Abstract
Purpose
Prevention of thromboembolic disease requires patients’ adherence to the extended thromboprophylaxis scheme. Oral anticoagulants are expected to improve adherence as a result of their route of administration; however, this assumption is yet to be confirmed. The purpose of this study was to assess the impact of the route of administration and dosage regimen on the compliance to the prescription.
Materials and methods
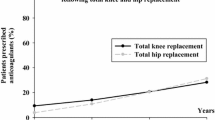
This prospective cohort study included hip and knee arthroplasty patients who received pharmacological extended thromboprophylaxis with one daily injection, one daily oral tablet, or two daily oral tablets. A telephonic questionnaire was applied 35 days after the day of the surgery. Patients who omitted one or more doses of medication during the follow-up period were classified as “non-adherent.” Differences of adherence rates were assessed.
Results
Five hundred and twenty patients were included: 153 received Apixaban (oral, twice a day), 155 Enoxaparin (injectable, once a day), and 212 Rivaroxaban (oral, once a day). Patients receiving oral once a day medication was more compliant compared with those who received an oral medication twice a day. Non-adherence rates were 3.2 and 9.2%, respectively (p = 0.033). No significant differences (p = 0.360) were found between oral once a day and injectable once a day medication.
Conclusions
The number of daily doses prescribed was related to adherence to extended chemical prophylaxis, while the route of administration did not seem to have a significant impact. Strategies to promote outpatient compliance must be implemented, especially when regimes including more than one daily dose are prescribed.





Similar content being viewed by others
References
Arcelus JI, Felicissimo P (2013) Venous thromboprophylaxis duration and adherence to international guidelines in patients undergoing major orthopaedic surgery: results of the international, longitudinal, observational DEIMOS registry. Thromb Res 131:e240–e246. https://doi.org/10.1016/j.thromres.2013.03.014
Bala A, Huddleston JI, Goodman SB et al (2017) Venous thromboembolism prophylaxis after TKA: aspirin, warfarin, enoxaparin, or factor Xa inhibitors? Clin Orthop Relat Res 475:2205–2213. https://doi.org/10.1007/s11999-017-5394-6
Bautista M, Llinás A, Bonilla G et al (2016) Thromboprophylaxis after major orthopedic surgery: improving compliance with clinical practice guidelines. Thromb Res 137:113–118. https://doi.org/10.1016/j.thromres.2015.10.020
Bergqvist D, Arcelus J, Felicissimo P (2012) Post-discharge compliance to venous thromboembolism prophylaxis in high-risk orthopaedic surgery- results from the ETHOS registry. Thromb Haemost 107:280–287
Borris L (2010) Emerging antithrombotic agents for thromboprophylaxis, clinical potential and patient considerations. J Blood Med 123. https://doi.org/10.2147/JBM.S6543
Carrothers AD, Rodriguez-Elizalde SR, Rogers BA et al (2014) Patient-reported compliance with thromboprophylaxis using an oral factor Xa inhibitor (rivaroxaban) following total hip and total knee arthroplasty. J Arthroplast 29:1463–1467. https://doi.org/10.1016/j.arth.2013.02.001
Claxton AJ, Cramer J, Pierce C (2001) A systematic review of the associations between dose regimens and medication compliance. Clin Ther 23:1296–1310. https://doi.org/10.1016/S0149-2918(01)80109-0
Falck-Ytter Y, Francis C, Johanson N et al (2012) Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e278S–e325S. https://doi.org/10.1378/chest.11-2404
Farfan M, Bautista M, Bonilla G et al (2016) Worldwide adherence to ACCP guidelines for thromboprophylaxis after major orthopedic surgery: a systematic review of the literature and meta-analysis. Thromb Res 141:163–170. https://doi.org/10.1016/j.thromres.2016.03.029
Hull RD, Pineo GF, Stein PD et al (2001) Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 135:858–869. https://doi.org/10.7326/0003-4819-135-10-200111200-00006
Januel J, Chen G, Ruffieux C (2012) Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee Arthroplasty among patients receiving recommended prophylaxis. A systematic review. J Am Med Assoc 307:294–303
Lebel B, Malherbe M, Gouzy S et al (2012) Oral thromboprophylaxis following total hip replacement: the issue of compliance. Orthop Traumatol Surg Res 98:186–192. https://doi.org/10.1016/j.otsr.2011.10.010
Merli GJ, Malangone E, Lin J et al (2011) Real-world practices to prevent venous thromboembolism with pharmacological prophylaxis in US orthopedic surgery patients: an analysis of an integrated healthcare database. J Thromb Thrombolysis 32:89–95. https://doi.org/10.1007/s11239-011-0554-0
Muntz JE, O’ Connor PJ, Yin H, Vogenberg FR (2007) Factors associated with thromboprophylaxis for orthopedic patients and their impact on outcome. Am J Orthop 36:193–197
NHS. National Institute for Health and Clinical Excellence (2010) Venous thromboembolism: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary emboism) in patients admitted to hospital
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353:487–497. https://doi.org/10.1056/NEJMra050100
Peidro-Garces L, Otero-Fernandez R, Lozano-Lizarraga L (2013) Adherence to and satisfaction with oral outpatient thromboembolism prophylaxis compared to parenteral: SALTO study. Rev Esp Cir Ortop Traumatol 57:53–60. https://doi.org/10.1016/j.recot.2012.10.009
Rodríguez Chamorro MÁ, García-Jiménez E, Amariles P et al (2008) Revisión de tests de medición del cumplimiento terapéutico utilizados en la práctica clínica. Aten Primaria 40:413–417. https://doi.org/10.1157/13125407
Selby R, Borah BJ, McDonald HP et al (2012) Impact of thromboprophylaxis guidelines on clinical outcomes following total hip and total knee replacement. Thromb Res 130:166–172. https://doi.org/10.1016/j.thromres.2012.01.013
Warwick D, Friedman RJ, Agnelli G et al (2007) Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the global orthopaedic registry. J Bone Joint Surg (Br) 89:799–807. https://doi.org/10.1302/0301-620X.89B6.18844
Wilke T (2009) Patient preferences for an oral anticoagulant after major orthopedic surgery. Patient 2:39–49. https://doi.org/10.2165/01312067-200902010-00005
Wilke T, Moock J, Müller S et al (2010) Nonadherence in outpatient thrombosis prophylaxis with low molecular weight heparins after major orthopaedic surgery. Clin Orthop Relat Res 468:2437–2453. https://doi.org/10.1007/s11999-010-1306-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JM declares that he has no conflict of interest. MB has received royalties for research support from a company or supplier as a principal researcher from Grunenthal and DePuy Synthes (Orthopedics), and other financial support from Grunenthal and Abbott. JC declares that he has no conflict of interest. GB has participated as paid speaker for Boehringer-Ingelheim, Pfizer, Sanofi, and DePuy Synthes (Orthopedics); has received other financial support from DePuy Synthes (Orthopedics); and has received research support from a company or supplier as a principal researcher for Grunenthal and DePuy Synthes (Orthopedics), outside this work. AL has received royalties from Innomed, Novamed, and 3 M; has participated as paid speaker for Zimmer, Shire, Novonordisk, Novartis, DePuy Synthes (Orthopedics), Medtronic Bayer, and Procaps; has participated as paid consultant for Zimmer and Medtronic, outside this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moreno, J.P., Bautista, M., Castro, J. et al. Extended thromboprophylaxis for hip or knee arthroplasty. Does the administration route and dosage regimen affect adherence? A cohort study. International Orthopaedics (SICOT) 44, 237–243 (2020). https://doi.org/10.1007/s00264-019-04454-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04454-3