Abstract
Introduction
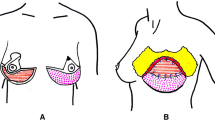
Large and ptotic breasts always represented a great reconstructive challenge for plastic surgeons. In order to deal with these patients, we started performing Wise-pattern skin-reducing mastectomies (SRM) followed by direct-to-implant breast reconstructions (DTI-BR) in the prepectoral space where the implants were covered with the autologous adipo-dermal flap and a human acellular dermal matrix called MODA.
Materials and Method
We retrospectively reviewed all patients that underwent Wise-pattern SRM followed by MODA-assisted, prepectoral, DTI-BR between January 2017 and November 2019 at our Institution. Inclusion criteria were large ptotic breast and pinch test >2cm, while exclusion criteria were smoking >10 cigarettes/day, history of prior radiotherapy, patients supposedly requiring breast implants bigger than 550cc or post-mastectomy radiotherapy. Patients’ data were collected through their electronic medical records. Both short- and long-term outcomes were reported.
Results
Seventeen patients underwent Wise-pattern SRM followed by MODA-assisted, prepectoral, DTI-BR for a total of twenty-one breast reconstruction and fourteen matching procedures. Mean follow-up was 13.4 months (SD= ±3.67). No major complication was reported. Three (14.3%) reconstructed breasts had minor complications: 2 (9.5%) minimal (<1cm2) wound dehiscence and 1 (4.8%) de-epithelization of the skin at the T junction that were treated conservatively. Drainages gave mean output of 410.59 ml (SD= ±214.83) and were kept in place on average for 8.59 days (SD= ±3.45).
Conclusion
Few are the reports in the literature regarding DTI-BR following SRM and even fewer are those where BR was performed in the prepectoral space. Our work demonstrated the safety of prepectoral DTI-BR following SRM in selected patients in accordance with the “conservative reconstruction” principles. Furthermore, we confirmed the reliability of MODA in accordance with previously published works.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.



Similar content being viewed by others
References
Bertozzi N, Pesce M, Santi PL, Raposio E (2017) Oncoplastic breast surgery: comprehensive review. Eur Rev Med Pharmacol Sci 21:2572–2585
Nava MB, Cortinovis U, Ottolenghi J et al (2006) Skin-reducing mastectomy. Plast Reconstr Surg 118:603–613
Reitsamer R, Peintinger F, Klaasen-Federspiel F, Sir A (2019) Prepectoral direct-to-implant breast reconstruction with complete ADM or synthetic mesh coverage e 36-Months follow-up in 200 reconstructed breasts. The Breast 40:32–37
Bertozzi N, Pesce M, Santi PL, Raposio E (2017) One-stage immediate breast reconstruction: a concise review. BioMed Res Int. https://doi.org/10.1155/2017/6486859
Folli S, Curcio A, Melandri D et al (2018) A new human-derived acellular dermal matrix for breast reconstruction available for the European market: Preliminary results. Aesthetic Plast Surg 42:434–441
Yde SS, Brunbjerg ME, Damsgaard TE (2016) Acellular dermal matrices in breast reconstructions—a literature review. J Plast Surg Hand Surg 50:187–196
Aurora A, McCarron J, Iannotti JP, Derwin K (2007) Commercially available extracellular matrix materials for rotator cuff repair: state of the art and future trends. J Shoulder Elbow Surg 16:171S-S178
Fini M, Bondioli E, Castagna A et al (2012) Decellularized human dermis to treat massive rotator cuff tears: in vitro evaluations. Connect Tissue Res 53:298–306
Rotini R, Marinelli A, Guerra E et al (2011) Human dermal matrix scaffold augmentation for large and massive rotator cuff repairs: preliminary clinical and MRI results at 1-year follow-up. Musculoskelet Surg 95:S13–S23
Giavaresi G, Bondioli E, Melandri D et al (2013) Response of human chondrocytes and mesenchymal stromal cells to a decellularized human dermis. BMC Musculoskelet Disord 14:12
Ghetti M, Bondioli E, Purpura V, Cenacchi G, Ruscelli P, Melandri D (2017) Decellularized human dermal matrix produced by a skin bank: a new treatment for abdominal wall defects. Ann Ital Chir 5:443–448
Gasperoni M, Neri R, Carboni A, Purpura V, Morselli PG, Melandri D (2016) The alexander surgical technique for the treatment of severe burns. Ann Burns Fire Disasters 29:281–285
Newman MK (2016) Reconstruction of the ptotic breast using wise pattern skin deepithelialization. Plast Reconstr Surg Glob Open 4:e1077. https://doi.org/10.1097/GOX.0000000000001077
Dikmans REG, Nene LEH, Mb B et al (2017) The aesthetic items scale: a tool for the evaluation of aesthetic outcome after breast reconstruction. Plast Reconstr Surg Glob Open 5:e1254. https://doi.org/10.1097/GOX.0000000000001254
Visser NJ, Damen TH, Timman R et al (2010) Surgical results, aesthetic outcome, and patient satisfaction after microsurgical autologous breast reconstruction following failed implant reconstruction. Plast Reconstr Surg 126:26–36
Adams WP, Rios JL, Smith SJ (2006) Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical trial. Plast Reconstr Surg 117:30–36
Ramos-Gallardo G (2016) How I can suspect of mycobacteria infection in breast implant surgery? World J Plast Surg 5:328–331
Liu J, Hou J, Li Z, Wang B, Sun J (2020) Efficacy of acellular dermal matrix in capsular contracture of implant-based breast reconstruction: a single-arm metanalysis. Aesth Plast Surg. https://doi.org/10.1007/s00266-019-01603-2
Hallberg H, Rafnsdottir S, Selvaggi G et al (2018) Benefits and risks with acellular dermal matrix (ADM) and mesh support in immediate breast reconstruction: a systematic review and metanalysis. J Plast Surg Hand Surg 52:130–147
Lee KT, Mun GH (2017) A meta-analysis of studies comparing outcomes of diverse acellular dermal matrices for implant-based breast reconstruction. Ann Plast Surg 79:115–123
Ho G, Nguyen J, Shahabi A, Hwang BH, Chan LS, Wong AK (2012) A systematic review and meta-analysis of complications associated with acellular dermal matrix-assisted breast reconstruction. Ann Plast Surg 68:346–356
Salzberg CA (2012) Focus on technique: one-stage implant-based breast reconstruction. Plast Reconstr Surg 130:95S-103S
Jansen LA, De Caigny P, Guay NA, Lineaweaver WC, Shokrollahi K (2013) The evidence-based for the acellular dermal matrix AlloDerm. Ann Plast Surg 70:587–594
Jansen LA, Macadam SA (2011) The use of AlloDerm in post- mastectomy alloplastic breast reconstruction: part I. A Syst Rev Plast Reconstr Surg 127:2232–2244
Nahabedian MY (2016) Prosthetic breast reconstruction with acellular dermal matrices: achieving predictability and reproducibility. Plast Reconstr Surg Glob Open 4:e698
Bondioli E, Fini M, Veronesi F et al (2012) Development and evaluation of a decellularized membrane from human dermis. J Tissue Eng Regen Med 8:325–336
Greig H, Roller J, Ziaziaris W, Van Laeken N (2019) A retrospective review of breast reconstruction outcomes comparing AlloDerm and DermaCELL. J Plast Rescontr Surg 22:19–26
Derderian CA, Karp NS, Choi M (2009) Wise-pattern breast reconstruction: modification using AlloDerm and a vascularized dermal-subcutaneous pedicle. Ann Plast Surg 62:528–532
Friedman HI, Talebagha S, Gilstrap J, Mujadzic M, Chen E (2019) Wise pattern direct to implant breast reconstruction: a review and improved outcomes using dermal matrix. Plast Reconstr Surg Glob Open 7:e2439. https://doi.org/10.1097/GOX.0000000000002439
Bonomi S, Sala L, Gennaro M, Ricci C, Cortinovis U (2019) Skin-reducing mastectomy and direct-to-implant breast reconstruction with submuscular-dermal mesh pocket. Ann Plast Surg 82:19–27
Kankam HKN, Hourston GJM, Forouhi P, Di Candia M, Wishart GC, Malata CM (2018) Combination of acellular dermal matrix with a de-epithelialized dermal flap during skin-reducing mastectomy and immediate breast reconstruction. Ann R Coll Surg Engl 100:e197–e202
Caputo GG, Marchetti A, Dalla Pozza E et al (2016) Skin-reducing breast reconstructions with prepectoral implant. Plast Reconstr Surg 137:1702–1705
Maruccia M, Elia R, Gurrado A et al (2020) Skin-reducing mastectomy and pre-pectoral breast reconstruction in large ptotic breast. Aesth Plast Surg. https://doi.org/10.1007/s00266-020-01616-2
Khalil HH, Malahias MN, Ashour T, Rhobaye S (2019) Nipple-sparing mastectomy and prepectoral implant /acellular dermal matrix wrap reconstruction in large ptotic breasts. Plast Reconstr Surg Glob Open 7:e2289. https://doi.org/10.1097/GOX.0000000000002289
Hammond DC, Capraro PA, Ozolins EB, Arnold JF (2002) Use of a skin-sparing reduction pattern to create a combination skin- muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg 110:206–211
Storm-Dickerson T, Sigalove N (2017) Prepectoral breast reconstruction: the breast surgeon’s perspective. Plast Reconstr Surg 140:43S-48S
Antony AK, Robinson EC (2019) An algorithmic approach to prepectoral direct- to-implant breast reconstruction: version 2.0. Plast Reconstr Surg 143:1311–1319
Yang JY, Kim CW, Lee JW, Kim SK, Lee SA, Hwang E (2019) Considerations for patient selection: prepectoral versus subpectoral implant-based breast reconstruction. Arch Plast Surg 46:550–557
Viezel-Mathieu A, Alnaif N, Aljerian A et al (2020) Acellular dermal matrix-sparing direct-to-implant prepectoral breast reconstruction: a comparative study including cost analysis. Ann Plast Surg 84:139–143
Cheng A, Saint-Cyr M (2012) Comparison of different ADM materials in breast surgery. Clin Plast Surg 39:167–175
Corban J, Shash H, Safran T, Sheppard-Jones N, Fouda-Neel O (2017) A systematic review of complications associated with direct implants versus tissue expanders following wise pattern skin-sparing mastectomy. J Plast Reconstr Aesth Surg 70:1191–1199
Manrique OJ, Banuelos J, Abu-Ghname A et al (2019) Surgical outcomes of prepectoral versus subpectoral implant-based breast reconstruction in young women. Plast Reconstr Surg Glob Open 7:e2119. https://doi.org/10.1097/GOX.0000000000002119
Manrique OJ, Kapoor T, Banuelos J et al (2020) Single-stage direct-to-implant breast reconstruction a comparison between prepectoral and subpectoral placement. Ann Plast Surg 84:361–365
Kobraei EM, Cauley R, Gadd M, Austen WG Jr, Liao EG (2016) Avoiding breast animation deformity with pectoralis-sparing subcutaneous direct-to-implant breast reconstruction. Plast Reconstr Surg Glob Open 4:e708. https://doi.org/10.1097/GOX.0000000000000681
Elswick SM, Harless CA, Bishop SN et al (2018) Prepectoral implant-based breast reconstruction with postmastectomy radiation therapy. Plast Reconstr Surg 142:1–12
Sinnot CJ, Persing SM, Pronovost M, Hodyl C, McConnell D, Young AO (2018) Impact of postmastectomy radiation therapy in prepectoral versus subpectoral implant-based breast reconstruction. Ann Surg Oncol 25:2899–2908
Bernini M, Calabrese C, Cecconi L et al (2015) Subcutaneous direct-to-implant breast reconstruction: surgical, functional, and aesthetic results after long-term follow-up. Plast Reconstr Surg Glob Open. https://doi.org/10.1097/GOX.0000000000000533
Baker BJ, Irri R, MacCallum V, Chattopadhyay R, Murphy J, Harvey JR (2018) A prospective comparison of short-term outcomes of subpectoral and prepectoral strattice-based immediate breast reconstruction. Plast Reconstr Surg 141:1077–1084
Zenn M, Venturi M, Pittman T et al (2017) Optimizing outcomes of postmastectomy breast reconstruction with acellular dermal matrix: a review of recent clinical data. Eplasty 17:e18
Funding
The authors received no financial support for the research, authorship and/or publication of this article. None of the author has financial interest to declare in relation to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Furthermore, for this type of study, formal consent is not required.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 171001 kb)
Rights and permissions
About this article
Cite this article
Marongiu, F., Bertozzi, N., Sibilio, A. et al. The First Use of Human-Derived ADM in Prepectoral Direct-to-Implant Breast Reconstruction after Skin-Reducing Mastectomy. Aesth Plast Surg 45, 2048–2057 (2021). https://doi.org/10.1007/s00266-021-02231-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-021-02231-5