajah F et al (2019) A retrospective head-to-head comparison between TiLoop Bra/TiMesh® and Seragyn® in 320 cases of reconstructive breast surgery. Anticancer Res 39:2599–2605. https://doi.org/10.21873/anticanres.13383
Margulies IG, Salzberg CA (2019) The use of acellular dermal matrix in breast reconstruction: evolution of techniques over 2 decades. Gland Surg 8:3–10. https://doi.org/10.21037/gs.2018.10.05
Gunnarsson GL, Bille C, Reitsma LC et al (2017) Prophylactic nipple-sparing mastectomy and direct-to-implant reconstruction of the large and ptotic breast: Is preshaping of the challenging breast a key to success? Plast Reconstr Surg 140:449–454. https://doi.org/10.1097/PRS.0000000000003621
Rezai M, Strauß S, Kimmig R, Kern P (2016) Risk-reducing, conservative mastectomy-analysis of surgical outcome and quality of life in 272 implant-based reconstructions using TiLoop (®) Bra versus autologous corial flaps. Gland Surg 5:1–8. https://doi.org/10.3978/j.issn.2227-684X.2015.07.03
Dieterich M, Stubert J, Gerber B et al (2015) Biocompatibility, cell growth and clinical relevance of synthetic meshes and biological matrixes for internal support in implant-based breast reconstruction. Arch Gynecol Obstet 291:1371–1379. https://doi.org/10.1007/s00404-014-3578-9
Salibian AA, Frey JD, Choi M, Karp NS (2016) Subcutaneous implant-based breast reconstruction with acellular dermal matrix/mesh: a systematic review. Plast Reconstr Surg Glob Open 4:e1139. https://doi.org/10.1097/GOX.0000000000001139
Pusic AL, Klassen AF, Scott AM et al (2009) Development of a new patient-reported outcome measure for breast surgery: the Breast-Q. Plast Reconstr Surg 124:345–353. https://doi.org/10.1097/PRS.0b013e3181aee807
Spear SL, Rottman SJ, Seiboth LA, Hannan CM (2012) Breast reconstruction using a staged nipple-sparing mastectomy following mastopexy or reduction. Plast Reconstr Surg 129:572–581
Robertson SA, Jeevaratnam JA, Agrawal A, Cutress RI (2017) Mastectomy skin flap necrosis: challenges and solutions. Breast Cancer Dove Med Press 9:141–152. https://doi.org/10.2147/BCTT.S81712
Bayram Y, Kulahci Y, Irgil C et al (2010) Skin-reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. Aesthet Plast Surg 34:71–77. https://doi.org/10.1007/s00266-009-9452-7
Tessler O, Reish RG, Maman DY et al (2014) Beyond biologics: Absorbable mesh as a low-cost, low-complication sling for implant-based breast reconstruction. Plast Reconstr Surg 133:90–99. https://doi.org/10.1097/01.prs.0000437253.55457.63
Krishnan NM, Chatterjee A, Van Vliet MM et al (2013) A comparison of acellular dermal matrix to autologous dermal flaps in single-stage, implant-based immediate breast reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg 131:953–961
Funding
No Funding to disclosure.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patzelt, M., Zarubova, L., Vecerova, M. et al. Risk Comparison Using Autologous Dermal Flap and Absorbable Breast Mesh on Patient Undergoing Subcutaneous Mastectomy with Immediate Breast Reconstruction. Aesth Plast Surg 46, 1145–1152 (2022). https://doi.org/10.1007/s00266-022-02799-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02799-6