Abstract
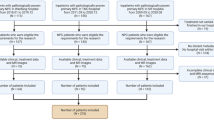
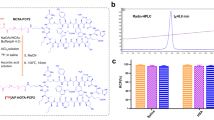
Enhanced tumor glycolytic activity is a mechanism by which tumors induce an immunosuppressive environment to resist adoptive T cell therapy; therefore, methods of assessing intratumoral glycolytic activity are of considerable clinical interest. In this study, we characterized the relationships among tumor 18F-fluorodeoxyglucose (FDG) retention, tumor metabolic and immune phenotypes, and survival in patients with resected non-small cell lung cancer (NSCLC). We retrospectively analyzed tumor preoperative positron emission tomography (PET) 18F-FDG uptake in 59 resected NSCLCs and investigated correlations between PET parameters (SUVMax, SUVTotal, SUVMean, TLG), tumor expression of glycolysis- and immune-related genes, and tumor-associated immune cell densities that were quantified by immunohistochemistry. Tumor glycolysis-associated immune gene signatures were analyzed for associations with survival outcomes. We found that each 18F-FDG PET parameter was positively correlated with tumor expression of glycolysis-related genes. Elevated 18F-FDG SUVMax was more discriminatory of glycolysis-associated changes in tumor immune phenotypes than other 18F-FDG PET parameters. Increased SUVMax was associated with multiple immune factors characteristic of an immunosuppressive and poorly immune infiltrated tumor microenvironment, including elevated PD-L1 expression, reduced CD57+ cell density, and increased T cell exhaustion gene signature. Elevated SUVMax identified immune-related transcriptomic signatures that were associated with enhanced tumor glycolytic gene expression and poor clinical outcomes. Our results suggest that 18F-FDG SUVMax has potential value as a noninvasive, clinical indicator of tumor immunometabolic phenotypes in patients with resectable NSCLC and warrants investigation as a potential predictor of therapeutic response to immune-based treatment strategies.






Similar content being viewed by others
Abbreviations
- 18F-FDG:
-
18F-fluorodeoxyglucose
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DFS:
-
Disease-free survival
- DISTHG:
-
Downregulated Immune Signature of Tumors with High Glycolysis
- FFPE:
-
Formalin-fixed, paraffin-embedded
- HR:
-
Hazard ratio
- ICI:
-
Immune checkpoint inhibitor
- IHC:
-
Immunohistochemistry
- IQR:
-
Interquartile range
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PET:
-
Positron emission tomography
- PROSPECT:
-
Profiling of Resistance Patterns and Oncogenic Signaling Pathways in Evaluation of Cancers of the Thorax
- SUV:
-
Standardized uptake value
- TAIC:
-
Tumor-associated immune cell
- TLG:
-
Total lesion glycolysis
- UISTHG:
-
Upregulated Immune Signature of Tumors with High Glycolysis
- VOI:
-
Volume of interest
References
Borghaei H, Paz-Ares L, Horn L et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373:1627–1639. https://doi.org/10.1056/NEJMoa1507643
Brahmer J, Reckamp KL, Baas P et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N Engl J Med 373:123–135. https://doi.org/10.1056/NEJMoa1504627
Reck M, Rodriguez-Abreu D, Robinson AG et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375:1823–1833. https://doi.org/10.1056/NEJMoa1606774
Forde PM, Chaft JE, Smith KN et al (2018) Neoadjuvant PD-1 blockade in resectable lung cancer. N Engl J Med 378:1976–1986. https://doi.org/10.1056/NEJMoa1716078
Renner K, Singer K, Koehl GE, Geissler EK, Peter K, Siska PJ, Kreutz M (2017) Metabolic hallmarks of tumor and immune cells in the tumor microenvironment. Front Immunol. https://doi.org/10.3389/fimmu.2017.00248
Chang C-H, Qiu J, O’Sullivan D et al (2015) Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell 162:1229–1241. https://doi.org/10.1016/j.cell.2015.08.016
Fischer K, Hoffmann P, Voelkl S et al (2007) Inhibitory effect of tumor cell–derived lactic acid on human T cells. Blood 109:3812–3819. https://doi.org/10.1182/blood-2006-07-035972
Estrella V, Chen T, Lloyd M et al (2013) Acidity generated by the tumor microenvironment drives local invasion. Cancer Res 73:1524–1535. https://doi.org/10.1158/0008-5472.can-12-2796
Walenta S, Wetterling M, Lehrke M, Schwickert G, Sundfør K, Rofstad EK, Mueller-Klieser W (2000) High lactate levels predict likelihood of metastases, tumor recurrence, and restricted patient survival in human cervical cancers. Cancer Res 60:916–921
Cascone T, McKenzie JA, Mbofung RM et al (2018) Increased tumor glycolysis characterizes immune resistance to adoptive T cell therapy. Cell Metab 27:977–87.e4. https://doi.org/10.1016/j.cmet.2018.02.024
Liu J, Dong M, Sun X, Li W, Xing L, Yu J (2016) Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: a meta-analysis. PLoS ONE 11:e0146195. https://doi.org/10.1371/journal.pone.0146195
Pak K, Cheon GJ, Nam HY, Kim SJ, Kang KW, Chung JK, Kim EE, Lee DS (2014) Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: A systematic review and meta-analysis. J Nucl Med 55:884–890. https://doi.org/10.2967/jnumed.113.133801
Im HJ, Pak K, Cheon GJ, Kang KW, Kim SJ, Kim IJ, Chung JK, Kim EE, Lee DS (2015) Prognostic value of volumetric parameters of 18F-FDG PET in non-small-cell lung cancer: a meta-analysis. Eur J Nucl Med Mol Imaging 42:241–251. https://doi.org/10.1007/s00259-014-2903-7
Kwon HR, Pahk K, Park S et al (2019) Prognostic value of metabolic information in advanced gastric cancer using preoperative (18)F-FDG PET/CT. Nucl Med Mol Imaging 53:386–395. https://doi.org/10.1007/s13139-019-00622-w
Bruzzi JF, Munden RF (2006) PET/CT imaging of lung cancer. J Thorac Imaging 21:123–136
Cardnell RJG, Behrens C, Diao L et al (2015) An integrated molecular analysis of lung adenocarcinomas identifies potential therapeutic targets among TTF1-negative tumors, including DNA repair proteins and Nrf2. Clin Cancer Res 21:3480–3491. https://doi.org/10.1158/1078-0432.ccr-14-3286
Skoulidis F, Byers LA, Diao L et al (2015) Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer Discov 5:860–877. https://doi.org/10.1158/2159-8290.cd-14-1236
Tang H, Xiao G, Behrens C et al (2013) A 12-gene set predicts survival benefits from adjuvant chemotherapy in non-small cell lung cancer patients. Clin Cancer Res 19:1577–1586. https://doi.org/10.1158/1078-0432.ccr-12-2321
Mohammed N, Kestin LL, Grills IS, Battu M, Fitch DL, C-yO W, Margolis JH, Chmielewski GW, Welsh RJ (2011) Rapid disease progression with delay in treatment of non–small-cell lung cancer. Int J Radiat Oncol Biol Phys 79:466–472. https://doi.org/10.1016/j.ijrobp.2009.11.029
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, Postmus PE, Rusch V, Sobin L (2007) The IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2:706–714. https://doi.org/10.1097/JTO.0b013e31812f3c1a
Mhlanga JC, Chirindel A, Lodge MA, Wahl RL, Subramaniam RM (2018) Quantitative PET/CT in clinical practice: assessing the agreement of PET tumor indices using different clinical reading platforms. Nucl Med Commun 39:154–160. https://doi.org/10.1097/mnm.0000000000000786
Werner-Wasik M, Nelson AD, Choi W et al (2012) What is the best way to contour lung tumors on PET scans? Multiobserver validation of a gradient-based method using a NSCLC digital PET phantom. Int J Radiat Oncol Biol Phys 82:1164–1171. https://doi.org/10.1016/j.ijrobp.2010.12.055
Nilsson MB, Sun H, Diao L et al (2017) Stress hormones promote EGFR inhibitor resistance in NSCLC: implications for combinations with beta-blockers. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aao4307
Cesano A (2015) nCounter® PanCancer immune profiling panel (NanoString Technologies Inc, Seattle, WA). J Immunother Cancer 3:42. https://doi.org/10.1186/s40425-015-0088-7
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful spproach to multiple testing. J R Stat Soc Ser B (Methodological) 57:289–300
Law CW, Alhamdoosh M, Su S, Dong X, Tian L, Smyth GK, Ritchie ME (2016) RNA-seq analysis is easy as 1-2-3 with limma, Glimma and edgeR. F1000Res. https://doi.org/10.12688/f1000research.9005.3
Krämer A, Green J, Pollard J Jr, Tugendreich S (2013) Causal analysis approaches in ingenuity pathway analysis. Bioinformatics 30:523–530. https://doi.org/10.1093/bioinformatics/btt703
Danaher P, Warren S, Lu R, Samayoa J, Sullivan A, Pekker I, Wallden B, Marincola FM, Cesano A (2018) Pan-cancer adaptive immune resistance as defined by the tumor inflammation signature (TIS): results from the cancer genome atlas (TCGA). J Immunother Cancer 6:63. https://doi.org/10.1186/s40425-018-0367-1
Jerby-Arnon L, Shah P, Cuoco MS et al (2018) A cancer cell program promotes T cell exclusion and resistance to checkpoint blockade. Cell 175:984–97.e24. https://doi.org/10.1016/j.cell.2018.09.006
Parra ER, Behrens C, Rodriguez-Canales J et al (2016) Image analysis-based assessment of PD-L1 and tumor-associated immune cells density supports distinct intratumoral microenvironment groups in non-small cell lung carcinoma patients. Clin Cancer Res 22:6278–6289. https://doi.org/10.1158/1078-0432.ccr-15-2443
Kadara H, Choi M, Zhang J et al (2017) Whole-exome sequencing and immune profiling of early-stage lung adenocarcinoma with fully annotated clinical follow-up. Ann Oncol 28:75–82. https://doi.org/10.1093/annonc/mdw436
Győrffy B, Surowiak P, Budczies J, Lánczky A (2013) Online survival analysis software to assess the prognostic value of biomarkers using transcriptomic data in non-small-cell lung cancer. PLoS ONE 8:e82241. https://doi.org/10.1371/journal.pone.0082241
R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria. https://www.R-project.org/.
Chung AS, Wu X, Zhuang G et al (2013) An interleukin-17–mediated paracrine network promotes tumor resistance to anti-angiogenic therapy. Nat Med 19:1114. https://doi.org/10.1038/nm.3291
Charles KA, Kulbe H, Soper R et al (2009) The tumor-promoting actions of TNF-alpha involve TNFR1 and IL-17 in ovarian cancer in mice and humans. J Clin Invest 119:3011–3023. https://doi.org/10.1172/jci39065
Alfaro C, Teijeira A, Oñate C et al (2016) Tumor-produced interleukin-8 attracts human myeloid-derived suppressor cells and elicits extrusion of neutrophil extracellular traps (NETs). Clin Cancer Res 22:3924–3936. https://doi.org/10.1158/1078-0432.Ccr-15-2463
Wellenstein MD, de Visser KE (2018) Cancer-cell-intrinsic mechanisms shaping the tumor immune landscape. Immunity 48:399–416. https://doi.org/10.1016/j.immuni.2018.03.004
Liu J, Zhang C, Wu R, Lin M, Liang Y, Liu J, Wang X, Yang B, Feng Z (2015) RRAD inhibits the Warburg effect through negative regulation of the NF-KB signaling. Oncotarget 6:14982–14992. https://doi.org/10.18632/oncotarget.3719
Wang H, Nicolay BN, Chick JM et al (2017) The metabolic function of cyclin D3–CDK6 kinase in cancer cell survival. Nature 546:426. https://doi.org/10.1038/nature22797
Brand A, Singer K, Koehl Gudrun E et al (2016) LDHA-associated lactic acid production blunts tumor immunosurveillance by T and NK cells. Cell Metab 24:657–671. https://doi.org/10.1016/j.cmet.2016.08.011
Vander Heiden MG, DeBerardinis RJ (2017) Understanding the intersections between metabolism and cancer biology. Cell 168:657–669. https://doi.org/10.1016/j.cell.2016.12.039
Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324:1029–1033. https://doi.org/10.1126/science.1160809
Timm KN, Kennedy BW, Brindle KM (2016) Imaging tumor metabolism to assess disease progression and treatment response. Clin Cancer Res 22:5196–5203. https://doi.org/10.1158/1078-0432.ccr-16-0159
Mamede M, Higashi T, Kitaichi M et al (2005) 18F-FDG Uptake and PCNA, Glut-1, and Hexokinase-II expressions in cancers and inflammatory lesions of the lung. Neoplasia (New York, N. Y.) 7:369–379. https://doi.org/10.1593/neo.04577
Kaira K, Serizawa M, Koh Y et al (2014) Biological significance of 18F-FDG uptake on PET in patients with non-small-cell lung cancer. Lung Cancer 83:197–204. https://doi.org/10.1016/j.lungcan.2013.11.025
Zhou X, Chen R, Xie W, Ni Y, Liu J, Huang G (2014) Relationship between 18F-FDG accumulation and lactate dehydrogenase A expression in lung adenocarcinomas. J Nucl Med 55:1766–1771. https://doi.org/10.2967/jnumed.114.145490
Goodwin J, Neugent ML, Lee SY et al (2017) The distinct metabolic phenotype of lung squamous cell carcinoma defines selective vulnerability to glycolytic inhibition. Nat Commun 8:15503. https://doi.org/10.1038/ncomms15503
Boroughs LK, DeBerardinis RJ (2015) Metabolic pathways promoting cancer cell survival and growth. Nat Cell Biol 17:351. https://doi.org/10.1038/ncb3124
Contractor KB, Aboagye EO (2009) Monitoring predominantly cytostatic treatment response with 18F-FDG PET. J Nucl Med 50:97S–105S. https://doi.org/10.2967/jnumed.108.057273
Ottensmeier CH, Perry KL, Harden EL et al (2016) Upregulated glucose metabolism correlates inversely with CD8+ T-cell infiltration and survival in squamous cell carcinoma. Cancer Res 76:4136–4148. https://doi.org/10.1158/0008-5472.can-15-3121
Soo RA, Chen Z, Yan Teng RS, Tan HL, Iacopetta B, Tai BC, Soong R (2018) Prognostic significance of immune cells in non-small cell lung cancer: meta-analysis. Oncotarget 9:24801–24820. https://doi.org/10.18632/oncotarget.24835
Tang H, Wang Y, Chlewicki LK, Zhang Y, Guo J, Liang W, Wang J, Wang X, Fu Y-X (2016) Facilitating T cell infiltration in tumor microenvironment overcomes resistance to PD-L1 blockade. Cancer Cell 29:285–296. https://doi.org/10.1016/j.ccell.2016.02.004
Lopci E, Toschi L, Grizzi F et al (2016) Correlation of metabolic information on FDG-PET with tissue expression of immune markers in patients with non-small cell lung cancer (NSCLC) who are candidates for upfront surgery. Eur J Nucl Med Mol Imaging 43:1954–1961. https://doi.org/10.1007/s00259-016-3425-2
Kaira K, Higuchi T, Naruse I et al (2018) Metabolic activity by (18)F-FDG-PET/CT is predictive of early response after nivolumab in previously treated NSCLC. Eur J Nucl Med Mol Imaging 45:56–66. https://doi.org/10.1007/s00259-017-3806-1
Usmanij EA, de Geus-Oei LF, Troost EG, Peters-Bax L, van der Heijden EH, Kaanders JH, Oyen WJ, Schuurbiers OC, Bussink J (2013) 18F-FDG PET early response evaluation of locally advanced non-small cell lung cancer treated with concomitant chemoradiotherapy. J Nucl Med 54:1528–1534. https://doi.org/10.2967/jnumed.112.116921
Spigel DRCJ, Gettinger S, Chao BH, Dirix L, Schmid P et al (2018) FIR: Efficacy, safety, and biomarker analysis of a phase II open-label study of atezolizumab in PD-L1-selected patients with NSCLC. J Thorac Oncol 13:1733–1742
Parra ER, Villalobos P, Behrens C et al (2018) Effect of neoadjuvant chemotherapy on the immune microenvironment in non-small cell lung carcinomas as determined by multiplex immunofluorescence and image analysis approaches. J Immunother Cancer 6:48. https://doi.org/10.1186/s40425-018-0368-0
Cascone T, William WN, Weissferdt A et al (2019) Neoadjuvant nivolumab (N) or nivolumab plus ipilimumab (NI) for resectable non-small cell lung cancer (NSCLC): Clinical and correlative results from the NEOSTAR study. J Clin Oncol 37: suppl; abstr 8504. https://doi.org/10.1200/JCO.2019.37.15_suppl.8504
Kwiatkowski DJ, Rusch VR, Chaft JE et al (2019) Neoadjuvant atezolizumab in resectable non-small cell lung cancer (NSCLC): interim analysis and biomarker data from a multicenter study (LCMC3). J Clin Oncol 37: suppl; abstr 8503. https://doi.org/10.1200/JCO.2019.37.15_suppl.8503
Provenico M, Nadal E, Insa A et al (2019) Neoadjuvant chemo-immunotherapy for the treatment of stage IIIA resectable non-small cell lung cancer (NSCLC): a phase II multicenter exploratory study-Final data of patients who underwent surgical assessment. J Clin Oncol 37: suppl; abstr 8509. https://doi.org/10.1200/JCO.2019.37.15_suppl.8509
Gandhi L, Rodríguez-Abreu D, Gadgeel S et al (2018) Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med 378:2078–2092. https://doi.org/10.1056/NEJMoa1801005
Lopes G, Wu Y-L, Kudaba I et al. (2018) Pembrolizumab (pembro) versus platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1%: Open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 36: LBA4-LBA. https://doi.org/10.1200/JCO.2018.36.18_suppl.LBA4
Faubert B, Li KY, Cai L et al (2017) Lactate metabolism in human lung tumors. Cell 171:358–371. https://doi.org/10.1016/j.cell.2017.09.019
Momcilovic M, Jones A, Bailey ST et al (2019) In vivo imaging of mitochondrial membrane potential in non-small-cell lung cancer. Nature 575:380–384. https://doi.org/10.1038/s41586-019-1715-0
Hensley CT, Faubert B, Yuan Q et al (2016) Metabolic heterogeneity in human lung tumors. Cell 164:681–694. https://doi.org/10.1016/j.cell.2015.12.034
Chen PH, Cai L, Huffman K et al (2019) Metabolic diversity in human non-small cell lung cancer cells. Mol Cell 76:838–51.e5. https://doi.org/10.1016/j.molcel.2019.08.028
Acknowledgements
The authors appreciate the assistance of Mr. Alex Liu with the Division of Information Services, Oncology Care and Research IS at MD Anderson Cancer Center, and Mr. Donald Norwood with the Department of Scientific Publications at MD Anderson Cancer Center for his editorial assistance.
Funding
This work was supported in part by the National Cancer Institute (5 P50 CA070907; P50 CA221703; R01 CA187076; R01 CA184845, P30CA01667), the Cancer Prevention and Research Institute of Texas (RP170401), the American Society of Clinical Oncology 2018 Career Development Award (12895), the Department of Defense (W81XWH-07-1-0306), and the Bob Mayberry Foundation. This work was also supported in part by the Bruton Endowed Chair in Tumor Biology Funds, and the generous philanthropic contributions to the University of Texas MD Anderson Cancer Center Lung Cancer Moon Shot Program, the Khalifa Scholars Program (from Khalifa Bin Zayed Al Nahyan Foundation), the Advanced Scholar Program (from CG Johnson Foundation), and the Physician Scientist Program (from T.J. Martell Foundation).
Author information
Authors and Affiliations
Contributions
WP and TC contributed to conception and design. TC, WP, BA, and ERP contributed to development of methodology. TC, WP, BA, KGM, HK, ERP, PV, CB, AR, YW, JW, AW, CAM, and JF contributed to data acquisition. TC, WP, KGM, BA, ERP, PV, CB, AR, YW, AW, JJL, and DPW contributed to analysis and interpretation of data. KGM, BA, BS, MCBG, ERP, PV, HK, CB, AR, AAV, WLH, SGS, WNW, DLG, IIW, PH, JVH, BWC, YW, JW, JJL, DPW, AW, CAM, JF, GLW, DPW, WP, and TC wrote, reviewed, and revised the manuscript. TC, WP, JVH, and IIW contributed to administrative, technical, or material support. WP and TC contributed to study supervision.
Corresponding authors
Ethics declarations
Conflict of interest
M.C.B. Godoy has received research funding from Siemens Healthcare. W.N. William has received honoraria/speaker’s fees and/or participated in advisory boards from Roche/Genentech, Bristol-Myers Squibb, Eli Lilly, Merck, AstraZeneca, and Pfizer. D.L. Gibbons has received research funding from AstraZeneca, Janssen, and Takeda and has participated in advisory boards for AstraZeneca and Sanofi. P. Hwu is a consultant and/or has participated in advisory boards for Immatics, Dragonfly, Sanofi, and GlaxoSmithKline. S.G. Swisher has participated in advisory committees for Ethicon and for the Peter MacCallum Cancer Center. B.S. receives consulting fees from Bristol-Myers Squibb. J.V. Heymach has received research support from AstraZeneca, Bayer, GlaxoSmithKline, and Spectrum; participated in advisory committees for AstraZeneca, Boehringer Ingelheim, Exelixis, Genentech, GlaxoSmithKline, Guardant Health, Hengrui, Lilly, Novartis, Specrtum, EMD Serono, and Synta; and received royalties and/or licensing fees from Spectrum. P. Hwu and W. Peng have received research funding in the form of grants to MD Anderson Cancer Center from GlaxoSmith Kline. T. Cascone has received speaker’s fees from the Society for Immunotherapy of Cancer and Bristol-Myers Squibb; receives consulting/advisory role fees from MedImmune, Bristol-Myers Squibb and EMD Serono, and research funding to MD Anderson Cancer Center from Boehringer Ingelheim, MedImmune and Bristol-Myers Squibb. No potential conflicts of interest are disclosed by the other authors.
Ethical approval
The study was approved by The University of Texas MD Anderson Cancer Center's Institutional Review Board (PROSPECT—LAB07-0233).
Human and animal rights
All human studies were conducted in accordance with the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mitchell, K.G., Amini, B., Wang, Y. et al. 18F-fluorodeoxyglucose positron emission tomography correlates with tumor immunometabolic phenotypes in resected lung cancer. Cancer Immunol Immunother 69, 1519–1534 (2020). https://doi.org/10.1007/s00262-020-02560-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-020-02560-5