Abstract
Background
Recent concerns regarding the association between macrotextured breast implants and anaplastic large cell lymphoma (ALCL) have led to renewed interest in the use of devices with less texturing. Smooth implants appear to have a decreased risk of ALCL; however, low implant adherence has led to questions about implant stabilization and bottoming-out. The senior author has used a split muscle support (SMS) technique to help support the implant infero-laterally in over 380 breast augmentations and augmentation–mastopexy using smooth implants, with a low complication and reoperation rate.
Methods
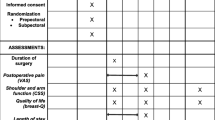
A retrospective chart review of 387 consecutive breast augmentation and augmentation–mastopexy patients operated on by the senior author over 24 months was performed. The SMS technique was classified in three grades according to amount of implant support by the pectoralis major muscle.
Results
Patients were followed for an average of 13 months. Major complications occurred in seven (1.9%) patients, of which five (1.4%) were considered implant-related. There were one case of implant rotation and three cases of malposition during the transition from microtexture to nanotexture implants and one case of capsular contracture in a previously irradiated breast. Three post-massive weight loss patients required reoperation for further skin adjustment, and one patient requested upsizing of her implants at 3 months.
Conclusions
The SMS technique is easily reproducible, adjustable intraoperatively according to patient characteristics, and helps stabilize breast implants. With increasing patient awareness regarding ALCL, the association of smooth implants along with the varying degrees of implant support afforded by SMS can help achieve a low complication and reoperation rate.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.




Similar content being viewed by others
References
International Society of Aesthetic Plastic Surgery. 2017 Global Statistics. https://www.isaps.org/medical-professionals/isaps-global-statistics/. Accessed 30 Sep 2019
Stutman RL, Codner M, Mahoney A, Amei A (2012) Comparison of breast augmentation incisions and common complications. Aesthetic Plast Surg 36:1096–1104
Tebbetts JB (2006) Achieving a zero percent reoperation rate at 3 years in a 50-consecutive-case augmentation mammaplasty premarket approval study. Plast Reconstr Surg 118:1453–1457
Stevens WG, Pacella SJ, Gear AJ et al (2008) Clinical experience with a fourth-generation textured silicone gel breast implant: a review of 1012 Mentor MemoryGel breast implants. Aesthet Surg J. 28:642–647
Codner MA, Mejia JD, Locke MB et al (2011) A 15-year experience with primary breast augmentation. Plast Reconstr Surg 127:1300–1310
Handel N, Cordray T, Gutierrez J, Jensen JA (2006) A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg 117:757–767 discussion 768
Somogyi RB, Brown MH (2015) Outcomes in Primary Breast Augmentation: a single surgeon's review of 1539 consecutive cases. Plast Reconstr Surg 135:87–97
Khan UD (2007) Muscle-splitting biplane breast augmentation. Aesthet Plast Surg 31:353–358
Baxter RA (2005) Subfascial breast augmentation: theme and variation. Aesthet Surg J 25:447–453
Sforza M, Hammond DC, Botti G et al (2019) Expert consensus on the use of a new bioengineered, cell-friendly, smooth surface breast implant. Aesthet Surg J 8(39):S95–S102
Sforza M, Zaccheddu R, Alleruzzo A, Seno A, Mileto D, Paganelli A, Sulaiman H, Payne M, Maurovich-Horvat L (2018) Preliminary 3-year evaluation of experience with silksurface and velvetsurface motiva silicone breast implants: a single-center experience with 5813 consecutive breast augmentation cases. Aesthet Surg J 15(38):S62–S73
Munhoz AM, Clemens MW, Nahabedian MY (2019) Breast implant surfaces and their impact on current practices: where we are now and where are we going? Plast Reconstr Surg Global Open 7(10):e2466
Cheffe MR, Valentini JD, Collares MVM, Piccinini PS, da Silva JLB (2018) Quantifying Dynamic Deformity After Dual Plane breast augmentation. Aesthetic Plast Surg 42(3):716–724
Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RCC, Auersvald A (2003) Subfascial breast implant: a new procedure. Plast Reconstr Surg 111(2):904–908
Lang Stumpfle R, Figueras Pereira-Lima L, Alves Valiati A et al (2012) Transaxillary muscle-splitting breast augmentation: experience with 160 cases. Aesthetic Plast Surg 36:343–348
Lang Stumpfle R, Piccinini PS, Pereira-Lima LF, Valiati AA (2019) Muscle-splitting augmentation-mastopexy: implant protection with an inferior dermoglandular flap. Ann Plast Surg 82:137–144
Daniel MJB (2005) Inclusion of the breast prosthesis in double space. Rev Soc Bras Cir Plást 20(2):82–87
Auersvald A, Auersvald LA (2011) Breast augmentation and mastopexy using a pectoral muscle loop. Aesthetic Plas Surg 35(3):333–340
Valente DS (2018) Reverse-muscle sling reduces complications in revisional mastopexy-augmentation. Aesthetic Plast Surg 42(4):1202
Funding
No funding from public, private or nonprofit organizations was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The senior author is a clinical instructor for Motiva Experts. The remaining authors declare no conflicts of interest in relation to the content of this manuscript.
Ethical Approval
The study was performed according to the Declaration of Helsinki for Research in Human Subjects and our institutional ethics standards.
Informed Consents
All patients signed informed consent for surgery, use of photographs and data for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MOV 28865 kb)
Supplementary material 2 (MOV 79262 kb)
Supplementary material 3 (MOV 92127 kb)
Supplementary material 4 (MP4 27826 kb)
Rights and permissions
About this article
Cite this article
Rigo, M.H., Piccinini, P.S., Sartori, L.D.P. et al. SMS—Split Muscle Support: A Reproducible Approach for Breast Implant Stabilization. Aesth Plast Surg 44, 698–705 (2020). https://doi.org/10.1007/s00266-019-01565-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-019-01565-5