Abstract
Purpose
The COVID-19 pandemic is importantly affecting the orthopaedic practice all over the world with Northern Italy being the first European area that faced the worst scenario. In this study, the changes in clinical practice occurred in an orthopaedic center in Milan are described.
Methods
Number and type of admissions, outpatients cancelled and preserved, emergency room, and intensive care unit activities have been analyzed in the timeframe of seven weeks since the beginning of the pandemic (from February 24th to April 10th) and compared with the same period in 2019.
Results
The planned surgical admissions declined from 2172 in 2019 to 664 in 2020 (69.42%, p < 0.0001), while emergencies increased from 158 to 268 (69.62%). The rehabilitation admissions declined from 414 to 69 (83.33%). The overall admission decreased by 63.52%, the trend showed a drop in the last weeks. Surgery performed in the COVID-19 operating room increased by 16.7% in the last week. Seven deaths occurred (0.7% of all orthopaedics and trauma admissions) compared with four (0.1%) which happened in the same period in 2019 (p = 0.004). Six of these patients were suffering from COVID-19. A total of 23,580 outpatients (93.8%) were cancelled. Emergency room consultations declined by 68.14% and 63.47% among white and green priority, respectively, while increased by 25% and 100% among yellow and red, respectively.
Conclusion
These numbers show the radical changed scenario in an orthopaedic center in Milan during COVID-19 pandemic. Elective surgery declined rapidly going close to zero, outpatient admissions were restricted to cases that cannot be postponed, while emergencies increased due to the role played by the hospital as referral orthopaedic centre during the pandemic. The still ongoing emergency will have important impacts on the overall orthopaedic healthcare management for the next months.
Similar content being viewed by others
Introduction
The profound healthcare reorganization caused by the coronavirus disease 2019 (COVID-19) pandemic has resulted in a significant reallocation of health resources with the focus on COVID-19 patients all over the world [1].
Northern Italy was the first European area that faced the worst infection scenario. Lombardy is the largest Italian region with a recorded population of 10,060,000 people at the beginning of 2020 [2]. It is the major economic and industrial area of the country. The Regional Health System is recognized as one of the best performing in Italy including orthopaedic procedures. A total of 23.4% of all the total joint replacements and 24.0% of all revisions in Italy are performed in the Lombardy Region according to the Italian Arthroplasty Registry (RIAP) [3].
Lombardy has been suffering the most critical novel SARS-CoV2 situation in Italy with a rapid and acute spread of the pandemic during February and March 2020. At the time of data retrieved (April 15th), the total number of COVID-19-positive cases in the region was 62,153, of which 12,043 patients were hospitalized and 1074 more in intensive care units (ICUs) and 11,377 people were dead (57% of overall Italian deceased) [4].
The rapid pandemic spread has dramatically affected the orthopaedic practice. Hospitals and departments have been quickly converted to COVID-19 care centres since the beginning of the emergency. Staff and operating rooms (ORs) have been converted, elective surgical procedures have been either cancelled or postponed, and nonurgent consultations have been stopped. Most general hospitals have been overwhelmed with SARS-CoV2 patients while, according to the regional reorganization, non-deferrable orthopaedics and trauma cases are being referred to selected centers, designated as either minor or major trauma hubs.
IRCCS Istituto Ortopedico Galeazzi is located in Milan, the capital of Lombardy. It is one of the major orthopaedic centres in Italy with high volume of surgery (4006 total joints procedures and 1759 spine procedure in 2019). It provides emergency service for minor orthopaedic trauma, it is accredited to the Italian Ministry of Health as clinical and basic research center and provides academic and training activity. To cope with the emergency period, the hospital has been designated by the regional government as a referral centre for minor trauma and orthopaedics and has even contributed to COVID-19 patient care in ICU and in a converted department.
The purpose of this study is to describe the profound changes in the clinical practice and the consequent effects on the clinical management of orthopaedic patients that have occurred in a specialized orthopaedic centre during the first seven weeks (from February 24th to April 10th 2020) of COVID-19 emergency in Milan.
Materials and methods
Internal administrative flows integrated and double-checked by the health management data of the hospital represented the data sources of the present study. Approval was obtained by the institutional review board, in using anonymous data flows.
Reorganization of the hospital in a network area
The trigger of a consecutive series of changes in Italy was the identification of the first Italian citizen affected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) in Lombardy. He was a young man from Codogno, a small town in the southern Lombardy on February the 21st. The day after National Government’s restrictions fixed some areas of Lombardy as red zones and closed schools for COVID-19. At this point, Galeazzi Institute started to reduce the operating rooms and the number of elective operations since February 24th (Week 1). The following week, some more surgeries were allowed; in the meantime, the patients with less severe pain conditions started to decline spontaneously their attendance both for surgical procedures and for consultations (Week 2). On March 8th, the number of operating rooms (ORs) was reduced to 60% (Week 3) in parallel to regional and national lockdown, approved on the same day, and following the regional resolution delivered that established roles and duties of regional hospitals in order to face the spreading of the pandemic. Moreover, during this week, a dedicated COVID-19 OR was quickly set up. On March 14th, the orthopaedic network was rebuilt by an addendum to the regional resolution. Galeazzi Institute was identified as a hub for nondeferrable orthopaedic procedures (Table 1) and for minor orthopaedic trauma, while most of general hospitals and ICUs in the region were increasingly overloaded with COVID-19 patients. Since March 16th (Week 4), nearly all the surgery but acute trauma, acute infections, and malignant tumours resections were stopped in our institution. Also, cases to be, theoretically, performed according to regional rules (i.e. severe loosening or recurrent dislocations or rapid developing arthritis with bone necrosis) have been stopped as the widespread dissemination of COVID19 infections increased the risk of nosocomial infection. Since Week 4, only two or three ORs were running depending on the number of emergencies. Hence, during Weeks 5, 6, and 7, only trauma, acute orthopedic infections, and malignant tumours resections were performed both on COVID-19 positive and negative patients.
Reorganization of the institute went on consequently. Starting from Week 3, departments were isolated for COVID-19 patients, with healthcare personnel provided with high-level personal protection equipment (PPE), impossibility for relatives to meet patients, according to infection disease protection protocols. During Week 4, in order to face the huge increase in the number of infected patients all around the region, even non-orthopedic COVID-19 patients were admitted to the hospital and were allocated in a separate department. Starting from Week 5, even the relatives of SARS-CoV2-negative patients were no longer allowed to access the hospital in order to further reduce the risk of infection. Since Week 5, all the hospitalized patients have been screened for COVID-19 infection with nasopharyngeal swab and allocated at time of admission in an observational area until the result of the test (usually taking 1 day) and then transferred to the COVID-19 department or to the non-COVID ones who were located on separate floors. Due to these restrictions and to the reduced nurse staff (in the meantime, the number of personnel in quarantine raised), the number of beds was reduced to less than a third (median 100; 364 beds including rehabilitation are usually occupied).
A special effort involved the anaesthetists of the institution. Usually the ICU is dedicated to post-operative monitoring and intensive care of the most complicated patients and those undergoing most complex surgical procedures. Six out of eight beds are usually occupied, every day, for this activity. Starting from Week 3, four beds were turned in an isolated area for severe intubated COVID-19 patients coming from other hospitals. During the most critical time in Week 4, as part of the Regional Network of ICUs, the ICU was extended and moved into a floor usually fully occupied by an operating block that was adapted for respiratory assistance of ten intubated patients.
Number and type of admissions in the hospital are reported in a seven week period since the beginning of the pandemic phase (from February 24th to April 10th) and compared with the same period in 2019. The analysis includes type of surgeries and number of deaths in COVID-19 and non-COVID-19 orthopedic patients, number of outpatients canceled and preserved, and frequency of patients in emergency room.
Statistical analysis
The differences among the data observed over the seven weeks in 2020 and the corresponding period in 2019 were analyzed by means of the Mann-Whitney U test. Data recorded in the first three weeks and in the last four weeks of the seven week period in 2019 and 2020 have been compared using ordinary two-way ANOVA with Sidak’s multiple comparison test. Data have been analyzed by the means of χ2 test in order to compare the corresponding weeks in 2019 and 2020: admission rates in terms of surgery cases and rehabilitation cases, planned vs urgent surgery, and number of deaths. Statistical analysis has been performed with GraphPad Prism v6.0 (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Number and type of surgery and admissions
The overall number of admissions declined from 2744 in 2019 to 1001 in 2020 (63.52%, Tables 2, 3, and 4) in the whole period, but the trend shows a major drop of the curve on Week 4 (Fig. 1a). The mean value of total admissions in the seven observed weeks was decreased in 2020 compared with 2019 (p = 0.0006), as shown in Fig. 1b. The decrease continued up to 88% during Week 7 with only 47 admissions (4 oncologic cases, 41 trauma patients, and 3 others included 1 tendon rupture and 2 infections) (Table 3). The mean value of admissions in the first three weeks and the last four weeks in 2020 were both significantly decreased compared with 2019 (p = 0.0013, p < 0.0001). Moreover, considering the mean number of admissions in the first three weeks and the last four weeks (Fig. 1c), the two values were comparable (p = 0.96) in 2019, while they significantly differed in 2020 (p = 0.0001). In addition, the rehabilitation admissions declined from 414 to 69 (83.33%) (Table 2). The rehabilitation department was closed at the end of Week 4 due to the decreased number of patients and also to limit at the maximum the risk of nosocomial infection spreading while the hospital was reorganized to host non-orthopedic COVID-19 patients, on a separate floor. The planned surgical admissions declined from 2172 in 2019 to 664 in 2020 (69.42%), whereas emergencies increased from 158 (6.8% of admissions) to 268 (28.8% of admissions) in 2020 (69.62%), including network admissions and transfers from other hospitals (Table 4). Operations performed in the COVID-19 OR were 31 (3.5% in the whole period), raising up to 16.67% (6 cases vs 36 in standard ORs) in the Week 7 (Table 5). Basically, the activity has been converted from mainly elective surgery to emergencies.
Outpatient activity
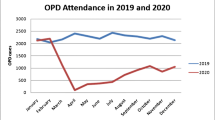
A total number of 23,580 (93.8%) outpatients were canceled declining to 365 in the Week 7 (Table 6), and the mean value of outpatients in all period of 7 weeks in 2020 significantly decreased compared with 2019 (p = 0.03) (Fig. 2a). Starting from Week 2, a spontaneous reduction of the number of outpatients due to the regional lockdown and to the increasing concerns of the population on the pandemic was observed. During Week 4, consultations were cancelled directly by the booking office of the hospital and then limited to nondeferrable cases (sutures, plaster cast removals, immediate post-operative controls, emerging complications) based on an agreement between the call centre and the surgeons. This situation has continued along the time (Weeks 5, 6, and 7). Indeed, in 2020, the mean value of outpatient in the last four weeks decreased in comparison with 2019 (p < 0.0001). Moreover, in 2020, the mean value of outpatients in the last four weeks significantly decreased compared with the outpatients in the first three weeks (p < 0.0001), as shown in Fig. 2b.
The flow of patients in emergency room
The flow of patients in the emergency room (ER) spontaneously reduced, mainly in the less severe cases. All the patients were admitted to triage procedures as usual, the only differences were a strict protocol regarding PPE of the staff and the number of patients admitted in the waiting room. Moreover, no relatives were allowed and protection devices were provided to the patients. According to triage classification when compared with 2019 (Table 7), there was a reduction of 68.14% and 63.47% in white and green codes, while yellow codes increased by 25% and red codes went up from 0 in 2019 to 7 patients in 2020 (Fig. 3). ERs in orthopedic centers are not usually intended as a life-threatening first aid.
The impact of pandemic on hospital contamination and mortality
A total number of 79 COVID-19 patients were treated; 25 (31.64%) of them were orthopaedics or trauma cases that developed SARS-CoV2-like symptoms during hospitalization (3% of all admissions) in the surgical or in the rehabilitation department. They were preventively isolated in an observational area and, after the test, recognized as COVID-19-positive and sent in the COVID-19 department. Sixteen more were orthopaedics and trauma patients recognized as positive since the admission. The remaining 38 were not orthopaedics or trauma patients: two were admitted directly by the ER for respiratory symptoms and 36 were transferred from other hospitals in the COVID-19 department or in the ICU that was converted to host positive patients, as previously described. The ICU for COVID-19 had 15 admissions in total, with four deaths and four discharges.
Eleven patients died in the study period at our hospital. Seven deaths occurred (0.7% of all admissions) among orthopaedics and trauma patients, compared with four (0.1%) in the same period of 2019 (p = 0.004) (Table 8), with six of these patients suffering from COVID-19 (Table 9). The seven cases included four patients with femoral neck fractures (three COVID-19 patients) aged 77, 87, 88, and 95 years old, respectively, all females, one oncologic patient with bone metastasis (74 years old, male), and two women who underwent total knee arthroplasty (79 and 84 years old, respectively) who gave a positive swab test during the rehabilitation time and developed pulmonary complications related to COVID-19 infection. Four deaths occurred in COVID-19 positive patients with no orthopaedic-related problems, coming from other hospitals.
Discussion
The aim of this study was to describe the profound modifications of the SARS-CoV2 pandemic. To the best of our knowledge, this is the first report about the change in orthopaedic practice in a specialized orthopaedic centre during the spread of COVID-19 pandemic over seven weeks of activity and the role of such institution in a pandemic scenario that included some non-orthopaedic clinical activities.
Asian orthopaedic surgeons, based on the lessons learned from SARS-CoV2 in 2003, postponed or cancelled all elective surgery requiring more than 23 hours of hospitalization [5]. In other medical disciplines, downturn in the activities have already been reported during the COVID-19 pandemic, such as a reduction in major organ transplantation (more than 25%) [6], a significant reduction in colorectal surgery [7], along with concerns about urology patients [8], especially in those with malignant tumours.
All the planned surgical procedures have been progressively stopped in our institution during the crisis [9]. At the beginning, this strategy was applied only to elective procedures, limiting indications to rapidly progressive arthritis with bone necrosis, severe implant loosening, and failure of previous fixation according to the regional resolution. Then, in the time of the maximum spreading of COVID-19 infection, all the operations were postponed except for trauma, acute infection, and malignant tumours resections. This type of approach taken out by both health authorities and orthopaedic surgeons has several undoubtable reasons: to preserve resources for COVID-19 patients (staff, hospital beds, ICU, economy), to reduce the risks of contamination (of the staff, of the patients, of the whole community) in an “open environment” such as the hospital that is difficult to be controlled, and to guarantee a safe and effective rehabilitation time for the patients operated upon. The possible contamination rate in all the admissions was 3%, extremely low; nevertheless, old fragile patients are at major risk. For this reason, it looks reasonable to stop all the surgery “that can be postponed.” A case by case discussion with the patients and the relatives about pros and cons of delaying surgery has been done in the most critical cases, sharing the decisions with the patients. An overall increase of mortality in trauma and orthopaedics patients was observed compared with the same period in 2019 that was clearly related to COVID-19.
Not only the admissions have been postponed but also consultations and outpatients have been deferred in the vast majority. At the time of writing, no one could know the real impact of the pandemic on the waiting lists, which is supposed to be huge along with the chances of providing timely and safe treatments to our elective surgical cases. The decision on the consultations that cannot be postponed was taken by clinicians in collaboration with the booking office.
The emergency flow was influenced by the regional resolution that assigned the role of hub for minor trauma to the institute. This decision and the consequent actions taken to reorganize the hospital (creation of complete selected COVID-19 journey including separated OR, reinforcement of emergency staff) show how much is important, in the time of such a pandemic, a global strategy and a well-functioning local network able to provide the best and safest healthcare to the patients. The attendance in the ER spontaneously decreased in the lighter cases.
Orthopaedic surgeons changed their practice according to their best skills. Even some arthroplasty surgeons had taken care of trauma cases and part of the staff supported also the care of COVID-19 patients under the supervision of anaesthetists and clinicians. In emergency, 45 non-orthopaedic patients were treated including ICU assistance. The relation with relatives changed as they were not admitted to the hospital. For this reason, a daily phone call, in order to provide information about patients, was scheduled.
This study has several limitations. First of all, its retrospective nature, but it would not have been possible the contrary considering that the emergency was clearly unexpected until some weeks ago. Moreover, our hospital is a specialized orthopaedic centre. For this reason, its role in the whole COVID-19 pandemic scenario was limited compared with large general hospitals in the region where orthopaedics and even trauma activity was completely stopped. Nevertheless, the focus of the paper was to describe the huge changes in the orthopaedic practice during the pandemic. Another limitation is that, according to continuously changing protocols, the patients were screened for COVID-19 only after Week 4, so it may be possible that the number of SARS-CoV2 has been underestimated. Finally, we did not have results of any test at time of discharge for the negative patients and neither information after the hospitalization about changes in their clinical conditions. However, all the patients were in good clinical conditions at the time of discharge, including respiratory function.
In conclusion, the experience in an orthopaedic centre located in the middle of one of the most critical areas worldwide during the COVID-19 pandemic demonstrated how orthopaedic activities could be seriously affected. The experience showed the need for flexibility by healthcare professionals in their tasks in emergency time, the importance of clear and timely protocols, and of coordination at institutional, regional, and national level. When the present emergency will be hopefully over, new challenges are waiting the orthopaedic community with longer waiting lists, the risk of recurrence of the COVID-19 infection, and probably limited healthcare resources. We hope that the efforts experienced by the orthopaedic staff of our institute could be of help for other colleagues facing a similar challenging pandemic in their countries.
References
Tsai J, Wilson M (2020) COVID-19: a potential public health problem for homeless populations. Lancet Public Health 5:e186–e187. https://doi.org/10.1016/S2468-2667(20)30053-0
Popolazione residente al 1° gennaio. http://dati.istat.it/Index.aspx?QueryId=18460. Accessed 15 Apr 2020
(2017) Quarto Report RIAP 2017. In: RIAP. http://riap.iss.it/riap/it/attivita/report/2017/12/15/quarto-report-2017/. Accessed 14 Apr 2020
Salute M della Covid-19, i casi in Italia 13 aprile ore 18. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4459. Accessed 14 Apr 2020
Chang Liang Z, Wang W, Murphy D, Po Hui JH (2020) Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.20.00236
Angelico R, Trapani S, Manzia TM et al (2020) The COVID-19 outbreak in Italy: initial implications for organ transplantation programs. Am J Transplant. https://doi.org/10.1111/ajt.15904
Lisi G, Campanelli M, Spoletini D, Carlini M (2020) The possible impact of COVID-19 on colorectal surgery in Italy. Color Dis. https://doi.org/10.1111/codi.15054
Connor MJ, Winkler M, Miah S (2020) COVID-19 pandemic - is virtual urology clinic the answer to keeping the cancer pathway moving? BJU Int. https://doi.org/10.1111/bju.15061
D’Apolito R, Faraldi M, Ottaiano I, Zagra L (2020) Disruption of arthroplasty practice in an orthopedic center in Northern Italy during the coronavirus disease 2019 pandemic. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.04.057
Availability of data and material
Not applicable
Code availability
Not applicable
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript, and they all approved the final version.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
A statement is reported in the manuscript with regard to Institutional Review Board Approval.
Consent to participate
Not applicable
Consent for publication
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zagra, L., Faraldi, M., Pregliasco, F. et al. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. International Orthopaedics (SICOT) 44, 1591–1598 (2020). https://doi.org/10.1007/s00264-020-04590-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04590-1