Abstract
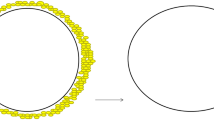
Introduction: Breast augmentation has enjoyed worldwide acceptance in the last few decades. In order to optimize the outcomes of this operation, numerous variables such as incision location, pocket plane, implant design, and materials, and individual tissue characteristics must be carefully considered. Although no combination of choices may be considered superior, satisfactory results depend on adjusting the available options to each patient’s requirements. In this paper, the authors present a seven-year experience with augmentation mammaplasty using the subfascial plane, analyzing important aspects of surgical technique, benefits and trade-offs when compared to other approaches, and the resulting outcomes. Method: A total of 241 primary and secondary breast augmentation procedures were performed over a seven-year period, employing anatomical high-cohesivity gel textured implants (McGhan 410 Style). After choosing the appropriate approach and performing the skin incision, dissection proceeds parallel to the skin (as in skin-sparing mastectomies) for approximately 4 cm. The breast’s parenchyma is then incised in a radial direction (perpendicular to the skin incision) and vertically until the fascial layer is reached. Dissection of the implant’s pocket is then performed in the well-defined subfascial plane. After insertion of the implants, the distance between the areola’s inferior border and the inframammary fold should be approximately equal to 6–7 cm (or X). The distance between the areola’s superior border and the uppermost point of the breast should be approximately equal to 9–10.5 cm (or 1.5X). Another important parameter is the distance between the implants, which should be approximately 2–3 cm. Finally, the distance between the areola’s medial border and the midsternal line should be about 9–10 cm. Postoperative care issues are specified. Results: Pleasing long-term results have been obtained, with maintenance of a natural breast shape, a smooth transition between the soft tissues and implant in the upper pole, and low morbidity. The rate of capsular contracture was extremely low and there were no complaints regarding displacement of the implants with contraction of the pectoralis major muscle. Conclusion: The presented technique offers improved long-term aesthetic results due to the creation of a stronger supporting system for the implant’s superior pole. This tends to keep the implant’s upper third from altering its shape and position over time and combines the potential benefits of the subglandular approach with the improvements that may be achieved by having more tissue available to cover the implant’s upper pole. The trade-offs of the subpectoral approach have been significantly reduced and factors such as morbidity and postoperative recovery are acceptable. The presented technique is extremely versatile and may also be used in patients requiring removal and replacement of breast implants.






Similar content being viewed by others
References
A Barnett (1990) ArticleTitleTransaxillary subpectoral augmentation in the ptotic breast: Augmentation by disruption of the extended pectoral fascia and parenchymal sweep. Plast Reconstr Surg 86 76
TM Biggs RS Yarish (1988) ArticleTitleAugmentation mammaplasty: Retropectoral versus retromammary implantation. Clin Plast Surg 15 549 Occurrence Handle1:STN:280:BiaC3snkt1A%3D Occurrence Handle3224480
WC Dempsey WD Latham (1968) ArticleTitleSubpectoral implants in augmentation mammaplasty: Preliminary report. Plast Reconstr Surg 42 515
RM Graf et al. (2000) ArticleTitleSubfascial endoscopic transaxillary augmentation mammaplasty. Aesthetic Plast Surg 24 216
H Gray (1989) Gray’s anatomy, 37th edition. Longman Group UK Limited London
DA Hidalgo (2000) ArticleTitleBreast augmentation: Choosing the optimal incision, implant, and pocket plane. Plast Reconstr Surg 105 2202 Occurrence Handle1:STN:280:By%2BD2s%2FitFY%3D Occurrence Handle2686121
D Mahler J Ben-Yakar DJ Hauben (1982) ArticleTitleThe retropectoral route for breast augmentation. Aesthetic Plast Surg 6 237
J Papillon (1976) ArticleTitlePros and cons of subpectoral implantation. Clin Plast Surg 3 321
CL Puckett et al. (1987) ArticleTitleA critical look at capsular contracture in subglandular versus subpectoral mammary augmentation. Aesthetic Plast Surg 11 23
P Regnault (1977) ArticleTitlePartially submuscular breast augmentation. Plast Reconstr Surg 59 72
JB Tebbetts (1984) ArticleTitleTransaxillary subpectoral augmentation mammaplasty: Long-term follow-up and refinements. Plast Reconstr Surg 74 636
JB Tebbetts (2001) ArticleTitleDual plane breast augmentation: Optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg 107 1255
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Góes, J., Landecker, A. Optimizing Outcomes in Breast Augmentation: Seven Years of Experience with the Subfascial Plane . Aesth. Plast. Surg. 27, 178–184 (2003). https://doi.org/10.1007/s00266-003-0004-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-003-0004-2