Abstract
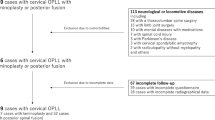
Between January 2000 and December 2003, a total of 83 patients (64 men and 19 women, average age: 56.4 years, range: 42–78 years) who underwent posterior laminectomy and instrumented fusion for ossification of the posterior longitudinal ligament (OPLL) were included in this study to investigate the long-term outcome of this surgical option and clarify which factors affect the prognosis. After an average 4.8-year follow-up, the mean Japanese Orthopaedic Association (JOA) score significantly increased from 9.2 ± 1.3 points before operation to 14.2 ± 0.9 points at the latest follow-up (P < 0.01). The improvement rate (IR) of neurological function ranged from 11.1 to 87.5%, with a mean of 62.4 ± 13.2%. Among 83 patients, 59 (71.1%) patients had a good prognosis (IR ≥ 50%), and the other 24 (28.9%) patients had a poor prognosis (IR < 50%). Postoperative nerve root palsy was the main complication in this series. Radiographic study showed that whilst improving cervical lordosis could provide a better decompression effect and good prognosis, it could have simultaneously contributed to the high incidence of postoperative nerve root palsy.
Résumé
Entre janvier 2000 et décembre 2003, 83 patients (64 hommes et 19 femmes) dont la moyenne d’âge était de 56,4 ans (42 – 78) ont bénéficié d’une laminectomie supérieure avec instrumentation et greffe pour une opération visant une OPLL avec évaluation du pronostic à long terme et détermination des facteurs pouvant le modifier. Après un suivi de 4 à 8 ans, le score de la JOA a été nettement amélioré passant de 9,2 (± 1,3) avant l’opération à 14,2 (± 0,9), au dernier suivi (p < 0,01). Le taux d’amélioration neurologique (IR) est passé de 11,1% à 87,5% avec une moyenne de 62,4% ± 13,2%. Parmi ces 83 patients, 59 (71,1%) avaient un bon pronostic (IR 50%) et les autres, 24 (28,9%) avaient un mauvais pronostic (IR < 50%). La paralysie des fibres nerveuses est la complication la plus importante dans cette série. L’étude radiographique montre que l’amélioration de la lordose cervicale permet un effet de décompression plus important et un meilleur pronostic mais a contribué de façon simultanée à un taux important de paralysie des racines nerveuses en post-opérartoire.


Similar content being viewed by others
References
Albert TJ, Vaccaro A (1998) Postlaminectomy kyphosis. Spine 23:2738–2745
Baba H, Imura S, Kawahara N et al (1995) Osteoplastic laminoplasty for cervical myeloradiculopathy secondary to ossification of the posterior longitudinal ligament. Int Orthop 19:40–45
Choi S, Lee SH, Lee JY et al (2005) Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech 18:309–314
Epstein N (2001) Anterior approaches to cervical spondylosis and ossification of the posterior longitudinal ligament: review of operative technique and assessment of 65 multilevel circumferential procedures. Surg Neurol 55:313–324
Hee HT, Majd ME, Holt RT et al (2003) Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech 16:1–9
Heller JG, Edwards CC II, Murakami H et al (2001) Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine 26:1330–1336
Houten JK, Cooper PR (2003) Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression and neurological outcome. Neurosurgery 52:1081–1088
Iwasaki M, Okuda S, Miyauchi A et al (2007) Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: clinical results and limitations of laminoplasty. Spine 32:647–653
Kawagchi Y, Kanamori M, Ishihara H et al (2001) Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am 83-A:1798–1802
Kumar VG, Rea GL, Mervis LJ et al (1999) Cervical spondylotic myelopathy: functional and radiographic long-term outcome after laminectomy and posterior fusion. Neurosurgery 44:771–778
Macdonald RL, Fehlings MG, Tator CH et al (1997) Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg 86:990–997
Masaki Y, Yamazaki M, Okawa A et al (2007) An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech 20:7–13
Matsunaga S, Sakou T, Taketomi E et al (2004) Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg 100(Suppl 3):245–248
Mizuno J, Nakagawa H (2006) Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J 6:282–288
Ogawa Y, Toyama Y, Chiba K et al (2004) Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 1:168–174
Sakaura H, Hosono N, Mukai Y et al (2003) C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine 28:2447–2451
Saruhashi Y, Hukuda S, Katsuura A et al (1999) A long-term follow-up study of cervical spondylotic myelopathy treated by “French window” laminoplasty. J Spinal Disord 12:99–101
Tani T, Ushida T, Ishida K et al (2002) Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine 27:2491–2498
Vaccro AR, Falatyn SP, Scuderi GJ et al (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11:410–415
Yamazaki A, Homma T, Uchiyama S et al (1999) Morphologic limitations of posterior decompression by midsagittal splitting method for myelopathy caused by ossification of the posterior longitudinal ligament in the cervical spine. Spine 24:32–34
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Y., Guo, Y., Chen, D. et al. Long-term outcome of laminectomy and instrumented fusion for cervical ossification of the posterior longitudinal ligament. International Orthopaedics (SICOT) 33, 1075–1080 (2009). https://doi.org/10.1007/s00264-008-0609-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0609-9