Abstract
Background
Biological matrix-assisted one-stage implant-based breast reconstruction (IBBR) could improve the inframammary fold to achieve good esthetic results. However, whether biological matrix-assisted one-stage IBBR yields better postoperative outcomes compared with two-stage IBBR remains unclear. We aimed to compare and analyze surgical complications and patient-reported outcomes (PROs) based on the BREAST-Q version 2.0 questionnaire between biological matrix-assisted one-stage IBBR and traditional two-stage IBBR.
Methods
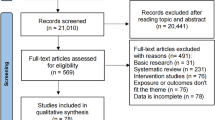
From May 2015 to June 2019, eligible patients who underwent SIS matrix-assisted one-stage IBBR or two-stage IBBR were enrolled in this retrospective cohort study. PROs were measured with BREAST-Q version 2.0, which scored the health-related quality of life, satisfaction, and experience domains. Complications were divided into major complications (patients requiring reoperation) and minor complications (patients who could be treated in the dressing room). PROs and complications were compared between the SIS matrix-assisted one-stage IBBR and two-stage IBBR groups. A multivariate linear regression analysis was used to identify the social and surgical factors that affected PROs.
Results
At our institution, 124 eligible patients were recruited. Seventy-nine patients (63.7%) underwent SIS matrix-assisted one-stage IBBR reconstruction, and 45 patients (36.3%) underwent tissue expander/implant reconstruction (two-stage IBBR). Postoperative BREAST-Q version 2.0 was completed by 68 of 79 patients (86.1%) in the SIS matrix-assisted one-stage IBBR group and by 35 of 45 patients (77.8%) in the two-stage IBBR group. In the satisfaction-related quality of life domain, satisfaction with breast was 9.27 points higher in the SIS matrix-assisted one-stage IBBR group (p = 0.012) compared with the two-stage IBBR group. The multivariate linear regression analysis showed that implant volume (p = 0.031) and postoperative radiotherapy (p = 0.036) significantly influenced the PRO of satisfaction with breast. However, patients in the SIS matrix-assisted one-stage IBBR group had a higher minor complication rate compared with patients in the two-stage IBBR group (p = 0.026).
Conclusions
Our retrospective study showed that although patients treated with biological matrix-assisted one-stage IBBR tended to have higher postoperative complication rates, this technique correlated with better PROs compared with two-stage IBBR.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Availability of data and material
The data generated or analyzed during this study are included in this article, or if absent are available from the corresponding author upon reasonable request.
References
Miller KD, Siegel RL, Lin CC et al (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4):271–289. https://doi.org/10.3322/caac.21349
Razdan SN, Cordeiro PG, Albornoz CR et al (2016) Cost-effectiveness analysis of breast reconstruction options in the setting of postmastectomy radiotherapy using the BREAST-Q. Plast Reconstr Surg 137(3):510e–517e. https://doi.org/10.1097/01.prs.0000479935.92904.a3
Rodriguez-Feliz J, Codner MA (2015) Embrace the change: incorporating single-stage implant breast reconstruction into your practice. Plast Reconstr Surg 136(2):221–231. https://doi.org/10.1097/PRS.0000000000001448
Colwell AS (2012) Direct-to-implant breast reconstruction. Gland Surg 1(3):139–141. https://doi.org/10.3978/j.issn.2227-684X.2012.10.04
Colwell AS, Tessler O, Lin AM et al (2014) Breast reconstruction following nipple-sparing mastectomy: predictors of complications, reconstruction outcomes, and 5-year trends. Plast Reconstr Surg 133(3):496–506. https://doi.org/10.1097/01.prs.0000438056.67375.75
Hamann M, Brunnbauer M, Scheithauer H et al (2019) Quality of life in breast cancer patients and surgical results of immediate tissue expander/implant-based breast reconstruction after mastectomy. Arch Gynecol Obstet 300(2):409–420. https://doi.org/10.1007/s00404-019-05201-0
Srinivasa DR, Garvey PB, Qi J et al (2017) Direct-to-implant versus two-stage tissue expander/implant reconstruction: 2-year risks and patient-reported outcomes from a prospective, multicenter study. Plast Reconstr Surg 140(5):869–877. https://doi.org/10.1097/PRS.0000000000003748
Clarke-Pearson EM, Lin AM, Hertl C et al (2016) Revisions in implant-based breast reconstruction: how does direct-to-implant measure up? Plast Reconstr Surg 137(6):1690–1699. https://doi.org/10.1097/PRS.0000000000002173
Azouz V, Lopez S, Wagner DS (2018) Surgeon-controlled comparison of direct-to-implant and 2-stage tissue expander-implant immediate breast reconstruction outcomes. Ann Plast Surg 80(3):212–216. https://doi.org/10.1097/SAP.0000000000001220
Dikmans RE, Negenborn VL, Bouman MB et al (2017) Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol 18(2):251–258. https://doi.org/10.1016/S1470-2045(16)30668-4
Brunbjerg M, Jensen T, Overgaard J et al (2021) Comparison of one-stage direct-to-implant with acellular dermal matrix and two-stage immediate implant-based breast reconstruction-a cohort study. Gland Surg 10(1):207–218. https://doi.org/10.21037/gs-20-581
Pusic AL, Klassen AF, Scott AM et al (2009) Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 124(2):345–353. https://doi.org/10.1097/PRS.0b013e3181aee807
Klassen AF, Pusic AL, Scott A et al (2009) Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Women’s Health 1(9):11. https://doi.org/10.1186/1472-6874-9-11
Cano SJ, Klassen AF, Scott AM et al (2012) The BREAST-Q: further validation in independent clinical samples. Plast Reconstr Surg 129(2):293–302. https://doi.org/10.1097/PRS.0b013e31823aec6b
Pusic AL, Matros E, Fine N et al (2017) Patient-reported outcomes 1 year after immediate breast reconstruction: results of the mastectomy reconstruction outcomes consortium study. J Clin Oncol 35(22):2499–2506. https://doi.org/10.1200/JCO.2016.69.9561
Pusic A, Klassen A, Cano S (2017) BREAST-Q Version 2.0© reconstruction module pre- and postoperative scales. Memorial Sloan Kettering Cancer Center and the University of British Columbia
Nelson JA, Allen RJ Jr, Polanco T et al (2019) Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 270(3):473–483. https://doi.org/10.1097/SLA.0000000000003467
Lin KY, Blechman AB, Brenin DR (2012) Implant-based, two-stage breast reconstruction in the setting of radiation injury: an outcome study. Plast Reconstr Surg 129(4):817–823. https://doi.org/10.1097/PRS.0b013e31824421d0
Baldelli I, Cardoni G, Franchelli S et al (2016) Implant-based breast reconstruction using a polyester mesh (Surgimesh-PET): a retrospective single-center study. Plast Reconstr Surg 137(6):931e-e939. https://doi.org/10.1097/PRS.0000000000002180
Sorkin M, Qi J, Kim HM et al (2017) Acellular dermal matrix in immediate expander/implant breast reconstruction: a multicenter assessment of risks and benefits. Plast Reconstr Surg 140(6):1091–1100. https://doi.org/10.1097/PRS.0000000000003842
McCarthy CM, Lee CN, Halvorson EG, Riedel E et al (2012) The use of acellular dermal matrices in two-stage expander/implant reconstruction: a multicenter, blinded, randomized controlled trial. Plast Reconstr Surg 130(502):57S
Killaars RC, Hommes J, van der Hulst RR et al (2018) Does 2-stage implant-based breast reconstruction allow for a larger volume of the definite implant compared with 1-stage reconstruction? Ann Plast Surg 80(5):481–486. https://doi.org/10.1097/SAP.0000000000001352
Hallberg H, Rafnsdottir S, Selvaggi G et al (2018) Benefits and risks with acellular dermal matrix (ADM) and mesh support in immediate breast reconstruction: a systematic review and meta-analysis. J Plast Surg Hand Surg 52(3):130–147. https://doi.org/10.1080/2000656X.2017.1419141
Handel N, Jensen J, Black Q et al (1995) The fate of breast implants: a critical analysis of complications and outcomes. Plast Reconstr Surg 96(7):1521–1533. https://doi.org/10.1097/00006534-199512000-00003
Yun JH, Diaz R, Orman AG (2018) Breast reconstruction and radiation therapy. Cancer Control 25(1):1073274818795489
Pusic AL, Chen CM, Cano S et al (2007) Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg 120(4):823–37. https://doi.org/10.1097/01.prs.0000278162.82906.8 (discussion 838-9)
Pusic AL, Klassen AF, Snell L et al (2012) Measuring and managing patient expectations for breast reconstruction: impact on quality of life and patient satisfaction. Expert Rev Pharmacoecon Outcomes Res 12(2):149–158. https://doi.org/10.1586/erp.11.105
Liu C, Zhuang Y, Momeni A et al (2014) Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast Cancer Res Treat 146(1):117–126. https://doi.org/10.1007/s10549-014-2981-z
Negenborn VL, Young-Afat DA, Dikmans REG et al (2018) Quality of life and patient satisfaction after one-stage implant-based breast reconstruction with an acellular dermal matrix versus two-stage breast reconstruction (BRIOS): primary outcome of a randomised, controlled trial. Lancet Oncol 19(9):1205–1214. https://doi.org/10.1016/S1470-2045(18)30378-4
Sewart E, Turner NL, Conroy EJ et al (2020) The impact of radiotherapy on patient-reported outcomes of immediate implant-based breast reconstruction with and without mesh. Ann Surg. https://doi.org/10.1097/SLA.0000000000004245
Jagsi R, Momoh A, Qi J et al (2018) Impact of radiotherapy on complications and patient-reported outcomes after breast reconstruction. J Natl Cancer Inst 110(2):157–165. https://doi.org/10.1093/jnci/djx148
Kim H, Park S, Woo K et al (2019) Comparative study of nipple-areola complex position and patient satisfaction after unilateral mastectomy and immediate expander-implant reconstruction nipple-sparing mastectomy versus skin-sparing mastectomy. Aesthetic Plast Surg 43(2):313–327. https://doi.org/10.1007/s00266-018-1217-8
Barber MD, Williams L, Anderson ED et al (2014) Outcome of the use of acellular-dermal matrix to assist implant-based breast reconstruction in a single centre. Eur J Surg Oncol 41(1):100–105
Gao P, Wang Z, Kong X et al (2020) Comparisons of therapeutic and aesthetic effects of one-stage implant-based breast reconstruction with and without biological matrix. Cancer Manag Res 12:13381–13392. https://doi.org/10.2147/cmar.S282442
Salzberg CA (2012) Focus on technique: one-stage implant-based breast reconstruction. Plast Reconstr Surg 130(5 Suppl 2):95S-103S. https://doi.org/10.1097/PRS.0b013e318262e1a1
Salzberg CA (2012) Direct-to-implant breast reconstruction. Clin Plast Surg 39(2):119–126. https://doi.org/10.1016/j.cps.2012.01.001
Salzberg CA, Ashikari AY, Berry C et al (2016) Acellular dermal matrix-assisted direct-to-implant breast reconstruction and capsular contracture: a 13-year experience. Plast Reconstr Surg 138(2):329–337. https://doi.org/10.1097/PRS.0000000000002331
Cordeiro PG, McGuire P, Murphy DK (2015) Natrelle 410 extra-full projection silicone breast implants: 2-year results from two prospective studies. Plast Reconstr Surg 136(4):638–646. https://doi.org/10.1097/PRS.0000000000001636
Swanson E (2017) Evidence-based cosmetic breast surgery. Springer Nature, Basingstoke
Acknowledgments
This work was supported by the Natural Science Foundation of China (No. 81872160), the Natural Science Foundation of China (No. 82072940), the China National Key R&D (or Research and Development) Program (No. 2020AAA0105000 and 2020AAA0105004), the Beijing Municipal Natural Science Foundation (Key Project) (No. 7191009), the Beijing Municipal Natural Science Foundation (No. 7204293), the Special Research Fund for Central Universities, Peking Union Medical College (No. 3332019053), the Beijing Hope Run Special Fund of Cancer Foundation of China (No. LC2019B03), the Beijing Hope Run Special Fund of Cancer Foundation of China (No. LC2019L07), the Beijing Hope Run Special Fund of Cancer Foundation of China (No. LC2020L01), the Golden Bridge Project Seed Fund of Beijing Association for Science and Technology (No. ZZ20004), the 2021 Chaoyang District Social Development Science and Technology Plan Project (Medical and Health Field) (No. CYSF2115), the Chinese Young Breast Experts Research project (No. CYBER-2021-005), the XianSheng Clinical Research Special Fund of China International Medical Foundation (No. Z-2014-06-2103), and the Beijing Xisike Clinical Oncology Research Foundation (No. Y-Young2021-0017).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
The experiments were approved by Ethics Committee of Cancer Hospital of Chinese Academy of Medical Sciences.
Informed consent
All participants provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, P., Bai, P., Ren, Y. et al. Biological Matrix-Assisted One-Stage Implant-Based Breast Reconstruction Versus Two-Stage Implant-Based Breast Reconstruction: Patient-Reported Outcomes and Complications. Aesth Plast Surg 45, 2581–2590 (2021). https://doi.org/10.1007/s00266-021-02509-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-021-02509-8