Abstract
Purpose
Bisphosphonates (BPs) are antiresorptive drugs typically used to inhibit bone resorption. The latest reports show that BPs play an important role in not only achieving better bone mineral density but also in improving bone microarchitecture. The mechanism of action of the BPs is complex and multifactorial. We tried to determine whether there are any changes in the microarchitectural bone structure during local use of BP (Pamifos 60). The aim of this study was to see if BP-enriched cement used in rat models had positive effects on bone formation.
Methods
Research was performed on 40 adult male Wistar rats that were divided into four groups: two control groups and two experimental groups. Rats in the experimental groups were implanted with BP-enriched cement into the bone, while the control group rats were implanted with clean bone cement (without BP). Micro-computed tomography was applied for the investigation of trabecular microarchitecture of the proximal physis of the tibial bone in all animals three and six weeks after surgery. In all microCT images variables such as bone volume density (BV/TV), trabecular thickness (TbTh), trabecular separation (TbSp) and trabecular number (TbN) were used to describe trabecular bone morphometry.
Results
The major finding of this study is that using BP-enriched cement results in distinct changes in bone microarchitecture. We showed that local use of pamidronate (Pamifos 60) in orthopaedic cement had a positive effect on bone formation. It significantly changed three variables. We noticed increasing bone volume fraction and trabecular thickness together with decreasing trabecular separation.
Conclusion
In this paper we demonstrate the efficacy of using BP-enriched cement in vitro in the tibiae of rats. Our most significant finding based on micro-CT picture analysis allows us to start further work on more suitable applications of BP-enriched cement in humans. We believe that future successful experiments will facilitate potential use of BP-enriched cement in clinical applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates (BPs) are antiresorptive drugs typically used to inhibit bone resorption. The latest reports show that BPs play an important role not only in achieving better bone mineral density but also in improving bone microarchitecture [1, 2].
The mechanism of action of the BPs is complex and multifactorial [3–5]. However BPs have an affinity for bone mineral and they act specifically on bone. During resorption of bone by osteoclasts, the ingestion of BPs interferes with specific intracellular processes, which impair osteoclast function and ultimately cause apoptosis or cell death. BPs also regulate osteoblastic functions such as proliferation and differentiation, prevent osteoblast apoptosis, modulate osteoblastic production of extracellular matrix proteins, and regulate osteoblastic expression and secretion of various growth factors and cytokines [6, 7]. Several recent studies, both preclinical and clinical, have focused on the potential application of the BPs to the problems of bone catabolism encountered in orthopaedics [8]. BP therapy is effective in reducing bone turnover by decreasing bone resorption rather than bone formation. BPs are widely used in the treatment of many skeletal disorders such as osteoporosis, malignant hypercalcaemia, bone metastasis or Paget’s disease [9–11]. Some studies have shown that nanomolar concentration of BPs had a positive effect on osteoblast and osteocytes [12, 13]. It is reasonable to believe that all those factors increase the bone density and may have a positive influence on bone implant osteointegration [14, 15]. It has also been shown that local use of BPs inhibits mineralisation of bone tissue and new bone formation [16].
The microarchitectural structure of bone due to osteoclast-mediated resorption is of great clinical importance for many bone diseases. BP effects have been proven therapeutic in prevention of bone collapse and also in enhancement of implant fixation. Nevertheless, further large scale in vivo clinical trials are required to confirm all benefits concerning orthopaedic treatment.
We tried to determine whether there are any changes in the microarchitectural bone structure after local use of BP (Pamifos 60). The aim of the study was to see if BP-enriched cement used in rat models had a positive effect on bone formation.
Materials and methods
Animals
Wistar rats CRL(WI)WU BR were obtained from Mossakowski Medical Research Centre Polish Academy of Sciences. The experimental procedures were reviewed and approved by the Bioethical Committee of Animal Experimentation of the Medical University of Lublin.
Reagents
Bisphosphonate–pamidronate (Pamifos 60) was purchased from Vipharm (Warsaw, Poland). Bone cement was purchased from CMW 1, DePuy International Ltd, England.
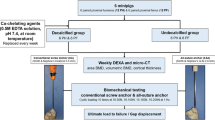
Research was performed on 40 adult male Wistar rats, with mean weight 240 g. Rats were divided into four groups, ten rats each, in two control groups and two experimental groups. Rats in experimental groups were implanted with BP-enriched cement into the bone. While in the control groups, rats were implanted with clean bone cement (without BP). Because experimental groups were operated upon at different times, each group was associated with its own dedicated control group.
Animal model
The animals were anaesthetised using thiopental with depth of anaesthesia being assessed by pedal reflex. After each animal was anaesthetised, it was placed in a supine position and the skin over both tibia bones was shaved and disinfected. A skin incision was made over the proximal part of the tibia. After exposing the proximal tibias identical doses of freshly mixed bone cement were pressurised into the bone canals through a pre-drilled hole using syringes with modified 2.1-mm needles. Twenty rats were given pure cement (control groups), while the remaining 20 rats were given cement mixed with BPs. The wound was closed using Vicryl sutures and staples. Three weeks after surgery, rats from the first control group and from the first experimental group were anaesthetised using thiopental (30 mg/kg), and proximal parts of tibial bones were taken for examination by micro-computed tomography. We performed the same procedure six weeks after surgery for the remaining rats in the second control and second experimental groups.
Micro-computed tomography
In micro-computed tomography the microCT SkyScan 1072 system was used. The SkyScan 1072 represented high-resolution desktop X-ray microtomography (Micro-CT) systems for in vitro scanning. Tomographic techniques were applied for the investigation of trabecular microarchitecture of the proximal physis of the tibial bone in all animals three and six weeks after surgery. Probes were located centrally on the tripod in the middle of the microtomography camera’s area of sight. Then probes were scanned (magnification 34×; pixel 8.42; rotation step 0.23; exposure 1.9 s; gain 1). Raw scans were reconstructed with the nRecon program (Skyscan, Belgium). Then the CTan program (Skyscan, Belgium) was used for detailed analysis.
Bone samples were selected from identical levels, beneath the lowest level of applied cement or BP-enriched cement implanted into the bone chosen during micro-CT before 3D reconstruction, as the threshold. The thresholding procedure allowed us to distinguish clearly between the cement or BP-enriched cement and the bone tissue (Fig. 1). The comparison of morphometric parameters extracted from the different images revealed specific changes in bone morphology. Morphometric analyses were based on 3D algorithms of identical ROI (regions of interest; Fig. 2) in all probes, whereby a cylinder was positioned in the centre of the proximal physis of the tibia bone. That cylinder was visually located at an identical distance from the most distal part of the implanted cement which was used as a benchmark. We used standardised nomenclature and symbols for bone histomorphometry [17]. In all microCT images variables such as bone volume (BV), trabecular thickness (Tb.Th), trabecular separation (Tb.Sp) and trabecular number (Tb.N) were analysed.
Statistical analysis
All data are presented as means ± SD. Differences and correlations were considered significant when p < 0.05. An ANOVA (analysis of variance) table was used for variance analysis to detect the existence of differences between the groups of rats that were investigated. All statistical calculations were performed using 6.0 STATISTICA software (StatSoft, Poland).
Results
The major finding of this study is that using BP-enriched cement results in distinct changes in bone microarchitecture (Fig. 3). High resolution micro-CT in vitro bone analysis showed an increase of bone volume (BV) in a group of rats implanted with BP-enriched cement after three weeks of treatment when compared to the control group. However there were no statistically significant differences between the groups studied (P = 0,444; Fig. 4). Nevertheless after six weeks of treatment statistics showed a significant increase of bone volume in rats implanted with BP-enriched cement (BV, P = 0.034; Fig. 5) compared to the group implanted with pure cement.
We also noted a statistically significant increase of trabecular thickness (Tb.Th) in both groups (three and six weeks) of rats implanted with BP-enriched cement compared to rats implanted with pure cement (Tb.Th, P = 0.003; Tb.Th, P = 0.014; Figs. 6 and 7). Though, three weeks after surgery we did not notice a significant decrease of trabecular separation in rats implanted with BP-enriched cement compared to rats implanted with cement without BP (Tb.Sp, P = 0.835; Fig. 8). Nonetheless six weeks after surgery we registered a significant decrease of that variable (Tb.Sp) between the control group and the group implanted with BP-enriched cement (P = 0.015; Fig. 9).
In micro-CT analysis performed three and six weeks after surgery in groups of rats implanted with BP-enriched cement we did not obtain a statistically significant increase of trabecular numbers (P = 0.706; P = 0.231; Fig. 10).
Discussion
The future potential use of BPs in orthopaedics encourages us to investigate the local use of this substance. Animal studies have shown that BPs inhibit bone resorption at the bone–implant interface [18]. BPs can also inhibit osteolysis by interacting directly with the osteoclasts. Experimental results made by Agholme et al. showed that soaking bone grafts in BP solution can prevent their resorption and increase the local bone density in rats. They indicated that local use of BPs might be a great factor against bone resorption; improving the bone’s microarchitecture and enhancing implant fixation without affecting the whole organism [15]. Experimental in vitro and in vivo research has shown great potential of using BPs in healing fractured bones, reducing osteoarthritis or enhancing bone allografts ingrowth [19–24].
Our micro-CT results showed only beneficial effects on the bone’s microarchitecture, which is similar to the observations of others [25]. In the rat model presented we did not notice any aggravation in the bone’s microarchitecture or other negative effects reported by other authors [26, 27].
High-resolution micro-computed tomography (microCT) imaging allowed us to assess bone morphology. Analyses based on 3D algorithms showed specific changes in three out of four variables that should be used to describe trabecular bone morphometry. Pamidronate implanted in cement did not affect the trabecular numbers, which is similar to other reports [27, 28]. Despite that fact some authors noticed significant changes in trabecular numbers during oral use of BPs in the paediatric population. Although they did not notice any changes in trabecular thickness, it was also noted that it might have been difficult to interpret because of the pathological process of specific diseases and the growth process in the young population [29]. We proved that local use of pamidronate (Pamifos 60) in orthopaedic cement significantly increases two variables: bone volume and trabecular thickness. We also noticed a significant decrease of trabecular separation. When reporting micro CT results Gao et al. presented similar results. Although, their implants before surgery had been rinsed in a solution containing various BPs: pamidronate, zoledronic acid or ibandronate [28]. Besides consistent changes in the parameters of trabecular microstructure they also reported effective induction of a greater restoration in the bone volume, which is similar to our findings.
Patients who need arthroplastic surgery are in high risk for osteopenia or osteoporosis [30]. Several recent studies have shown the utility of local application of various BPs on titanium implants [31–35]. In our opinion local BP treatment may be more beneficial considering some of the side effects connected with oral BP treatment [36, 37]. Furthermore, our micro-CT analysis showed great potential in the local use of BP-enriched cement. In the data presented, implanted BP-enriched cement simply changes the bone turnover in normal rats’ bone toward a positive balance between bone formation and bone resorption. As mentioned previously specific binding affinities and pharmacokinetics of pamidronate have different effects on osteoclasts and osteoblasts. However, its detailed mechanism of action is not completely understood. Pamidronate (Pamifos) appears to adsorb to calcium phosphate crystals in bone, blocking their dissolution by inhibiting osteoclast-mediated bone resorption. All those factors lead to positive effects on bone formation together with enhanced growth.
In our earlier report we proved that use of the bisphosphonate, Pamifos 60, that was present in the cement had a positive effect on bone turnover. BP stimulated increase in OPG and the RANKL decrease in the bone microenvironment markers in rat serum were important components of the mechanisms reducing bone resorption.
In this paper we also demonstrated the effectiveness of the idea of using BP-enriched cement in vitro in tibiae of rats. Our most significant findings based on micro-CT picture analysis allow us to start further work on more suitable applications of BP-enriched cement in humans. We believe that successful experiments will facilitate potential use of BP-enriched cement in clinical application.
References
Bock O, Börst H, Beller G, Armbrecht G, Degner C, Martus P, Roth HJ, Felsenberg D (2012) Impact of oral ibandronate 150 mg once monthly on bone structure and density in post-menopausal osteoporosis or osteopenia derived from in vivo μCT. Bone 50(1):317–324
Geoffroy V, Paschalis EP, Libouban H, Blouin S, Ostertag A, Chappard D, Cros M, Phipps R, de Vernejoul MC (2011) Effects of risedronate in Runx2 overexpressing mice, an animal model for evaluation of treatment effects on bone quality and fractures. Calcif Tissue Int 88(6):464–475
Reinholz GG, Getz B, Pederson L, Sanders ES, Subramaniam M, Ingle JN, Spelsberg TC (2000) Bisphosphonates directly regulate cell proliferation, differentiation, and gene expression in human osteoblasts. Cancer Res 60:6001–6007
Giuliani N, Pedrazzoni M, Negri G, Passeri G, Impicciatore M, Girasole G (1998) Bisphosphonates stimulate formation of osteoblast precursors and mineralized nodules in murine and human bone marrow cultures in vitro and promote early osteoblastogenesis in young and aged mice in vivo. Bone 22:455–461
Sahni M, Guenther HL, Fleisch H, Collin P, Martin TJ (1993) Bisphosphonates act on rat bone resorption through the mediation of osteoblasts. J Clin Invest 91:2004–2011
Fleisch H (1998) Bisphosphonates: mechanisms of action. Endcr Rev 19:80–100
Russell RGG, Rogers MJ (1999) Bisphosphonates: from the laboratory to the clinic and back again. Bone 25:97–106
Wilkinson JM, Little DG (2011) Bisphosphonates in orthopedic applications. Bone 49:95–102
Douglas DL, Russell RGG, Kanis JA, Preston CJ, Preston FE, Preston MA, Woodhead JS (1980) Effect of dichloromethylene diphosphonate in Paget’s disease of bone and in hypercalcaemia due to primary hyperparathyroidism or malignat disease. Lancet 1:10443–11047
Mundy GR, Yoneda T (1998) Bisphosphonates as anticancer drugs. N Engl J Med 339:398–400
Watts NB, Harris ST, Genant HK, Wasnich RD, Miller PD, Jackson RD, Licata AA, Ross P, Woodson GC, Yanover MJ, Mysiw WJ, Kohse L, Rao MB, Steiger P, Richmond B, Chesnut CH (1990) Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med 323:73–79
Kellinsalmi M, Monkkonen H, Monkkonen J et al (2005) In vitro comparison of clodronate, pamidronate, and zoledronic acid effects on rat osteoclast and human stem cell-derived osteoblasts. Basic Clin Pharmacol Toxicol 97:382–391
Plotkin LI, Manolagas SC, Bellido T (2006) Dissociation of the pro-apoptocic effects of bisphosphonates on osteoclasts from their anti-apoptotic effects on osteoblasts/osteocyters with novel analogs. Bone 39:443–452
Peter B, Gauthier O, Laib S, Bujoli B, Guicheux J, Janvier P et al (2006) Local delivery of bisphosphonate from coated orthopedic implants increases implant mechanical stability in osteoporotic rats. J Biomed Mater Res A 76:133–143
Agholme F, Aspenberg P (2009) Experimental results of combing bisphosphonates with allograft in a rat model. J Bone Joint Surg Br 91-B:670–675
Rodan GA (1997) Bone mass homeostasis and bisphosphonates action. Bone 20:1–4
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis A, Malluche H, Meunier PJ, Ott SM, Recker RR, Parfitt MA (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 28(1):2–17
Xuenong Z, Qingyun X, Haishengen L, Bunger M, Lind M, Bunger C (2003) Effect of alendronate on bone ingrowth into porous tantalum and carbon fiber interbody devices. Acta Orthop Scand 74(5):596–603
Aspenberg A, Astrand J (2002) Bone allograft pretreated with bisphosphonate are not resorbed. Acta Ortop Scand 73(1):20–23
Jee JH, Lee W, Lee BD (2010) The influence of alendronate on the healing of extraction sockets of ovariectomized rats assessed by in vivo microcomputed tomography. Oral Surg, Oral Med, Oral Pathol, Oral Radiol Endodontol 110(2):47–53
Jones MD, Tran CW, Li G, Maksymowych WP, Zernicke RF, Doschak MR (2010) In vivo microfocal computed tomography and micro-magnetic resonance imaging evaluation of antiresorptive and antiinflammatory drugs as preventive treatments of osteoarthritis in the rat. Arthritis Rheum 62(9):2726–2735
Allen MR (2011) The effects of bisphosphonates on jaw bone remodeling, tissue properties, and extraction healing. Odontology 99(1):8–17
Schindeler A, Birke O, Yu NY, Morse A, Ruys A, Baldock PA, Little DG (2011) Distal tibial fracture repair in a neurofibromatosis type 1-deficient mouse treated with recombinant bone morphogenetic protein and a bisphosphonate. J Bone Joint Surg Br 93(8):1134–1139
Qi M, Hu J, Li J, Li J, Dong W, Feng X, Yu J (2012) Effect of zoledronate acid treatment on osseointegration and fixation of implants in autologous iliac bone grafts in ovariectomized rabbits. Bone 50(1):119–127
Jakobsen T, Bass J, Bechtold JE, Elmengaard B, Soballe K (2007) Soaking morselized allograft bone in bisphosphonate can impair implant fixation. Clin Orthop 463:195–201
Baas J, Elmengaard B, Jensen TB et al (2005) The effect of pretreating morselized allograft bone with rhBMP-2 and/or pamidronate on the fixation of porous Ti and HA coated implants. Biomaterials 29:2915–2922
Seeman E, Delmas PD, Hanley DA, Sellmeyer D, Cheung AM, Shane E, Kearns A, Thomas T, Boyd SK, Boutroy S, Bogado C, Majumdar S, Fan M, Libanati C, Zanchetta J (2010) Microarchitectural deterioration of cortical and trabecular bone: differing effects of denosumab and alendronate. J Bone Miner Res 25(8):1886–1894
Gao Y, Zou S, Liu X, Bao C, Jing H (2009) The effect of surface immobilized bisphosphonates on the fixation of hydroxyapatite-coated titanium implants in ovariectomized rats. Biomaterials 30:1790–1796
Ward LM, Petryk A, Gordon C (2009) Use of bisphosphonates in treatment of pediatric osteoporosis. Int J Clin Rheumatol 4(6):657–672
Glowacki J, Hurwitz S, Thornhill TS, Kelly M, LeBoff MS (2003) Osteoporosis and vitamin-D deficiency among posmenopausal women with osteoarthritis undergoing total hip arthroplasty. J Bone Joint Surg Am 85:2371–2377
Wermelin K, Suska F, Tengvall P, Thomsen P, Spenberg P (2008) Stainless steel screws with bisphosphonates gave stronger fixation and more surrounding bone. Histomorphometry in rats. Bone 42:365–371
Youshinari M, Oda Y, Ueki H, Yokose S (2002) Immobilization of bisphosphonates on surface modified titanium. Biomaterials 23:2870–2885
Youshinari M, Oda Y, Inoue T, Matsuzaka T, Shimono M (2001) Bone response to calcium phosphate-coated and bisphosphonates-immobilized titanium implants. Biomaterials 22:709–715
Tanzer M, Karabasz D, Krygier JJ, Cohen R, Bobyn JD (2005) Bone augmentation around and within porosus implants by local bisphosphonates elution. Clin Orthop Relat Res 441:30–39
Kajiwara H, Yamaza T, Yoshinari M, Goto T, Iyama S, Atsuta I et al (2005) The bisphosphonate pamidronate on the surface of titanium stimulates bone formation around tibial implants in rats. Biomaterials 26:581–587
Marx RE (2003) Pamidronate (Aredia) and zoledronate (Zometa) induced a vascular necrosis of the jaw: a growing epidemic. J Oral Maxillofac Surg 61:1115–1117
Migliorati CA (2003) Bisphosphonates and oral cavity bone necrosis. J Clin Oncol 21:4253–4254
Acknowledgments
This paper would not have been possible without the support and help of PhD Marek Zaluski, MO, USA and Ashwani Srivastava MD student, CA, USA. The authors wish to express their gratitude to them. They were abundantly helpful and offered invaluable assistance and support during preparing of that article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Matuszewski, Ł., Turżańska, K., Matuszewska, A. et al. Effect of implanted bisphosphonate-enriched cement on the trabecular microarchitecture of bone in a rat model using micro-computed tomography. International Orthopaedics (SICOT) 37, 1187–1193 (2013). https://doi.org/10.1007/s00264-013-1855-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-1855-z