Abstract
Purpose
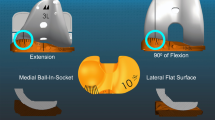
For a new tibial insert design with ball-in-socket (B-in-S) medial conformity (MC), posterior cruciate ligament (PCL) retention, and flat lateral articular surface (B-in-S MC + PCL), this study determined whether internal tibial rotation and knee flexion were limited and clinical outcome scores were lower during weight-bearing activities relative to an insert with intermediate (I) (i.e., less than ball-in-socket) medial conformity (I MC + PCL).
Methods
Twenty-five patients were treated with bilateral unrestricted, caliper-verified kinematic alignment (KA) total knee arthroplasty (TKA) with an I MC + PCL insert and B-in-S MC + PCL insert in opposite knees. Each patient performed weight-bearing deep knee bend, step up, and chair rise under single-plane fluoroscopy. Analysis following 3D model-to-2D image registration determined internal tibial rotation. For each TKA, knee flexion was measured and patients completed clinical outcome scoring questionnaires.
Results
Internal tibial rotation did not differ between conformities during chair rise and step up (p = 0.3419 and 0.1030, respectively). During deep knee bend, internal tibial rotation between 90° and maximum flexion was 3° greater in the B-in-S MC + PCL group (18° vs 15°) (p = 0.0290). Mean knee flexion (p = 0.3115) and median Forgotten Joint Score (FJS), Oxford Knee Score (OKS), and Western Ontario and McMasters Universities Arthritis Index (WOMAC) scores (p = 0.2100, 0.2154, and 0.4542, respectively) did not differ between conformities.
Conclusion
An insert with ball-in-socket medial conformity, which maximizes anteroposterior (AP) stability, did not limit internal tibial rotation and knee flexion and did not lower patient-reported outcomes when implanted with unrestricted caliper-verified KA and PCL retention. The high AP stability provided by the medial ball-in-socket might interest those surgeons exploring the treatment of the active patient with a desire to return to high-level and athletic activities.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
MacDessi SJ, Griffiths-Jones W, Chen DB, Griffiths-Jones S, Wood JA, Diwan AD, Harris IA (2020) Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint J 102-B:117–124. https://doi.org/10.1302/0301-620X.102B1.BJJ-2019-0674.R2
The New Zealand Joint Registry 18 Year Report: January 1999 to December 2016.
Lynch JT, Scarvell JM, Galvin CR, Smith PN, Perriman DM (2021) Influence of component design on in vivo tibiofemoral contact patterns during kneeling after total knee arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 29:446–466. https://doi.org/10.1007/s00167-020-05949-y
Pritchett JW (2011) Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty 26:224–228. https://doi.org/10.1016/j.arth.2010.02.012
Sabatini L, Risitano S, Parisi G, Tosto F, Indelli PF, Atzori F, Masse A (2018) Medial pivot in total knee arthroplasty: literature review and our first experience. Clin Med Insights Arthritis Musculoskelet Disord 11:1–4. https://doi.org/10.1177/1179544117751431
Gray HA, Guan S, Young TJ, Dowsey MM, Choong PF, Pandy MG (2020) Comparison of posterior-stabilized, cruciate-retaining, and medial-stabilized knee implant motion during gait. J Orthop Res 38:1753–1768. https://doi.org/10.1002/jor.24613
Moonot P, Mu S, Railton GT, Field RE, Banks SA (2009) Tibiofemoral kinematic analysis of knee flexion for a medial pivot knee. Knee Surg Sports Traumatol Arthrosc 17:927–934. https://doi.org/10.1007/s00167-009-0777-1
Moonot P, Shang M, Railton GT, Field RE, Banks SA (2010) In vivo weight-bearing kinematics with medial rotation knee arthroplasty. Knee 17:33–37. https://doi.org/10.1016/j.knee.2009.06.009
Shimmin A, Martinez-Martos S, Owens J, Iorgulescu AD, Banks S (2015) Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. Knee 22:522–526. https://doi.org/10.1016/j.knee.2014.11.011
Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM (2017) Do medial pivot kinematics correlate with patient-reported outcomes after total knee arthroplasty? J Arthroplasty 32:2411–2416. https://doi.org/10.1016/j.arth.2017.03.019
Dowsey MM, Gould DJ, Spelman T, Pandy MG, Choong PF (2020) A randomized controlled trial comparing a medial stabilized total knee prosthesis to a cruciate retaining and posterior stabilized design: a report of the clinical and functional outcomes following total knee replacement. J Arthroplasty 35:1583-1590 e1582. https://doi.org/10.1016/j.arth.2020.01.0850
Delman CM, Ridenour D, Howell SM, Hull ML (2021) The posterolateral upslope of a low-conforming insert blocks the medial pivot during a deep knee bend in TKA: a comparative analysis of two implants with different insert conformities. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06668-8.10.1007/s00167-021-06668-8
Nedopil AJ, Howell SM, Hull ML (2021) More passive internal tibial rotation with posterior cruciate ligament retention than with excision in a medial pivot TKA implanted with unrestricted caliper verified kinematic alignment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06840-0
Kayani B, Konan S, Horriat S, Ibrahim MS, Haddad FS (2019) Posterior cruciate ligament resection in total knee arthroplasty: the effect on flexion-extension gaps, mediolateral laxity, and fixed flexion deformity. Bone Joint J 101-B:1230–1237. https://doi.org/10.1302/0301-620X.101B10.BJJ-2018-1428.R2
Nowakowski AM, Majewski M, Muller-Gerbl M, Valderrabano V (2012) Measurement of knee joint gaps without bone resection: “physiologic” extension and flexion gaps in total knee arthroplasty are asymmetric and unequal and anterior and posterior cruciate ligament resections produce different gap changes. J Orthop Res 30:522–527. https://doi.org/10.1002/jor.21564
Freeman MA, Pinskerova V (2005) The movement of the normal tibio-femoral joint. J Biomech 38:197–208. https://doi.org/10.1016/j.jbiomech.2004.02.006
Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MA (2004) Does the femur roll-back with flexion? J Bone Joint Surg Br 86:925–931
Nedopil AJ, Singh AK, Howell SM, Hull ML (2018) Does calipered kinematically aligned TKA restore native left to right symmetry of the lower limb and improve function? J Arthroplasty 33:398–406
Rivière C, Iranpour F, Harris S, Auvinet E, Aframian A, Chabrand P, Cobb J (2017) The kinematic alignment technique for TKA reliably aligns the femoral component with the cylindrical axis. Orthop Traumatol 103:1069–1073. https://doi.org/10.1007/s00167-019-05776-w
Nedopil AJ, Zamora T, Shelton T, Howell SM, Hull M (2021) A best-fit of an anatomic tibial baseplate closely parallels the flexion-extension plane and covers a high percentage of the proximal tibia. J Knee Surg 34:1486–1494. https://doi.org/10.1055/s-0040-1710367
Nedopil AJ, Howell SM, Hull ML (2020) Deviations in femoral joint lines using calipered kinematically aligned TKA from virtually planned joint lines are small and do not affect clinical outcomes. Knee Surg Sports Traumatol Arthrosc 28:3118–3127. https://doi.org/10.1007/s00167-019-05776-w
Johnson JM, Mahfouz MR, Midillioglu MR, Nedopil AJ, Howell SM (2017) Three-dimensional analysis of the tibial resection plane relative to the arthritic tibial plateau in total knee arthroplasty. J Exp Orthop 4:27. https://doi.org/10.1186/s40634-017-0099-z
Burton WS, Myers CA, Jensen A, Hamilton L, Shelburne KB, Banks SA, Rullkoetter PJ (2021) Automatic tracking of healthy joint kinematics from stereo-radiography sequences. Comput Biol Med 139:104945. https://doi.org/10.1016/j.compbiomed.2021.104945
Pourtabib J (2022) Error analysis of methods for determining tibiofemoral kinematics in the native knee and after total knee arthroplasty: an in vivo study using single plane fluoroscopy during weight-bearing deep knee bend. In: MS Thesis in Biomedical Engineering, University of California Davis.
Escamilla RF (2001) Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc 33:127–141. https://doi.org/10.1097/00005768-200101000-00020
Elbuluk AM, Jerabek SA, Suhardi VJ, Sculco PK, Ast MP, Vigdorchik JM (2022) Head-to-head comparison of kinematic alignment versus mechanical alignment for total knee arthroplasty. J Arthroplasty 37:S849–S851. https://doi.org/10.1016/j.arth.2022.01.052
Scott DF, Gray CG (2022) Outcomes are better with a medial-stabilized vs a posterior-stabilized total knee implanted with kinematic alignment. J Arthroplasty 37:S852–S858. https://doi.org/10.1016/j.arth.2022.02.059
Harman MK, Banks SA, Hodge WA (2001) Polyethylene damage and knee kinematics after total knee arthroplasty. Clin Orthop Relat Res 383–393. https://doi.org/10.1097/00003086-200111000-00050
Nilsson KG, Karrholm J, Ekelund L, Magnusson P (1991) Evaluation of micromotion in cemented vs uncemented knee arthroplasty in osteoarthrosis and rheumatoid arthritis. Randomized study using roentgen stereophotogrammetric analysis. J Arthroplasty 6:265–278. https://doi.org/10.1016/s0883-5403(06)80174-9
Gudnason A, Adalberth G, Nilsson KG, Hailer NP (2017) Tibial component rotation around the transverse axis measured by radiostereometry predicts aseptic loosening better than maximal total point motion. Acta Orthop 88:282–287. https://doi.org/10.1080/17453674.2017.1297001
Hull ML, Nicolet-Petersen S, Saiz A, Delman C, Howell SM (2022) Posterior rim loading of a low-conforming tibial insert in unrestricted kinematic alignment is caused by rotational alignment of an asymmetric baseplate designed for mechanical alignment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06994-5
Nakamura S, Sharma A, Ito H, Nakamura K, Zingde SM, Komistek RD (2015) Kinematic difference between various geometric centers and contact points for tri-condylar bi-surface knee system. J Arthroplasty 30:701–705. https://doi.org/10.1016/j.arth.2014.11.020
Niesen AE, Garverick AL, Howell SM, Hull ML (2022) Low tibial baseplate migration 1 year after unrestricted kinematically aligned total knee arthroplasty using a medial conforming implant design. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07171-4
Howell SM, Nedopil AJ, Hull ML (2022) Negligible effect of surgeon experience on the accuracy and time to perform unrestricted caliper verified kinematically aligned TKA with manual instruments. Knee Surg Sports Traumatol Arthrosc 30:2966–2974. https://doi.org/10.1007/s00167-022-06939-y
Nedopil AJ, Dhaliwal A, Howell SM, Hull ML (2022) A surgeon that switched to unrestricted kinematic alignment with manual instruments has a short learning curve and comparable resection accuracy and outcomes to those of an experienced surgeon. J Pers Med 12. https://doi.org/10.3390/jpm12071152
Bansal A, Loucks DG, Greenhow R, Swann RP (2022) Calipered kinematic alignment using patient specific instrumentation. In: Howell SM, Bini SA, Steele GD (eds) Calipered kinematically aligned total knee arthroplasty. Elsevier, Philadelphia. 29–38. https://doi.org/10.1016/C2018-0-05402-X
Calliess T, Christen B (2022) Kinematic alignment with image-based robotic instrumentation. In: Howell SM, Bini SA, Steele GD (eds) Calipered kinematic alignment total knee arthroplasty. Elsevier, Philadephia. pp. 50–59. https://doi.org/10.1016/C2018-0-05402-X
McEwen PJ (2022) Calipered kinematic alignment with navigation instrumentation. In: Howell SM, Bini SA, Steele GD (eds) Calipered kinematically aligned total knee arthroplasty. Elsevier, Philadelphia. pp. 39–49. https://doi.org/10.1016/C2018-0-05402-X
Gao ZX, Long NJ, Zhang SY, Yu W, Dai YX, Xiao C (2020) Comparison of kinematic alignment and mechanical alignment in total knee arthroplasty: a meta-analysis of randomized controlled clinical trials. Orthop Surg 12:1567–1578. https://doi.org/10.1111/os.12826
Funding
M. L. Hull received research support from Medacta USA, Inc. and the Orthopaedic Research and Education Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of the University of California Davis (IRB# 1385598–6).
Consent to participate
The text states that consent was obtained from all subjects who participated in the study.
Consent for publication
All authors contributed substantively to this study. Material preparation, data collection, and analysis were performed by S. P. Elorza, E. O’Donnell, and A. Nedopil. The first draft of the manuscript was written by S. P. Elorza. M. L. Hull and S. M. Howell extensively revised the first draft. All authors read and approved the final manuscript.
Conflict of interest
S. M. Howell receives royalties from Medacta and is a paid consultant for Medacta. M. L. Hull receives research support from Medacta USA, Inc. and from the Orthopaedic Research and Education Foundation. M. L. Hull is on the Editorial Board of the Journal of Biomechanics. E. O’Donnell owns stock in Novocure. A. Nedopil receives royalties and is a paid consultant for Medacta.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Elorza, S.P., O’Donnell, E., Nedopil, A. et al. Ball-in-socket medial conformity with posterior cruciate ligament retention neither limits internal tibial rotation and knee flexion nor lowers clinical outcome scores after unrestricted kinematically aligned total knee arthroplasty. International Orthopaedics (SICOT) 47, 1737–1746 (2023). https://doi.org/10.1007/s00264-023-05834-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05834-6