Abstract
Purpose
The aim of this prospective, randomized, double-blind study was to compare the tumescent anesthesia method and erector spinae block with respect to postoperative analgesia consumption, pain scores and patient satisfaction, in patients receiving breast reduction surgery under general anesthesia.
Methods
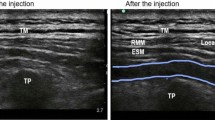
The study included 44 females, aged 20–65 years, who were to undergo breast reduction surgery, without adjunctive liposuction on the breast. Using the closed envelope method, the patients were randomly separated into two groups to receive tumescent anesthesia or erector spinae block (ESB). Patients in the ESB group received the block before general anesthesia by a single anesthetist (G.Ö.).
Results
The 24-h tramadol consumption with PCA, which was the primary outcome of the study, was determined to be statistically significantly less in the ESB group (p < 0.001). The NRS scores were compared at 30 min postoperatively and then at 1, 2, 4, 6, 12 and 24 h. At all the measured time points, the pain scores of the ESB group were statistically significantly lower (p < 0.001). Additional analgesia was required by one patient in the ESB group and by seven patients in the tumescent group and was applied as 1 g paracetamol. The requirement for additional analgesia was statistically significantly lower in the ESB group (p < 0.024). Patient satisfaction was statistically significantly better in the ESB group (p < 0.001).
Conclusions
According to the results of this study, bilateral ESB performed under ultrasound guidance in breast reduction surgery was more effective than tumescent anesthesia concerning postoperative analgesia consumption and pain scores. ESB could be an appropriate, effective and safe postoperative analgesia method for patients undergoing reduction mammoplasty surgery.
Level of Evidence II
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.


Similar content being viewed by others
References
Purohit S (2008) Reduction mammoplasty. Indian J Plast Surg 41(Suppl):64–79
Backstrom R, Rawal N (2008) Acute pain services—what it is, why it is and what is next. Eur J Pain 2:40–43
Baldini G, Carli F (2015) The current and future role of regional anaesthesia in enhanced recovery after surgery programs for abdominal surgery. Adv Anesth 33:39–59
Kang CM, Kim WJ, Yoon SH, Cho CB, Shim JS (2017) Postoperative pain control by intercostal nerve block after augmentation mammoplasty. Aesthetic Plast Surg 41(5):1031–1036
Salviz EA, Sivrikoz N, Ozonur A, Orhan-Sungur M, Savran-Karadeniz M, Altun D, Hocaoglu E, Celet-Ozden B, Tugrul KM (2017) Ultrasound-guided bilateral thoracic paravertebral blocks as an adjunct to general anesthesia in patients undergoing reduction mammaplasty: a historical cohort study. Plast Reconstr Surg 139(1):20e–28e. https://doi.org/10.1097/PRS.0000000000002842
Rosaeg OP, Bell M, Cicutti NJ, Dennehy KC, Lui AC, Krepski B (1998) Pre-incision infiltration with lidocaine reduces pain and opioid consumption after reduction mammoplasty. Reg Anesth Pain Med 23(6):575–579
O’Connor PJ, Moysa GL, Finucane BT (2001) Thoracic epidural anesthesia for bilateral reduction mammoplasty in a patient with Klippel–Feil syndrome. Anesth Analg 92(2):514–516
Paige KT, Bostwick J 3rd, Bried JT (2004) TRAM flap breast reconstruction: tumescent technique reduces blood loss and transfusion requirement. Plast Reconstr Surg 113(6):1645–1649
Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ (2016) The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med 41(5):621–627
Tulgar S, Balaban O (2018) Local anaesthetic injection point of erector spinae plane block. Indian J Anaesth 62(5):403–404
Ohgoshi Y, Ikeda T, Kurahashi K (2018) Continuous erector spinae plane block provides effective perioperative analgesia for breast reconstruction using tissue expanders: a report of two cases. J Clin Anesth 44:1–2
Kumar A, Hulsey A, Martinez-Wilson H, Kim J, Gadsden J (2018) The use of liposomal bupivacaine in erector spinae plane block to minimize opioid consumption for breast surgery: a case report. A A Pract 10(9):239–241
Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH, Kılıç CT (2018) Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth 50:65–68. https://doi.org/10.1016/j.jclinane.2018.06.033
Karaca O, Pınar HU, Arpacı E, Dogan R, Cok OY, Ahiskalioglu A (2018) The efficacy of ultrasound-guided type-I and type-II pectoral nerve blocks for postoperative analgesia after breast augmentation: a prospective, randomised study. Anaesth Crit Care Pain Med. https://doi.org/10.1016/j.accpm.2018.03.009
Khemka R, Chakraborty A, Ahmed R, Datta T, Agarwal S (2016) Ultrasound-guided serratus anterior plane block in breast reconstruction surgery. A A Case Rep 6(9):280–282
Christie BM, Kapur S, Kempton SJ, Hanson SE, Ma Y, Rao VK (2017) A prospective randomized trial comparing the effects of lidocaine in breast reduction surgery. Plast Reconstr Surg 139(5):1074e–1079e
Raj PP, Rosenblatt R, Miller J et al (1977) Dynamics of local-anesthetic compounds in regional anesthesia. Anesth Analg 56:110
Tulgar S, Kapakli MS, Senturk O, Selvi O, Serifsoy TE, Ozer Z (2018) Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth 49:101–106
Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E (2018) Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth 44:3–4
Adhikary SD, Bernard S, Lopez H, Chin KJ (2018) Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Reg Anesth Pain Med 1:1. https://doi.org/10.1097/aap.0000000000000798
Hamilton DL (2018) Pneumothorax following erector spinae plane block. J Clin Anesth 52:17. https://doi.org/10.1016/j.jclinane.2018.08.026
Ueshima H (2018) Pneumothorax after the erector spinae plane block. J Clin Anesth 48:12. https://doi.org/10.1016/j.jclinane.2018.04.009
Acknowledgements
All the authors declare that they have all participated in the design, execution and analysis of the paper and that they have approved the final version. Additionally, there are no conflicts of interest in connection with this paper, and the material described is not under publication or consideration for publication elsewhere.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oksuz, G., Bilgen, F., Arslan, M. et al. Ultrasound-Guided Bilateral Erector Spinae Block Versus Tumescent Anesthesia for Postoperative Analgesia in Patients Undergoing Reduction Mammoplasty: A Randomized Controlled Study. Aesth Plast Surg 43, 291–296 (2019). https://doi.org/10.1007/s00266-018-1286-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-018-1286-8