Abstract
Purpose
This study aims to assess the clinical presentation and surgical outcomes of lacertus syndrome (LS) and concomitant median nerve entrapments.
Methods
A retrospective study of prospectively collected data was conducted on patients undergoing lacertus release (LR) from June 2012 to June 2021. Available DASH (Disability of the Arm Shoulder Hand questionnaire) scores and post-operative Visual Analogue Scale (VAS) of pain, numbness, subjective satisfaction with surgical outcome, and intra-operative return of strength were analyzed.
Results
Two-hundred-seventy-five surgical cases were identified of which 205 cases (74.5%) underwent isolated LR, and 69 cases (25.1%) concomitant lacertus and carpal tunnel release. The three most common presenting symptoms in LS patients were loss of hand strength (95.6%), loss of hand endurance/fatigue (73.3%), and forearm pain (35.4%). Numbness in the median nerve territory of the hand was found in all patients with combined LS and carpal tunnel syndrome. Quick-DASH significantly improved (pre-operative 34.4 (range 2.3–84.1) to post-operative 12.4 (range 0–62.5), p < 0.0001) as did work and activity DASH (p < 0.0001). The postoperative VAS scores were pain VAS 1.9 and numbness VAS 1.8. Eighty-eight percent of patients reported good/excellent satisfaction with the surgical outcome. Intra-operative return of strength was verified in 99.2% of cases.
Conclusion
LS is a common median nerve compression syndrome typically presenting with loss of hand strength and hand endurance/fatigue. Minimally invasive LR immediately restores hand strength, significantly improves DASH scores, and yields positive outcomes regarding VAS pain, numbness, and subjective satisfaction with surgery in patients with proximal median nerve entrapment at a minimum six month follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal median nerve entrapment (PMNE) has attracted the interest of hand surgeons over the last decade [1]. Henrik Seyffarth first described it as pronator syndrome in 1951 [2], a nerve compression between the humeral and ulnar head of the pronator teres muscle, usually presenting a fibrous band between them. However, recent research has challenged which structure is primarily responsible for compression and the extent of the surgical release required to relieve symptoms [3, 4].
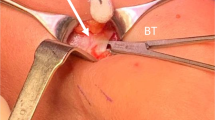
The lacertus fibrosus (LF) is an aponeurosis originating from the medial border of the distal biceps brachialis tendon, directed medially and distally, and in direct contact with the median nerve in almost half of individuals, crossing over the common flexor muscle mass and blending with its fascia [5, 6] (Fig. 1). Its dynamic biomechanical role in force transmission during elbow flexion, lever arm adjustment, and supination restraint could also explain its dynamic compression over the median nerve [4, 5]. In fact, due to the nerve topography and dynamic nature of entrapment caused by the LF, commonly known as lacertus syndrome (LS), its symptomatology often goes unnoticed [7, 8].
Anatomy of the lacertus fibrosus, also known as the bicipital aponeurosis, expanding from the common distal tendon of the biceps brachii (BT) to cross over the proximal flexor-pronator teres (PT) mass. The brachial artery and median nerve pass under the lacertus fibrosus at the level of the cubital fossa
Additionally, the literature on concomitant carpal tunnel syndrome (CTS) and PMNE remain scarce, reporting a prevalence ranging from 6 to 13% [9,10,11]. The underdiagnosis of the LS and the unsatisfactory outcomes after carpal tunnel release in double-crush syndromes demand an in-depth analysis of this entity’s current diagnostic and treatment approach [1, 11]. The aim of this study was to assess the clinical presentation and surgical outcomes of LS and concomitant median nerve entrapments.
Materials and methods
This study involving human participants was in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. Ethics committee approval and due consent were also obtained. A retrospective study of prospectively collected data was conducted on the patient registry from June 2012 to June 2021. Patients were included for final evaluation if they had undergone surgical decompression of the median nerve at the level of the LF (lacertus release), with or without simultaneous concomitant carpal tunnel or other median nerve releases. Patients surgically treated with concomitant peripheral nerve compressions other than the median nerve were excluded.
Medical charts were reviewed, and data on sex, age, occupation, hand dominance, reported subjective symptoms, surgical treatment, and intra-operative return of strength were collected. Available pre-and post-operative quick-DASH (Disability of the Arm Shoulder Hand questionnaire) with work and activity sub-scores and post-operative Visual Analogue Scale (VAS) of pain, numbness, subjective satisfaction with the surgical outcome, and intra-operative return of strength were analyzed.
Lacertus syndrome diagnosis
The diagnosis of LS was based on thorough patient history and clinical examination, including the previously described clinical triad of combining upper extremity manual muscle testing revealing weakness in the flexor carpi radialis (FCR), flexor pollicis longus (FPL), and flexor digitorum profundus to the index finger (FDP II), provocative sensory testing (scratch collapse test, SCT), and the presence of pain and/or positive Tinel’s test at the level of nerve compression (Online Resource 1) [4]. For the LS, pain is present at the level of the median nerve under the LF. Concomitant CTS was defined by a positive Tinel’s test and other provocative maneuvers. No electromyographic studies were implemented in diagnosing LS.
Surgical technique
Decompression of the median nerve at the level of the LF (lacertus release) followed a technique previously described [4] (Fig. 2). It was performed under wide-awake, local anaesthesia, and no tourniquet (WALANT) whenever feasible [12, 13]. The advantage of doing this procedure in an awake and cooperative patient is that intra-operative return of muscle power can be monitored, and possible further release if required, can be done immediately.
Illustration of the minimally invasive surgical technique for lacertus release. a 20–30 cc of 1% lidocaine-epinephrine solution is injected subcutaneously over the course of the lacertus fibrosus; b a 1.5–2-cm transverse skin incision is placed over the lacertus fibrosus, in the ulnovolar, and proximal aspect of the forearm; c following blunt dissection to forearm fascia, the lacertus fibrosus is easily identified and divided
Outcome measures
Outcome measures were prospectively collected via post six months post-operatively by an investigator outside the surgical team. A second letter was sent nine months post-operatively if no answer was retrieved after the first. The primary outcomes were the pre- and post-operative quick-DASH with work and activity sub-scores. The DASH questionnaire is a validated tool for standard assessment of the impact on the function of various musculoskeletal diseases and injuries in the upper extremity; scores range from 0 to 100, with higher ranking indicating worse symptoms [14, 15]. Secondary outcomes included the post-operative VAS for pain, numbness, subjective satisfaction with the surgery (VAS 0-10) [4], and intra-operative return of strength.
Statistical analyses
Pre-operative and post-operative scores were compared using paired two-tailed Student’s t-test. P values of < 0.05 were considered statistically significant. SPSS V.19 was used to perform statistical analysis. Results were presented as mean, ranges, median, and interquartile ranges.
Results
A total of 388 lacertus releases were identified in the ten year period. The final cohort included 275 lacertus releases in 245 patients after excluding patients who underwent simultaneous nerve decompressions of other nerves (radial nerve, N = 77; ulnar nerve, N = 39 patients). Of these, 205 cases (74.5%) were isolated lacertus release, 69 cases (25.1%) were concomitant lacertus and carpal tunnel release, and one had concomitant lacertus and median nerve release at the superficialis arcade. Twenty-six patients (12.7%) who underwent isolated lacertus release had prior carpal tunnel release with incomplete resolution of symptoms. Patients’ demographics are summarized in Table 1.
Presenting symptoms
The three most common presenting symptoms in LS patients were loss of hand strength (95.6%), loss of hand endurance/fatigue (73.3%), and forearm pain (35.4%) (Fig. 3). Numbness in the median nerve territory of the hand was found in all patients with combined LS and CTS. In contrast, only 10% of the patients with LS without previous history of carpal tunnel release presented with numbness, mainly within the palmar branch of the median cutaneous nerve or at the tips of the first to third digits.
Presenting symptoms of lacertus syndrome (top) and combined lacertus and carpal tunnel syndromes (bottom). The three most common presenting symptoms in lacertus syndrome patients were loss of hand strength (95.6%), loss of hand endurance/fatigue (73.3%), and forearm pain (35.4%). Numbness in the median nerve territory of the hand was found in all of the patients with combined lacertus and carpal tunnel syndromes
Surgical outcomes
Pre-operative quick-DASH with work and activity sub-scores were obtained from 227 patients. Of these, 136 patients (60%) completed the post-operative follow-up questionnaires. The average pre-operative quick DASH was 34.4 (range 2.3–84.1), work DASH 34.2 (0–100), and activity DASH 53.8 (range 0–100). The average post-operative quick DASH was 12.4 (range 0–62.5, mean difference 22), which is a statistically significant reduction (p < 0.0001). Similarly, the work and activity DASH subscores were significantly reduced (p < 0.0001) to 8.4 (0–75) and 19.5 (0–68.7), respectively (Fig. 4).
Box-and-whisker plots showing the results of pre-operative and post-operative quick-DASH, work-DASH, and activity-DASH scores. The boxes show the median and interquartile range, and the whiskers show the 25th and 75th percentiles. Cross marks the average, and dot indicates outliers outside the whiskers. ***Statistically significant changes in pre- and post-operative scores (p < 0.0001)
The mean post-operative VAS scores were as follows: pain VAS 1.9; numbness VAS 1.8; satisfaction with the surgical outcome VAS 8.5. Eighty-eight percent of patients reported good/excellent satisfaction with the surgical outcome. Only four patients were unsatisfied with the surgical outcome (1.6%), all of whom were later found to have a residual median nerve compression at the superficialis arcade that required revision surgery.
Two hundred fifty cases (91%) were done using WALANT anaesthesia which allows immediate evaluation of return of power in the FCR, FPL, and FDP II following lacertus release (Online Resource 2). Intraoperative return of strength was verified in 99.2% (248) of the patients. The two where power was not back on the table were with a complete palsy of the anterior interosseous nerve (FPL and FDP II palsy), and power was restored within eight weeks after surgery.
Discussion
The main findings of this study are that median nerve compression at the LF is a common entrapment syndrome and that lacertus release significantly improves quick-DASH score and subscores, VAS pain, numbness, and subjective satisfaction with the surgery at a minimum six month follow-up. Furthermore, it immediately restores hand strength in 99.2% of the patients.
Systematic clinical examination of strength in peripheral nerve entrapments has yielded a higher prevalence of dynamic compressions with no electromyographic changes (Sunderland zero compression neuropathies) and should thus be performed routinely [16,17,18,19,20,21]. The results of the present study show that patients with isolated LS typically present with complaints of loss of hand strength and loss of hand endurance/fatigue. The presence of associated median territory numbness ought to raise suspicion about concomitant CTS.
Correspondingly, patients with incomplete symptomatic relief after carpal tunnel release should be assessed to rule out concomitant LS, as they represented a not negligible 12.7% of the cases in this series. Other authors, like Binder et al. [16], found in a retrospective cohort study comprising 26 patients with pronator syndrome that 38.5% had a previous history of carpal tunnel release. Similarly, El-Haj et al. [18], in their retrospective study, including 27 patients with PMNE release, reported the same scenario in 48% of them. The wide range prevalence of unsatisfactory symptom relief after carpal tunnel release among these series can be explained by the lack of standardized diagnostic pathways, as the resulting PMNE motor deficit continues to be underdiagnosed and differential diagnoses still focus on the sensory deficits missing primary double-crush syndromes [10, 22].
Previous studies on PMNE have yielded satisfactory surgical outcomes. Binder et al. reported significant DASH (preop 48.7 ± 15.5 to postop 22.8 ± 18.4, p < 0.01) and VAS score (preop 8 ± 1 to postop 0.7 ± 1.4, p < 0.01) improvement after open PMNE release in twelve patients at a mean 75 months follow-up. Lee et al. [23] had similar outcomes implementing endoscopically assisted pronator syndrome decompression in 12 patients with an average of 51 points DASH score improvement (preop 57 to postop 6, p < 0.05) at a mean 22 months follow-up. Similarly, Apard et al. [17] presented a prospective cohort study of 15 patients undergoing ultrasound-guided percutaneous lacertus release, showing significant VAS score improvement (preop 6.2 to postop 0.6, p < 0.001) at four weeks post-operatively and immediate post-operative muscle power restoration in all patients.
The present study shows comparable outcomes by implementing an isolated mini-open lacertus release and exceeding the minimum clinically important difference in the quick-DASH score [24, 25]. However, it is still debatable which is the primary structure responsible for PMNE, with the lack of studies comparing surgical approaches partaking in it. This study contributes to this debate by revealing an immediate post-operative return of strength in 99.2% of the patients through the isolated release of the LF, thus highlighting this structure’s role in median nerve entrapment syndromes.
In fact, in the present cohort of 275 cases, only two patients were intra-operatively found to have a course of the median nerve that went between the ulnar and humeral heads of the pronator teres and, thus, could be defined as pronator syndromes in accordance with the original definition by Seyffarth [2]. Clinically, these two patients did not differ from the patients where the LF was the primary compressing structure. Additionally, one patient had concomitant compression at the superficialis arcade, and four revision procedures were done to release the median nerve at this level. For the superficialis arcade compression, the symptoms were that of pain approximately 3 cm distal of the LF as well as weakness in the flexor digitorum superficialis to the middle and ring fingers, a weakness not seen if the compression is at the LF alone. Although pronator involvement was exceedingly rare in our cohort, it is interesting to note that 222 patients (80.7%) reported having work that consisted of pronation for a minimum of five hours per day. It may thus be suggested that the vast majority of PMNE are not pronator syndrome but rather syndrome of pronation.
Pre-operative evaluation of the median nerve with ultrasound may be considered to distinguish between these rare but potentially differential diagnoses of PMNE sites. Ultrasound is a reliable imaging tool for diagnosing carpal tunnel syndrome [26] and is also proposed as a treatment modality for ultrasound-guided median nerve release both at the carpal tunnel and LF [17, 27, 28]. To date, however, there are no standardized protocols for median nerve ultrasound diagnostics proximal to the carpal tunnel. Future studies should aim to investigate normal and pathological median nerve ultrasound appearance from the distal upper arm (Struther’s arcade) to the mid-forearm (superficialis arcade) with regard to nerve size and structural integrity [29].
The present study certainly has some limitations. First, the short-term follow-up of patients, which is due to a fast recovery and symptomatic improvement after the surgical procedure, stops patients from complying with future appointments. Second is the lack of electromyographic assessment. However, as reported by other authors, electromyography has a limited role in diagnosing this clinical entity due to the dynamic nature of the median nerve entrapment [19,20,21, 30]. Lastly, the qualitative examination of the loss of strength was compensated with a comparative intraoperative strength assessment pre- and post-release. Future studies should focus on the prevalence of this syndrome and dynamic quantitative tests for its diagnostic workup.
Conclusion
Patients with isolated LS typically present with loss of hand strength and hand endurance/fatigue. Minimally invasive lacertus release immediately restores hand strength, significantly improves quick-DASH score and subscores, and yields positive outcomes regarding VAS pain, numbness, and subjective satisfaction with the surgery in patients with PMNE at a minimum six month follow-up.
Code/data availability
The data underlying this article are available in the article and its online supplementary material.
Abbreviations
- CTS:
-
carpal tunnel syndrome
- DASH:
-
Disability of the Arm Shoulder Hand Questionnaire
- FCR:
-
flexor carpi radialis
- FDP II:
-
flexor digitorum profundus to the index finger
- FPL:
-
flexor pollicis longus
- LF:
-
lacertus fibrosus
- LS:
-
lacertus syndrome
- PMNE:
-
proximal median nerve entrapment
- VAS:
-
visual analog scale
- WALANT:
-
wide-awake, local anesthesia, no tourniquet
References
Balcerzak AA, Ruzik K, Tubbs RS, Konschake M, Podgórski M, Borowski A, Drobniewski M, Olewnik Ł (2022) How to differentiate pronator syndrome from carpal tunnel syndrome: a comprehensive clinical comparison. Diagnostics 12(10):2433. https://doi.org/10.3390/diagnostics12102433
Seyffarth H (1951) Primary myoses in the M. pronator teres as cause of lesion of the N. medianus (the pronator syndrome). Acta Psychiatr Neurol Scand Suppl 74:251–254
Tubbs RS, Marshall T, Loukas M, Shoja MM, Cohen-Gadol AA (2010) The sublime bridge: anatomy and implications in median nerve entrapment. J Neurosurg 113(1):110–112. https://doi.org/10.3171/2009.10.JNS091251
Hagert E (2013) Clinical diagnosis and wide-awake surgical treatment of proximal median nerve entrapment at the elbow: a prospective study. Hand (N Y) 8(1):41–46. https://doi.org/10.1007/s11552-012-9483-4
Snoeck O, Lefèvre P, Sprio E, Beslay R, Feipel V, Rooze M, Van Sint Jan S (2014) The lacertus fibrosus of the biceps brachii muscle: an anatomical study. Surg Radiol Anat 36(7):713–719. https://doi.org/10.1007/s00276-013-1254-6
Caetano EB, Vieira LA, Almeida TA, Gonzales LAM, Bona JE, Simonatto TM, Bicipital aponeurosis. (2017) Anatomical study and clinical implications. Rev Bras Ortop 53(1):75–81. https://doi.org/10.1016/j.rboe.2017.11.014 PMID: 29367910; PMCID: PMC5771790
Löppönen P, Hulkkonen S, Ryhänen J (2022) Proximal median nerve compression in the differential diagnosis of carpal tunnel syndrome. J Clin Med 11(14):3988. https://doi.org/10.3390/jcm11143988
Sunderland S (1945) The intraneural topography of the radial, median and ulnar nerves. Brain 68:243–299. https://doi.org/10.1093/brain/68.4.243
Morris HH, Peters BH (1976) Pronator syndrome: clinical and electrophysiological features in seven cases. J Neurol Neurosurg Psychiatry 39(5):461–464. https://doi.org/10.1136/jnnp.39.5.461
Hsiao CW, Shih JT, Hung ST (2017) Concurrent carpal tunnel syndrome and pronator syndrome: a retrospective study of 21 cases. Orthop Traumatol Surg Res 103(1):101–103. https://doi.org/10.1016/j.otsr.2016.10.009
Özdemir A, Acar MA, Güleç A, Durgut F, Cebeci H (2020) Clinical, radiological, and electrodiagnostic diagnosis of pronator syndrome concurrent with carpal tunnel syndrome. J Hand Surg Am 45(12):1141–1147. https://doi.org/10.1016/j.jhsa.2020.06.006
Hagert E, Lalonde D (2015) Dags att begrava adrenalin-myten! - Säkert bruk av adrenalinbedövning inom handkirurgi och ortopedi [Time to bury the adrenaline-myth!--Safe use of adrenaline anesthesia in hand surgery and orthopedics]. Lakartidningen 112:C4MC
Hagert E, Lalonde DH, Ayhan E, Brutus JP, Ahmad AA, McKee D (2022) Lacertus syndrome: median nerve release at the elbow. In: Lalonde D (ed) Wide awake hand surgery, 2nd edn. Thieme Publishing, pp 141–144
Greenslade JR, Mehta RL, Belward P, Warwick DJ (2004) Dash and Boston questionnaire assessment of carpal tunnel syndrome outcome: what is the responsiveness of an outcome questionnaire? J Hand Surg Br 29(2):159–164. https://doi.org/10.1016/j.jhsb.2003.10.010
Gummesson C, Ward MM, Atroshi I (2006) The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 7:44. https://doi.org/10.1186/1471-2474-7-44
Binder H, Zadra A, Popp D, Komjati M, Tiefenboeck TM (2021) Outcome of surgical treated isolated pronator teres syndromes—a retrospective cohort study and complete review of the literature. Int J Environ Res Public Health 19(1):80. https://doi.org/10.3390/ijerph19010080
Apard T, Mares O, Duparc F, Michelin P (2022) Percutaneous ultrasound-guided release of the lacertus fibrosus for median nerve entrapment at the elbow. Cardiovasc Intervent Radiol 45(8):1198–1202. https://doi.org/10.1007/s00270-022-03123-0
El-Haj M, Ding W, Sharma K, Novak C, Mackinnon SE, Patterson JMM (2021) Median nerve compression in the forearm: a clinical diagnosis. Hand (N Y) 16(5):586–591. https://doi.org/10.1177/1558944719874137
Patterson JMM, Medina MA, Yang A, Mackinnon SE (2022) Posterior interosseous nerve compression in the forearm, AKA Radial Tunnel Syndrome: a clinical diagnosis. Hand (N Y), 15589447221122822. Advance online publication. https://doi.org/10.1177/15589447221122822
Peters BR, Pripotnev S, Chi D, Mackinnon SE (2022) Complete foot drop with normal electrodiagnostic studies: Sunderland “Zero” ischemic conduction block of the common peroneal nerve. Ann Plast Surg 88(4):425–428. https://doi.org/10.1097/SAP.0000000000003053
Carter GT, Weiss MD (2015) Diagnosis and treatment of work-related proximal median and radial nerve entrapment. Phys Med Rehabil Clin N Am 26(3):539–549. https://doi.org/10.1016/j.pmr.2015.04.001
Mujadzic M, Papanicolaou G, Young H, Tsai TM (2007) Simultaneous surgical release of ipsilateral pronator teres and carpal tunnel syndromes. Plast Reconstr Surg 119(7):2141–2147. https://doi.org/10.1097/01.prs.0000260703.56453.06
Lee AK, Khorsandi M, Nurbhai N, Dang J, Fitzmaurice M, Herron KA (2012) Endoscopically assisted decompression for pronator syndrome. J Hand Surg Am 37(6):1173–1179. https://doi.org/10.1016/j.jhsa.2012.02.023
Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G (2014) Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther 44(1):30–39. https://doi.org/10.2519/jospt.2014.4893
van Kampen DA, Willems WJ, van Beers LW, Castelein RM, Scholtes VA, Terwee CB (2013) Determination and comparison of the smallest detectable change (SDC) and the minimal important change (MIC) of four-shoulder patient-reported outcome measures (PROMs). J Orthop Surg Res 8:40. https://doi.org/10.1186/1749-799X-8-40
Fowler JR, Munsch M, Tosti R, Hagberg WC, Imbriglia JE (2014) Comparison of ultrasound and electrodiagnostic testing for diagnosis of carpal tunnel syndrome: study using a validated clinical tool as the reference standard. J Bone Joint Surg Am 96(17):e148. https://doi.org/10.2106/JBJS.M.01250
Leiby BM, Beckman JP, Joseph AE (2022) Long-term clinical results of carpal tunnel release using ultrasound guidance. Hand (N Y) 17(6):1074–1081. https://doi.org/10.1177/1558944720988080
Kamel SI, Freid B, Pomeranz C, Halpern EJ, Nazarian LN (2021) Minimally invasive ultrasound-guided carpal tunnel release improves long-term clinical outcomes in carpal tunnel syndrome. AJR Am J Roentgenol 217(2):460–468. https://doi.org/10.2214/AJR.20.24383
Telleman JA, Herraets IJ, Goedee HS, van Asseldonk JT, Visser LH (2021) Ultrasound scanning in the diagnosis of peripheral neuropathies. Pract Neurol 21(3):186–195. https://doi.org/10.1136/practneurol-2020-002645
Adler JA, Wolf JM (2020) Proximal median nerve compression: pronator syndrome. J Hand Surg Am 45(12):1157–1165. https://doi.org/10.1016/j.jhsa.2020.07.006
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by Elisabet Hagert and Theodorakys Marín Fermín. Data collection was performed by Ulrika Jedeskog. The first draft of the manuscript was written by Elisabet Hagert and Theodorakys Marín Fermín, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Swedish Ethical Review Authority (Dnr 2021-06048-01).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the videos in online resources 1 and 2.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Online Resource 1: Video of the clinical examination of the lacertus syndrome.
Online Resource 2: Video of the preoperative and intraoperative measurement of strength before and after lacertus release.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hagert, E., Jedeskog, U., Hagert, CG. et al. Lacertus syndrome: a ten year analysis of two hundred and seventy five minimally invasive surgical decompressions of median nerve entrapment at the elbow. International Orthopaedics (SICOT) 47, 1005–1011 (2023). https://doi.org/10.1007/s00264-023-05709-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05709-w