Abstract
Background
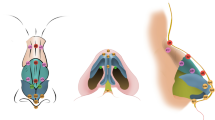
Protruding ears are the most common congenital ear deformity, with a frequency of 13.5%. Since 1845 and the first works of Dieffenbach, over 170 classical surgical methods have been proposed to correct it. We introduced laser-assisted cartilage reshaping (LACR) in 2004 as an alternative to invasive surgical otoplasty.
Methods
Between January 2008 and June 2008, 24 patients underwent LACR for treatment of bilateral ear protrusion. Fourteen adults and ten children were treated (mean age = 16.0 years, range = 6–45 years). No anesthesia was used. Both sides of the entire helix and the concha were irradiated using a 1540-nm laser connected to a 4-mm spot handpiece with integrated cooling. Fluences varying from 70 up to 84 J/cm2 were applied. Immediately after the irradiation, silicone elastomer was inserted inside the helix to give it the desired shape. After 3 minutes a solid mold was obtained. Patients were asked to keep this mold in place at all times with a bandage wrapped around the head for the first 3 weeks and then for an additional 3 weeks only during the night. A non-steroidal anti-inflammatory drug (NSAID) was prescribed to the patients for 3 days. At 1, 30, 60, and 90 days after the procedure, ears were checked and photographs were taken. Clinical follow-up at 1 year was obtained via direct patient contact or over the telephone.
Results
The treatment was well tolerated. No hematomas or skin necrosis occurred. Contact dermatitis was observed in four children and two adults as a result of inappropriate mold design. These patients stopped wearing the mold and the shape of their ear did not improve. For the remaining 18 patients (6 children and 9 adults), the expected ear reshaping was obtained (fluence was 84 J/cm2). For three other adults, incomplete reshaping of the ears was observed and can be correlated to a lower fluence (70 J/cm2).
Conclusion
LACR, performed without any anesthesia, is a safe and less morbid approach to surgical otoplasty.




Similar content being viewed by others
References
Dieffenbach JF (1845) Die operative chirurgie. Leipzi FA Brook-Haus, Wiesbaden
Luckett WH (1910) A new operation for prominent ears based on the anatomy of the deformity. Surg Gynecol Obstet 10:635–638
Mustarde JC (1967) Treatment of prominent ears by buried mattress sutures. Plast Reconstr Surg 4:382–386
Minderjahn A, Wolf R, Hildmann H (1980) Mustarde’s otoplasty. Evaluation of correlation between clinical and statistical findings. J Maxillofac Surg 8:241–250
Morestin H (1903) De la reposition et du plissement cosmétiques du pavillon de l’oreille. Rev Ortho Chir Appar Mot 4:289
Becker OJ (1952) Correction of the protruding deformed ears. Br J Plast Surg 5:187
Stenström S (1967) A simple operation for prominent ears. Acta Otolaryngol Suppl 224:393+
Limandjaja GC, Breugem CC, Mink van der Molen AB, Kon M (2009) Complications of otoplasty: a literature review. J Plast Reconstr Aesthet Surg 62(1):19–27
Mordon S, Wang T, Fleurisse L, Creusy C (2004) Laser cartilage reshaping in an in vivo rabbit model using a 1.54 micron Er:glass laser. Lasers Surg Med 34(4):315–322
Jones N, Sviridov A, Sobol E, Omelchenko A, Lowe J (2001) A prospective randomised study of laser reshaping of cartilage in vivo. Lasers Med Sci 16(4):284–290
Trelles MA, Mordon S (2006) Correction of ear malformations by laser-assisted cartilage reshaping (LACR). Lasers Surg Med 38:659–662
Helidonis E, Sobol E, Kavvalos G, Bizakis J, Christodoulou P, Velegrakis G, Segas J, Bagratashvili V (1993) Laser shaping of composite cartilage grafts. Am J Otolaryngol 14:410–412
Sobol E, Bagratashvili NV, Omel’chenko A, Sviridov A (1994) Laser shaping of cartilage. In: Anderson RR, Katzir A (eds) Laser surgery: advanced chararcterization, therapuetics, and systems, 4th ed, vol 2128. SPIE, Bellingham, WA, pp 43–49
Bagratashvili NV, Bagratashvili VN, Gapontsev VP, Makhmutova G, Minaev VP, Omel’chenko A, Samartsev IE, Sviridov A, Sobol E, Tsypina SI (2001) Change in the optical properties of hyaline acrtilage heated by the near-IR laser radiation. Quantum Electron 31:534–538
Sviridov AP, Sobol EN, Bagratashvili VN, Omel’chenko AI, Ovchinnikov YM, Shekhter A, Svistushkin V, Shinaev AA, Nikiforova G, Jones N et al (1999) In vivo study and histological examination of laser reshaping of cartilage. In: Anderson RR (ed) Lasers in surgery: Advanced characterization, therapeutics, and systems, vol 3590, 9th edn. SPIE, Bellingham, WA, pp 222–228
Aksan A, McGrath JJ (2002) Quantitative determination of subablative thermal exposure producing optimal response of collagenous tissues. In: Jacques SL, Duncan DD, Kirkpatrick SJ, Kriete A (eds) Laser–tissue interaction XIII: Photochemical, photothermal, and photomechanical, vol 4617. SPIE, Bellingham, WA, pp 87–96
Bos PK, van Osch GJ, Frenz DA, Verhaar JA, Verwoerd-Verhoef HL (2001) Growth factor expression in cartilage wound-healing: temporal and spatial immunolocalization in a rabbit auricular cartilage wound model. Osteoarthritis Cartilage 9:382–389
Capon A, Mordon S (2003) Can thermal lasers promote skin wound healing? Am J Clin Dermatol 4:1–12
Tiffee JC, Griffin JP, Cooper LF (2000) Immunolocalization of stress proteins and extracellular matrix proteins in the rat tibia. Tissue Cell 32:141–147
Watson AT, Visram A (2003) Children’s preoperative anxiety and postoperative behaviour. Paediatr Anaesth 13(3):188–204
Jemec BI, Jemec GBE (2002) Braces for postoperative bandage after otoplasty. Aesthetic Plast Surg 26:156–158
Tan ST, Shibu M, Gault DT (1994) A splint for correction of congenital ear deformities. Br J Plast Surg 47:575–578
Jeffery SL (1999) Complications following correction of prominent ears: an audit review of 122 cases. Br J Plast 52(7):588–590
Acknowledgment
The authors thank Pascal Servell for checking the manuscript for English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leclère, F.M.P., Petropoulos, I. & Mordon, S. Laser-Assisted Cartilage Reshaping (LACR) for Treating Ear Protrusions: A Clinical Study in 24 Patients. Aesth Plast Surg 34, 141–146 (2010). https://doi.org/10.1007/s00266-009-9353-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-009-9353-9