Abstract
Purpose
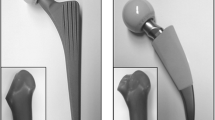
After clinical introduction of the Fitmore® stem (Zimmer), we noticed the formation of cortical hypertrophies in a few cases. We questioned whether (1) the primary stability or (2) load transfer of the Fitmore® stem differs from other stems unassociated with the formation of hypertrophies. We compared the Fitmore® stem to the well-established CLS® stem.
Methods
Four Fitmore® and four CLS® stems were implanted in eight synthetic femurs. A cyclic torque around the stem axis and a mediolateral cyclic torque were applied. Micromotions between stems and femurs were measured to classify the specific rotational implant stability and to analyse the bending behaviour of the stem.
Results
No statistical differences were found between the two stem designs with respect to their rotational stability (p = 0.82). For both stems, a proximal fixation was found. However, for the mediolateral bending behavior, we observed a significantly (p < 0.01) higher flexibility of the CLS® stem compared to the Fitmore® stem.
Conclusion
Hip stem implantation may induce remodelling of the periprosthetic bone structure. Considering the proximal fixation of both stems, rotational stability of the Fitmore® stem might not be a plausible explanation for clinically observed formation of hypertrophies. However, bending results support our hypothesis that the CLS® stem presumably closely follows the bending of the bone, whereas the shorter Fitmore® stem acts more rigidly. Stem rigidity and flexibility needs to be considered, as they may influence the load transfer at the implant–bone interface and thus possibly affect bone remodelling processes.




Similar content being viewed by others
References
Garellick G (2012) Swedish Hip Arthroplasty Register. Annual Report 2011. Department of Ortopaedics, Sahlgrenska University Hospital
Rubash HE, Sinha RK, Shanbhag AS, Kim SY (1998) Pathogenesis of bone loss after total hip arthroplasty. Orthop Clin North Am 29(2):173–186
Scannell PT, Prendergast PJ (2009) Cortical and interfacial bone changes around a non- cemented hip implant: simulations using a combined strain/damage remodelling algorithm. Med Eng Phys 31(4):477–488. doi:10.1016/j.medengphy.2008.11.007
Bobyn JD, Mortimer ES, Glassman AH, Engh CA, Miller JE, Brooks CE (1992) Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res 274:79–96
Van Rietbergen B, Huiskes R, Weinans H, Sumner DR, Turner TM, Galante JO (1992) ESB Research Award 1992. The mechanism of bone remodeling and resorption around press- fitted THA stems. J Biomech 26(4–5):369–382
Sumner DR, Galante JO (1992) Determinants of stress shielding: design versus materials versus interface. Clin Orthop Relat Res 274:202–212
Bougherara H, Bureau MN, Yahia L (2010) Bone remodeling in a new biomimetic polymer-composite hip stem. J Biomed Mater Res A 92(1):164–174. doi:10.1002/jbm.a.32346
Glassman AH, Bobyn JD, Tanzer M (2006) New femoral designs: do they influence stress shielding? Clin Orthop Relat Res 453:64–74
Morrey BF, Adams RA, Kessler M (2000) A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br 82(7):952–958
Wilkinson JM, Hamer AJ, Rogers A, Stockley I, Eastell R (2003) Bone mineral density and biochemical markers of bone turnover in aseptic loosening after total hip arthroplasty. J Orthop Res 21(4):691–696. doi:10.1016/S0736-0266(02)00237-1
Steinhauser E (2006) Biomechanical principles of implant anchoring. In: Gradinger R, Gollwitzer H (eds) Ossear integration. Springer Medizin Verlag, Heidelberg, pp 16–23
Bensmann G (1990) [Cementless fixation of endoprostheses]. Biomed Tech (Berl) 35(Suppl 3):44–47
Gustke K (2012) Short stems for total hip arthroplasty: initial experience with the Fitmore stem. J Bone Joint Surg Br 94(11 Suppl A):47–51. doi:10.1302/0301-620X.94B11.30677
Streit MR, Schroder K, Korber M, Merle C, Gotterbarm T, Ewerbeck V, Aldinger PR (2012) High survival in young patients using a second generation uncemented total hip replacement. Int Orthop 36(6):1129–1136. doi:10.1007/s00264-011-1399-z
Schmidbauer U, Brendel T, Kunze KG, Nietert M, Ecke H (1993) Dynamic force measurement in implantation of total endoprostheses of the hip joint. Unfallchirurgie 19(1):11–15
Gortz W, Nagerl UV, Nagerl H, Thomsen M (2002) Spatial micromovements of uncemented femoral components after torsional loads. J Biomech Eng 124(6):706–713
Jakubowitz E, Bitsch RG, Heisel C, Lee C, Kretzer JP, Thomsen MN (2008) Primary rotational stability of cylindrical and conical revision hip stems as a function of femoral bone defects: an in vitro comparison. J Biomech 41(14):3078–3084. doi:10.1016/j.jbiomech.2008.06.002
Jakubowitz E, Kinkel S, Nadorf J, Heisel C, Kretzer JP, Thomsen MN (2011) The effect of multifilaments and monofilaments on cementless femoral revision hip components: an experimental study. Clin Biomech (Bristol, Avon) 26(3):257–261. doi:10.1016/j.clinbiomech.2010.11.004
Wolff J (1892) Law of bone remodeling. Law of bone remodeling. Julius Wolf Institut, Charité - Universitätsmedizin Berlin, Hirschwald
Jasty M, O’Connor DO, Henshaw RM, Harrigan TP, Harris WH (1994) Fit of the uncemented femoral component and the use of cement influence the strain transfer the femoral cortex. J Orthop Res 12(5):648–656. doi:10.1002/jor.1100120507
Brodner W, Bitzan P, Lomoschitz F, Krepler P, Jankovsky R, Lehr S, Kainberger F, Gottsauner-Wolf F (2004) Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty. A five-year longitudinal study. J Bone Joint Surg Br 86(1):20–26
Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D (2009) Survival of the cementless Spotorno stem in the second decade. Clin Orthop Relat Res 467(9):2297–2304. doi:10.1007/s11999-009-0906-7
Merle C, Streit MR, Volz C, Pritsch M, Gotterbarm T, Aldinger PR (2011) Bone remodeling around stable uncemented titanium stems during the second decade after total hip arthroplasty: a DXA study at 12 and 17 years. Osteoporos Int 22(11):2879–2886. doi:10.1007/s00198-010-1483-z
Bieger R, Ignatius A, Decking R, Claes L, Reichel H, Durselen L (2012) Primary stability and strain distribution of cementless hip stems as a function of implant design. Clin Biomech (Bristol, Avon) 27(2):158–164. doi:10.1016/j.clinbiomech.2011.08.004
Huiskes R, Weinans H, van Rietbergen B (1992) The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop Relat Res 274:124–134
Saito J, Aslam N, Tokunaga K, Schemitsch EH, Waddell JP (2006) Bone remodeling is different in metaphyseal and diaphyseal-fit uncemented hip stems. Clin Orthop Relat Res 451:128–133. doi:10.1097/01.blo.0000224045.63754.a3
Mulier M, Jaecques SV, Raaijmaakers M, Nijs J, Van der Perre G, Jonkers I (2011) Early periprosthetic bone remodelling around cemented and uncemented custom-made femoral components and their uncemented acetabular cups. Arch Orthop Trauma Surg 131(7):941–948. doi:10.1007/s00402-010-1239-4
Yamaguchi K, Masuhara K, Ohzono K, Sugano N, Nishii T, Ochi T (2000) Evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. The influence of the extent of porous coating. J Bone Joint Surg Am 82-A(10):1426–1431
Falez F, Casella F, Panegrossi G, Favetti F, Barresi C (2008) Perspectives on metaphyseal conservative stems. J Orthop Traumatol 9(1):49–54. doi:10.1007/s10195-008-0105-4
Chen HH, Morrey BF, An KN, Luo ZP (2009) Bone remodeling characteristics of a short- stemmed total hip replacement. J Arthroplasty 24(6):945–950. doi:10.1016/j.arth.2008.07.014
Santori FS, Santori N (2010) Mid-term results of a custom-made short proximal loading femoral component. J Bone Joint Surg Br 92(9):1231–1237. doi:10.1302/0301-620X.92B9.24605
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
W. Pepke and J. Nadorf shared first-authorship: these authors contributed equally to the study.
Rights and permissions
About this article
Cite this article
Pepke, W., Nadorf, J., Ewerbeck, V. et al. Primary stability of the Fitmore® stem: biomechanical comparison. International Orthopaedics (SICOT) 38, 483–488 (2014). https://doi.org/10.1007/s00264-013-2138-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2138-4