Abstract
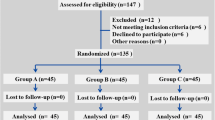
The amount of blood loss in a primary cemented total knee arthroplasty (TKA) seems to vary in different reported studies. We carried out a prospective study to determine the factors affecting the peri-operative blood loss, hidden blood loss and blood transfusion requirements in a primary cemented total knee arthroplasty. The factors analysed were gender, diagnosis, tourniquet time and body mass index (BMI). We included a total of 66 consecutive patients who underwent primary TKA by a single surgeon (A.M). There was significantly more peri-operative blood loss in male patients than in females (p=0.001, Student’s t test). The patients with rheumatoid arthritis did not show any statistical difference in peri-operative blood loss compared with that in patients with osteoarthritis. The tourniquet time and the surgical time showed a positive correlation with peri-operative blood loss. The BMI did not show any correlation with peri-operative blood loss. The incidence of blood transfusion was significantly higher in patients with rheumatoid knees as their pre-operative haemoglobin value was low. The amount of hidden blood loss in our series was 38%. We concluded that gender and tourniquet time plays a role in blood loss in TKA, but diagnosis (advanced osteoarthritis [OA] or rheumatoid arthritis (RA) does not. The blood transfusion depends on both pre-operative haemoglobin value and intra-operative blood loss. The post-operative transfusion trigger can be brought to 8.0 g% in a haemodynamically stable patient.
Résumé
La quantité de perte de sang dans une prothèse totale du genou de première intention cimentée est variable suivant les différentes études. Nous avons réalisé une étude prospective pour déterminer quels étaient les facteurs de la perte sanguine péri-opératoire et quels étaient les facteurs qui entraient dans la nécessité d’une transfusion, après une prothèse totale du genou de première intention. Les facteurs analysés ont été le sexe, le diagnostic, l’utilisation d’un garrot, le BMI. Nous avons inclus dans cette étude, 66 patients consécutifs, opérés par le même chirurgien (A.M.). Il y a eu une de façon significative une augmentation des pertes sanguines péri-opératoires chez les patients de sexe masculin (p=0.001, Student’s t test). Les patients présentant une arthrite rhumatoïde n’ont pas montré de différences significatives dans la perte de sang, comparés aux patients opérés pour gonarthrose. Le temps de garrot et le temps opératoire sont en corrélation avec les pertes de sang péri-opératoires, l’augmentation du BMI ne semble pas avoir de corrélation avec la perte sanguine. L’incidence des transfusions est de façon significative plus élevée chez les patients opérés pour arthrite rhumatoïde du genou et dont l’hémoglobine préopératoire était basse. Nous pouvons en conclure que le sexe et le temps de garrot ont une responsabilité dans la perte de sang dans la prothèse totale du genou mais, certainement pas l’étiologie. La nécessité de transfusion dépend du taux d’hémoglobine pré-opératoire et des pertes sanguines per-opératoires. Une transfusion peut être pratiquée pour 8.0 g% chez un patient haemodynamiquement stable.


Similar content being viewed by others
References
Aglietti P, Baldini A, Vena LM Abbate R, Fedi S, Falciani M (2000) Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res 371:169–177
Albert GM, Matthew PF, Daniel EM, Parsons JR (1990) Perioperative blood loss associated with total knee arthroplasty. J Bone Joint Surg Am 72:1010–1012
Benoni G, Fredin H (1996) Fibrinolytic inhibition with transexamic acid reduces blood loss and blood transfusion after knee arthroplasty. J Bone Joint Surg Br 78:434–440
Bernstein LH, Coles M, Granata A (1997) The Bridgeport Hospital experience with autologous transfusion in orthopedic surgery. Orthopedics 20:677–680
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RE (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 81:2–10
Capraro L (1998) Transfusion practices in primary total joint replacement in Finland. Vox Sang 75:1–6
Cohen JA, Brecher ME (1995) Preoperative autologous blood donation: benefit or detriment; a mathematical analysis. Transfusion 35:640–644
Cushner FD, Friedman RJ (1991) Blood loss in total knee arthroplasty. Clin Orthop Relat Res 269:98–101
Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID (1981) Blood loss with knee joint replacement. J R Coll Edinb 26:245
Faris PM, Spence RK, Larholt KM, Sampson AR, Frei D (1999) The predictive power of baseline hemoglobin for transfusion risk in surgery patients. Orthopedics 22 [1 Suppl]:S135–S140
Fiebig E (1998) Safety of the blood supply. Clin Orthop Relat Res 357:6–18
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anaesthesiology 58:277–280
Han CD, Shin DE (1997) Post operative blood salvage and reinfusion after total joint arthroplasty. J Arthroplasty 12:511–516
Hersekli MA, Akpinar S, Okoc G, Ozalay M et al (2004) The timing of tourniquet release and its influence on blood loss after total knee arthroplasty. Int Orthop 28:138–141
Keating EM, Meding JB, Faris PM, Ritter MA (1998) Predictors of transfusion risk in elective knee surgery. Clin Orthop Relat Res 357:50–59
Macfarlane BJ, Mar XL, Anquist K (1988) Analysis of a protocol for an autologous blood transfusion program for total joint replacement surgery. Can J Surg 31:126–179
Manner PA, Rubash HE, Herndon JH (1998) Future trends in transfusion. Clin Orthop Relat Res 357:101–115
Mcvay PA, Toy PT (1996) Very severe outcomes associated with autologous blood donation [letter]. Transfusion 36:761
Mollison PL, Engelfriet CP, Contreras M (1993) Blood transfusion in clinical medicine, 9th edn. Blackwell, Oxford
Mylod AG, France MP, Muser DE, Parsons JR (1990) Perioperative blood loss associated with total knee arthroplasty. J Bone Joint Surg Am 72:1010–1012
Page MH, Shepherd BD, Harrison JM (1984) Reduction of blood loss in knee arthroplasty. Aust N Z J Surg 54:141
Pattison E, Protheroe K, Pringle RM, Kennedy AC, Dick WC (1973) Reduction in hemoglobin after knee joint surgery. Ann Rheum Dis 32:582–584
Raut VV, Stone MH, Wroblewski BM (1993) Reduction of postoperative blood loss after press-fit condylar knee arthroplasty with use of a femoral intramedullary plug. J Bone Joint Surg Am 75:1356–1357
Reilly TJ, Ivan AG, William P, Maureen R (1986) The use of postoperative suction drainage in total knee arthroplasty. Clin Orthop Relat Res 208:238–252 July
Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 7:151–155
Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S (2001) Timing of the administration of transexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br 83:702–705
Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B (2002) The effect of tourniquet use in total knee arthroplasty. Int Orthop 26:306–309
Walker RH (1987) Transfusion risks. Am J Clin Pathol 88:374
Yomtovian R (1996) Autologous transfusion complications. In: Popovsky MA (ed) Transfusion reactions. American Association of Blood Banks Press, Bethesda, pp 237–280
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prasad, N., Padmanabhan, V. & Mullaji, A. Blood loss in total knee arthroplasty: an analysis of risk factors. International Orthopaedics (SICO 31, 39–44 (2007). https://doi.org/10.1007/s00264-006-0096-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-006-0096-9