Abstract
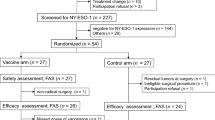
Cholesteryl pullulan (CHP) is a novel antigen delivery system. CHP and New York esophageal squamous cell carcinoma 1 (NY-ESO-1) antigen complexes (CHP-NY-ESO-1) present multiple epitope peptides to the MHC class I and II pathways. Adjuvants are essential for cancer vaccines. MIS416 is a non-toxic microparticle that activates immunity via the nucleotide-binding oligomerization domain 2 (NOD2) and TLR9 pathways. However, no reports have explored MIS416 as a cancer vaccine adjuvant. We conducted a first-in-human clinical trial of CHP-NY-ESO-1 with MIS416 in patients with NY-ESO-1-expressing refractory solid tumors. CHP-NY-ESO-1/MIS416 (μg/μg) was administered at 100/200, 200/200, 200/400 or 200/600 (cohorts 1, 2, 3 and 4, respectively) every 2 weeks for a total of 6 doses (treatment phase) followed by one vaccination every 4 weeks until disease progression or unacceptable toxicity (maintenance phase). The primary endpoints were safety and tolerability, and the secondary endpoint was the immune response. In total, 26 patients were enrolled. Seven patients (38%) continued vaccination in the maintenance phase. Grade 3 drug-related adverse events (AEs) were observed in six patients (23%): anorexia and hypertension were observed in one and five patients, respectively. No grade 4–5 drug-related AEs were observed. Eight patients (31%) had stable disease (SD). Neither augmentation of the NY-ESO-1-specific IFN-γ-secreting CD8+ T cell response nor an increase in the level of anti-NY-ESO-1 IgG1 was observed as the dose of MIS416 was increased. In a preclinical study, adding anti-PD-1 monoclonal antibody to CHP-NY-ESO-1 and MIS416 induced significant tumor suppression. This combination therapy is a promising next step.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peptide cancer vaccines have been evaluated in previous studies, but they have thus far exhibited limited efficacy against advanced cancers. Adjuvant selection is an important factor that affects the success of cancer vaccines. For example, substances that are retained at the injection site should be avoided as cancer vaccine adjuvants. Hailemichael et al. [1] reported that incomplete Freund’s adjuvant-based vaccination caused T cells to accumulate at the vaccination site rather than at the tumor site and induced T cell apoptosis. Stimulants of pathogen recognition receptors, including TLRs and nucleotide-binding oligomerization domain (NOD)-like receptors, could activate antigen-presenting cells and may thereby overcome the immunosuppressive tumor microenvironment. TLR stimulants, such as OK-432, CpG or poly-ICLC, have been evaluated in conjunction with the New York esophageal squamous cell carcinoma 1 (NY-ESO-1) antigen-related cancer vaccine in clinical studies [2,3,4,5,6,7,8]. One of the most promising agents is a stimulant of TLR9. Muraoka et al. [9] reported that immunization with a peptide vaccine without an adjuvant increased apoptosis in vaccine-induced CD8+ T cells; in contrast, immunization with a peptide vaccine with a TLR9 stimulant reduced apoptosis in vaccine-induced CD8+ T cells and induced a significant anti-tumor effect in a mouse model. The stimulation of multiple innate immunity signaling pathways may greatly improve the efficacy of cancer vaccines over that achieved by TLR9 signaling alone.
MIS416 is a nontoxic microparticle adjuvant derived from Propionibacterium acnes that activates the immune response via the NOD2 and TLR9 pathways. MIS416 acts as a Th1 response-skewing adjuvant by promoting the CD8+ T cell response and enhancing the anti-tumor activity of vaccines in a mouse model [10]. However, no clinical trials of cancer vaccines with MIS416 as an adjuvant have been reported. The NY-ESO-1 antigen, a cancer-testis antigen, was identified in esophageal cancer by serological expression cloning (SEREX) performed using serum obtained from patients with autologous esophageal squamous cell carcinoma [11, 12]. The NY-ESO-1 antigen is expressed in a variety of cancers; for example, the NY-ESO-1 antigen is expressed in approximately 40% of refractory urothelial cancers [13,14,15], approximately 15–40% of advanced prostate cancers [16, 17] and 49–75% of synovial cell sarcomas [18, 19] but is not expressed in normal tissues with the exception of the testis and placenta. These findings suggest that the NY-ESO-1 antigen could be an ideal target for cancer immunotherapy against many malignant tumors and may have high cancer specificity and low toxicity. Cholesteryl pullulan (CHP) is a polysaccharide-based novel antigen delivery system for cancer vaccines. A complex of CHP and the NY-ESO-1 antigen (CHP-NY-ESO-1) was constructed that contains multiple MHC class I- and II-restricted epitopes and efficiently induces antigen-specific CD4+ and CD8+ T cell immunity [20,21,22,23,24,25]. We conducted single-center, open-label, dose-escalation studies of CHP-NY-ESO-1 with MIS416 as an adjuvant in patients with NY-ESO-1-expressing refractory urothelial cancer or castration-resistant prostate cancer and malignant solid tumors to evaluate its safety, tolerability, and immune response [26, 27].
Materials and methods
Mice, cell lines and anti-mouse PD-1 monoclonal antibodies
Female BALB/c mice aged 6–10 weeks were used. A mouse colon tumor cell line CT26 was transfected with human NY-ESO-1 [9, 28]. Tumor volume was calculated as follows: 0.5 × length (mm) × width (mm)2. An anti-mouse PD-1 (clone RMP1-14) monoclonal antibody (mAb) was produced in-house from hybridoma and purified as monoclonal [29].
Patients and treatment
Patients meeting the following criteria were included: histologically documented urothelial cancer, prostate cancer (clinical trial Registration Number UMIN000005246) or malignant solid tumors (UMIN000008006) that were refractory to standard therapy, age ≥ 20 years, an Eastern Cooperative Oncology Group (ECOG) performance status (PS) scale of 0–2, a life expectancy ≥ 3 months, adequate organ function and positive tumor expression of NY-ESO-1. Patients with a history of active autoimmune disease, the use of steroids (more than 20 mg equivalent of prednisolone/day), the use of immunosuppressive drugs, uncontrolled infections or previous NY-ESO-1-related immunotherapy were excluded.
Patients were enrolled from March 2011 to February 2017 and received CHP-NY-ESO-1 (0.5 mg/mL)/MIS416 (2 mg/mL) administered at 100 μg/200 μg, 200 μg/200 μg, 200 μg/400 μg or 200 μg/600 μg (cohorts 1, 2, 3 and 4, respectively) every 2 weeks for a total of 6 doses during the treatment phase (clinical trial registration number UMIN000005246 and UMIN000008006) followed by vaccination every 4 weeks (maintenance phase) until disease progression, patient refusal or unacceptable toxicity (UMIN000008007). CHP-NY-ESO-1 and MIS416 were manufactured according to good manufacturing practices and provided by ImmunoFrontier, Inc. (Tokyo, Japan) and Innate Therapeutics Ltd., respectively. CHP-NY-ESO-1 was subcutaneously (s.c.) injected into the chest, abdomen, upper arm or lower leg. MIS416 was injected s.c. at a site 2 cm away from the periphery of the CHP-NY-ESO-1 injection bulge. Mixing the 2 drugs under the skin was prohibited. The primary endpoints were safety and tolerability, and the secondary endpoints were immune response and quality of life (QOL). The dose-limiting toxicity (DLT) was defined as grade 3 or higher for injection site reaction, allergic reaction, pruritus, chills, and fever. The maximum tolerated dose (MTD) was the highest dose that caused DLT in no more than one of 6 patients. Patients assessable for dose escalation were those who were treated with more than 4 courses. If the number of assessable patients was lower than three, patients were added to the cohort. In cohort 4, 2 of the 4 patients had a total of 3 severe adverse events (SAEs), including 1 treatment-related case of anorexia, 1 nervous system disorder caused by cancer progression and 1 case of pancreatitis caused by alcohol intake. The data and safety committee recommended stopping further patient enrollment in cohort 4 because of the high frequency of SAEs. We decided to terminate the clinical trial considering the long amount of time required for patient enrollment and because no further improvements in efficacy were expected.
Assessment
Treatment response was assessed at 12 weeks by computed tomography. Patients with prostate cancer were also assessed by bone scans and the detection of serum PSA levels. Responses were assessed according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria version 1.1 [30]. AEs were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Serial serum and PBMC samples were collected before and during treatment.
QOL was assessed using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 Japanese version 3.0 every 4 weeks as follows: at baseline and on treatment phase course 3 day 1, treatment phase course 5 day 1, and treatment phase course 6 day 15 (clinical trial registration number UMIN000005246). The EORTC QLQ-C30 is a questionnaire that was developed to assess the QOL of cancer patients. The QLQ-C30 contains 5 functional scales (physical, role, cognitive, emotional, and social), 3 symptom scales (fatigue, pain, and nausea and vomiting), and a global health and QOL scale [31].
Expression of the NY-ESO-1 antigen
Archival or newly obtained tumor samples obtained from patients were screened for NY-ESO-1 expression. Eligible patients were those with NY-ESO-1 expression in ≥ 1% of tumor cells according to immunohistochemical staining with an E978 monoclonal antibody or ≥ 1 copy NY-ESO-1/104 copies of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) according to a quantitative real-time PCR (qRT-PCR) analysis.
T cell response, NY-ESO-1-specific antibody response and cytokine kinetics
Serum samples were obtained at baseline, 6 h and 1 week after the 1st vaccination, and 2 weeks after each vaccination. PBMCs were obtained at baseline, before the 4th vaccination and 2 weeks after the 6th vaccination. All samples were stored at − 80 °C until analyzed.
The T cell response was assessed by ELISPOT assay as previously described [32]. In brief, ELISPOT plates (MAHA S4510; Millipore) were coated with an anti-human interferon (IFN)-γ monoclonal antibody (R&D Systems, Minneapolis, MN). A total of 5 × 104 sensitized CD4+ or CD8+ T cells and 1 × 105 peptide-pulsed irradiated CD4− CD8− PBMCs were placed in each well of the ELISPOT plate. NY-ESO-1-overlapping peptides were grouped as follows: anterior half-mix p1–20, p11–30, p21–40, p31–50, p41–60, p51–70, p61–80, p71–90 and p81–100 and posterior half-mix p91–110, p101–120, p111–130, p119–141, p131–150, p139–160, p151–170 and p161–180. After the mixtures were incubated for 22 h at 37 °C, the plate was washed, the biotinylated capture antibody was added, and the combined mixture was incubated overnight at 4 °C. After the cells were washed, they were reacted with streptavidin–alkaline phosphatase conjugate and then stained using an alkaline phosphatase conjugate substrate kit (BioRad, Hercules, CA). The spots were counted using an ELISPOT Plate Reader (ImmunoSpot, CTL-Europe GmbH, Bonn, Germany).
The NY-ESO-1-specific antibody response was assessed by ELISA as previously described [24, 25]. Briefly, recombinant NY-ESO-1 proteins (His-tag and GST-tag) were absorbed onto immunoplates (442,404; Nunc, Roskilde, Denmark) at a concentration of 10 ng/50 μL/well at 4 °C. The collected serum samples were diluted from 1:400 to 1:6400. After washing and blocking the plate, the sera were added and incubated for 10 h. After washing, goat anti-human IgG (H + L chain) (MBL, Nagoya, Japan) conjugated with peroxidase was added. After adding the TMB substrate (Pierce, Rockford, IL), the plate was read using a Microplate Reader (model 550; BioRad, Hercules, CA). Serum samples were obtained from 83 healthy volunteers and assayed by ELISA for the NY-ESO-1 IgG antibody as described in another study performed at Mie University (Mie University approval number: 817) before the start of this clinical study using CHP-NY-ESO-1 and MIS416. The cutoff level selected for the anti-NY-ESO-1 IgG antibody was defined as the mean optical density (OD) 450–550 absorption value + 1.645 × the standard deviation as 0.254. Hence, an OD 450 absorption value of at least 0.254 was considered a positive reaction at a serum dilution of 1:400. For patients who were antibody-positive at the baseline, their antibody titers were judged to be “augmented” if they changed by fourfold or more compared with the baseline. The IgG subclass antibody response to the NY-ESO-1 protein was detected with ELISA using polyclonal sheep anti‑human IgG1 (dilution, 1:25,600; cat. no. AP006), IgG2 (dilution, 12,800; cat. no. AP007) and IgG3 (dilution, 1:12,800; Cat. No. AP008) (H + L chain) conjugated with HRP (The Binding Site Group Ltd., Birmingham, UK) used as the secondary antibodies.
The serum levels of 48 cytokines and chemokines were determined using Bio-Plex kits (Bio-Rad, Hercules, CA) according to the manufacturer's instructions. The kits’ analytes were IL-1α, IL-1β, IL-1Ra, IL-2, IL-2Rα, IL-3, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-12 (p40), IL-12 (p70), IL-13, IL-15, IL-16, IL-17, IL-18, eotaxin, basic fibroblast growth factor (bFGF), G-CSF, GM-CSF, IFN-γ, C–C motif chemokine ligand 2 (CCL2), CCL3, CCL4, CCL5, platelet-derived growth factor (PDGF)-BB, cutaneous T-cell-attracting chemokine (CTACK), growth-related oncogene (GRO)-α, hepatocyte growth factor (HGF), IFNα2, leukemia inhibitory factor (LIF), CCL7, macrophage colony-stimulating factor (M-CSF), macrophage migration inhibitory factor (MIF), C–X–C motif chemokine ligand 9 (CXCL9), CXCL10, β-nerve growth factor (NGF), stem cell factor (SCF), stem cell growth factor (SCGF)-β, stromal cell-derived factor (SDF)-1α, TNF-α, TNF-β, TRAIL and VEGF [33].
Statistical analysis
The combined data analyses of the two treatment phase trials are described in the protocol. The Mann–Whitney U test was used to compare data obtained in the two groups. Fisher's exact test was used to compare the IgG positivity rates of patients who received CHP-NY-ESO-1 at 100 µg versus those who received CHP-NY-ESO-1 at 200 µg. Kruskal–Wallis ANOVA was used to compare data obtained in more than three groups. Student's t test was used to assess changes in QLQ-C30 scores between the pretreatment and treatment phases. P-values below 0.05 were considered statistically significant. Calculations were performed with SPSS Statistics version 25 (IBM Japan, Ltd., Tokyo, Japan).
Results
Patient characteristics and treatment exposure
In total, 26 patients were enrolled (13 with prostate cancer, 5 with urothelial cancer, 4 with synovial sarcoma and 4 with other cancers, as shown in Table 1 and Supplementary Table 1). The median age was 70 years old (range 36–84). All patients had received prior therapies (chemotherapy, radiation, and/or surgery). Eight patients, all of whom were all prostate cancer patients, received systemic dexamethasone (DEX) (Supplementary Table 2). Nine patients were enrolled in cohort 1, 7 in cohort 2, 6 in cohort 3 and 4 in cohort 4. The median number of vaccinations was 6 (range 1–66). Seven patients (38%) moved to the maintenance phase and received ≥ 7 doses of the vaccine.
Drug-related adverse events
The drug-related AEs reported in this study are shown in Table 2. Grade 1–2 injection site reactions were observed in all patients. Grade 3 drug-related AEs were observed in 6 patients (23%): 5 exhibiting hypertension and 1 presented with anorexia. There was 1 case of grade 3 hypertension (11.1%) in cohort 1, 2 (28.6%) in cohort 2, 1 (16.7%) in cohort 3, and 1 (25.0%) in cohort 4 (Supplementary Table 3). The patients with these AEs were all prostate cancer patients and had grade 2 hypertension at baseline. One patient required an increase in the dose of antihypertensive medication, and the other AEs were resolved without medical modification. No grade 4–5 drug-related AEs were observed.
Responses
Eight patients (31%) had stable disease (SD) (Table 3). Among the 13 patients with prostate cancer, 5 had SD (38%), 7 had PD (54%) and 1 was N/A (7%) (Supplementary Table 2). Among these patients, 4 advanced to the maintenance phase. One patient with prostate cancer who was enrolled in cohort 2 received 60 vaccinations during the maintenance phase. He showed no disease progression or significant increase in the serum PSA levels over 5 years.
Serial titers of anti-NY-ESO-1 IgG
An antibody response was observed in 5 of 9 patients (56%) in cohort 1 (CHP-NY-ESO-1 at 100 µg) and 16 of 17 patients (94%) in cohorts 2–4 (CHP-NY-ESO-1 at 200 µg) (p = 0.040) (Table 3, Fig. 1). Among the patients who received more than 3 vaccinations, an antibody response was observed in 4 of 7 patients (57%) in cohort 1 and in 16 of 16 patients (100%) in cohorts 2–4.
NY-ESO-1-specific IgG response. Anti-NY-ESO-1 IgG was assayed by ELISA at serum dilutions of 1:400 (blue line), 1:1,600 (orange line), 1:6,400 (yellow line) and 1:25,600 (green line). Serum was collected at baseline, course 1 day 8 (C1D8), course 2 day 1 (C2D1), course 3 day 1 (C3D1), course 4 day 1 (C4D1), course 5 day 1 (C5D1), course 6 day 1 (C6D1) and course 6 day 15 (C6D15). The cutoff for OD 450 absorption was 0.254 (red dotted line)
Cytokine analysis
We hypothesized that the MIS416 adjuvant affected serum cytokine levels in the early phase. The changes in serum cytokine/chemokine levels that occurred from baseline to 6 h after the 1st vaccination were determined using a multiplex assay. Sixteen patients’ samples were assessable. To exclude an effect of NY-ESO-1 dose, we assessed samples from patients enrolled in cohorts 2–4. Compared with baseline values, the levels of IL-6, IL-9, IL-10, GM-CSF, PDGF-BB, β-NGF, SCF and SCGF-β were significantly higher at 6 h after the first vaccination (Fig. 2). In contrast, no cytokines significantly decreased. With regard for the MIS dose, a comparison of cohorts 2, 3 and 4 revealed that the level of IL-17 tended to increase as the MIS416 dose increased (Supplementary Figure 1).
Cytokine analyses. Serum cytokine changes from baseline to 6 h after the first vaccination was assessed. To exclude an effect of the NY-ESO-1 dose, we assessed samples from patients enrolled in cohorts 2–4 (CHP-NY-ESO-1 200 µg with MIS416 200–600 µg). Only those cytokines for which levels significantly changed are shown. The following cytokines had levels that significantly changed from baseline to 6 h after the 1st vaccination: IL-6 (p = 0.033), IL-9 (p = 0.048), IL-10 (p = 0.018), GM-CSF (p = 0.020), PDGF-BB (p = 0.049), β-NGF (p = 0.005), SCF (p = 0.003) and SCGF-β (p = 0.003)
T cell response
Patients whose PBMCs were available for assessing T cell responses are listed in Table 3. The T cell response was assessed in two patients per cohort, for a total of 8 patients. No increase in NY-ESO-1-specific IFN-γ secreting CD8+ T cells was detected after vaccination. In contrast, the number of NY-ESO-1-specific IFN-γ-secreting CD4+ T cells increased in 2 patients after vaccination. One of these 2 patients, Pt ID UR-008, did not show progression for 5 years, as mentioned above, but did exhibit a NY-ESO-1-specific CD4+ T cell response (Table 3 and Supplementary Fig. 2a).
Quality of life
In total, 11 patients were assessed for QOL. There was no significant difference in any score, including the 5 functional scales, 3 symptom scales, and global health and QOL scale, during treatment (Supplementary Fig. 3).
Preclinical study of CHP-NY-ESO-1 + MIS416 with a PD-1 inhibitor
To determine whether CHP-NY-ESO-1 exerts anti-tumor activity in an animal model, we assessed vaccine efficacy by adding an anti-PD-1 monoclonal antibody (mAb) to the CHP-NY-ESO-1 + MIS416 group. Treatment with CHP-NY-ESO-1, anti-PD-1 mAb, CHP-NY-ESO-1 + anti-PD-1 mAb or CHP-NY-ESO-1 + MIS416 could not suppress tumor growth, whereas treatment with CHP-NY-ESO-1 + MIS416 + anti-PD-1 mAb induced significant tumor growth suppression (Fig. 3).
Addition of the PD-1 inhibitor to CHP-NY-ESO-1 + MIS416 in the NY-ESO-1-transfected tumor–bearing mouse model. BALB/c mice subcutaneously inoculated with 1 × 106 human NY-ESO-1-transfected murine colon tumor cell line CT26 cells were treated with CHP-NY-ESO-1 alone, anti-PD-1 mAb (clone RMP1-14) alone, CHP-NY-ESO-1 + MIS416, CHP-NY-ESO-1 + anti-PD-1 mAb, or CHP-NY-ESO-1 + MIS416 + anti-PD-1 mAb (n = 4 per group). CHP-NY-ESO-1 (40 μg/mouse) and MIS416 (250 μg/mouse) were administered subcutaneously on days 1 and 7. The anti-PD-1 monoclonal antibody (clone RMP1-14, 150 μg/mouse) was administered intraperitoneally on days 1, 4, 7, 9, 13, 16 and 19. Compared with the no-treatment group, only the CHP-NY-ESO-1 + MIS416 + anti-PD-1 mAb group showed significant tumor growth suppression (p = 0.029)
Discussion
CHP-NY-ESO-1 is a safe and promising cancer vaccine [21,22,23,24,25]. We expected the addition of MIS416 to make CHP-NY-ESO-1 more efficient without compromising safety. In this study, CHP-NY-ESO-1 with adjuvant MIS416 200–400 μg showed acceptable safety and tolerability. Grade 3 hypertension was observed in five patients (19%). In multiple sclerosis (MS) patients who were administered MIS416 intravenously, vascular disorders, including hypertension, were observed in 52.5% of the patients [34]. In the higher MIS416 dose group (500–600 μg), the frequency of vascular disorders was 83.3%; these included diastolic hypertension in 50.0%, hypertension in 50.0%, and systolic hypertension in 66.7% of the patients. These results indicate that MIS416 may cause vascular AEs. The exact mechanism has not yet been clarified. In our study, among the 5 patients with grade 3 hypertension, 4 had prostate cancer. A previous meta-analysis showed that there was a relationship between hypertension and the risk of prostate cancer [35]. Because some cytokines can elevate blood pressure [36], prostate cancer patients with hypertension at baseline might be more sensitive to MIS416-induced cytokines. In line with the results of a previous study [25], we found that the antibody response was stronger in patients who received CHP-NY-ESO-1 200 µg than in those who received CHP-NY-ESO-1 100 µg (Table 3). The antibody response rate and cycle number in the seropositive group were similar between the report by Kageyama et al. (53.8% and a median of 2 cycles in the CHP-NY-ESO-1 100 μg group; and 100% and a median of 2 cycles in the CHP-NY-ESO-1 200 μg group, respectively) and our study (56% and a median of 3 cycles in the CHP-NY-ESO-1 100 μg + MIS416 200 μg group; and 94% and a median of 2 cycles in the CHP-NY-ESO-1 200 μg + MIS416 200–600 μg group). The IgG subtype was also considered in our study. Karbach et al. reported that when CpG was added to the NY-ESO-1 vaccine, IgG1 and IgG3 responses were induced [5]. To clarify the effect of MIS416, we compared the titers of IgG1, IgG2 and IgG3 in serum obtained from patients in cohorts 2–4 (CHP-NY-ESO-1 200 µg with MIS416) to those reported in 8 patients enrolled in a previous study by Kageyama et al. of CHP-NY-ESO-1 200 µg without an adjuvant [25]. One patient in cohort 3 of our study was vaccinated twice and had negative seroconversion, and this patient was excluded from the IgG analysis. CHP-NY-ESO-1 induced a prominent IgG1 response with increased IgG2 and IgG3 titers. However, adding MIS416 seemed to suppress IgG1, 2 and 3 responses (Supplementary Fig. 4a). While some patients did use steroids, NY-ESO-1-specific IgG1 titers were not affected by steroid use in cohorts 2–4 (Supplementary Fig. 4c). The patients’ QOL was well-maintained during vaccination with CHP-NY-ESO-1 with MIS416 (200 and 400 µg) (Supplementary Fig. 3). However, CHP-NY-ESO-1 vaccination with 600 μg MIS416 was not well-tolerated, and tumor shrinkage was not observed in this group. Furthermore, the immune response stimulated by CHP-NY-ESO-1 was not enhanced by increasing the dose of MIS416.
MIS416 skewed the Th1 response in a mouse model [10]. In vitro, MIS416 was readily internalized by human myeloid and plasmacytoid DCs, resulting in cytokine secretion and cell activation/maturation. In this study, the subcutaneous injection of MIS416 caused IL-6 and IL-10 levels to be increased at 6 h after the first vaccination (Fig. 2). CHP-NY-ESO-1 vaccination showed CD4+ and CD8+ T cell responses in previous studies [22,23,24]. Unfortunately, in this study, we did not find that CD4+ Th1 cell and CD8+ T cell responses were enhanced. As mentioned above, we compared serum IgG1, IgG2 and IgG3 titers between samples obtained from patients in cohorts 2–4 (CHP-NY-ESO-1 200 μg with MIS416) and those obtained from 8 patients enrolled in a previous study by Kageyama et al. in which the patients received CHP-NY-ESO-1 200 μg without an adjuvant [25]. The anti-NY-ESO-1 IgG1 response was also attenuated as the dose of MIS416 increased (Supplementary Fig. 4b). The NY-ESO-1-specific IgG1 titer was significantly lower in patients who received MIS416 600 μg than in those who received the vaccine without MIS416. Two main causes might lead to these unexpected results. One cause is species-specific differences [37]. Although MIS416 suppressed IL-17 in an MS mouse model [38], this result has not been confirmed in humans with MS [34]. In our study, IL-17 levels tended to increase as the dose of MIS416 increased (Supplementary Fig. 1). When the effects of different CHP-NY-ESO-1 doses were compared, no significant change in the serum cytokine levels was observed with the exception of IL-13 (Supplementary Fig. 5). Based on the findings in a mouse model, we could not predict whether the human innate immune system would be activated by the TLR9 and NOD2 signals included in MIS416, leading to an adaptive immune response. Another cause is the paradoxical effect of MIS416. IL-10 generally acts as an immunosuppressive cytokine but can enhance the CD8+ T cell response at higher doses [39, 40]. Although IL-10 levels were increased in this study (Fig. 2), the change in absolute concentration was small (median + 1.3 pg/mL, Supplementary Table 4). In vitro, MIS416 stimulated PBMCs, causing them to secrete IL-6, IL-10, IFN-γ, TNF-α and IL-1β and exhibit an inverse dose–response to MIS416 at 5, 20 and 50 µg/mL [41]. In an MS mouse model, a high dose of MIS416 (100 µg/mouse) resulted in the systemic suppression of pro-inflammatory cytokine levels [38]. In addition, in humans, in a clinical trial in which a TLR9 stimulant was applied, the higher dose group had a lower response rate than was observed in the lower dose group (≤ 2 mg 80%, 8 mg 38%) [42]. These findings suggest that TLR stimulation may suppress the innate response in a dose-dependent manner. However, it is not possible to directly compare data obtained using MIS416 preclinical and human studies since the route of administration was different between the present and previous studies, and this is an important factor. In a previous study of MS patients, MIS416 was administered intravenously with the expectation that it would move to the liver and act as an immunosuppressive agent; in contrast, in this study, MIS416 was administered subcutaneously with the expectation that it would exert an immune stimulatory effect in a draining lymph node [10].
There are several limitations of this study. First, there are a variety of cancer types, and we cannot exclude differences in prior systemic therapy and immunogenicity in different cancers. Second, the effect of steroids cannot be ruled out as steroid use is an important issue in cancer immunotherapy. For example, in patients with prostate cancer, steroids may elicit anti-prostate cancer effects. Combined systemic therapy with steroids is commonly administered to patients with prostate cancer refractory to castration [43,44,45,46]. In this study, steroid use (≤ 20 mg equivalent of prednisolone/day) was allowed. Eight patients (31%) used DEX, with 1 mg/day used by 3 patients and ≤ 0.5 mg/day used by 5 patients. All 8 patients were prostate cancer patients who received DEX at enrollment and throughout this study. Among these 8 patients, 38% achieved SD. In the cytokine analysis, steroid use was found to suppress changes in serum G-CSF and CCL2 levels (Supplementary Fig. 6). However, the measured values showed no significant differences. Steroid use also did not affect NY-ESO-1-specific IgG1 titers (Supplementary Fig. 4c). Interestingly, one of the 8 patients who were enrolled in cohort 2 experienced no progression for 5 years and showed a NY-ESO-1-specific CD4+ T cell response. Cancer vaccines are known to be effective in prostate cancer, as shown in studies using Sipuleucel-T [47, 48]. Yoshimura et al. [49] reported that patients who received a peptide vaccine plus DEX had longer PSA progression-free survival than was observed in patients who received DEX alone. Although we cannot deny that immune suppression was induced by steroids, these findings suggest that the induction of the NY-ESO-1-specific T cell response shows promising effects for prostate cancer patients, even among patients undergoing low-dose systemic steroid treatment.
It has been assumed that the appropriate clinical use of an immune-stimulating adjuvant enhances the anti-tumor effects of cancer vaccines. Based on this idea, a number of cancer vaccine clinical trials have been conducted worldwide; however, almost all of them have produced disappointing results. Melanoma-associated antigen (MAGE)-A3, a cancer-testis antigen, is one of the most promising targets for cancer vaccines [50]. Recombinant MAGE-A3 vaccination with the AS15 immunostimulant, which contains CpG, a TLR9 stimulant, was assessed in patients with melanoma and non-small cell lung cancer but did not produce a survival benefit [51, 52]. This finding suggests that cancer vaccines cannot be developed as monotherapies. In our study, no complete or partial response was observed. The combination of CHP-NY-ESO-1 + MIS416 + anti-PD-1 mAb exerted a significant tumor growth suppression effect in the mouse model (Fig. 3). The addition of anti-PD-1 mAb activates not only NY-ESO-1-specific T cells but also other tumor antigen-reactive T cells. A combination therapy that includes a cancer vaccine with the proper adjuvant and an immune checkpoint inhibitor may confer clinical anti-tumor effects.
In conclusion, CHP-NY-ESO-1 with MIS416 200–400 µg was safe and tolerable but did not induce adequate immune or clinical responses. As a next step, we plan to conduct a clinical trial of a combination therapy that includes a cancer vaccine, an adjuvant and an immune checkpoint inhibitor.
Abbreviations
- ALT:
-
Alanine aminotransferase
- bFGF:
-
Basic fibroblast growth factor
- CCL:
-
C–C motif chemokine ligand
- CHP:
-
Cholesteryl pullulan
- CRPC:
-
Castration-resistant prostate cancer
- CTACK:
-
Cutaneous T-cell-attracting chemokine
- CXCL:
-
C–X–C motif chemokine ligand
- DEX:
-
Dexamethasone
- DLT:
-
Dose-limiting toxicity
- ECOG:
-
Eastern Cooperative Oncology Group
- EORTC:
-
European organization for research and treatment of cancer
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GRO:
-
Growth-related oncogene
- HGF:
-
Hepatocyte growth factor
- LIF:
-
Leukemia inhibitory factor
- MAGE:
-
Melanoma-associated antigen
- M-CSF:
-
Macrophage colony-stimulating factor
- MIF:
-
Macrophage migration inhibitory factor
- MS:
-
Multiple sclerosis
- MTD:
-
Maximum tolerated dose
- NGF:
-
Nerve growth factor
- NOD:
-
Nucleotide-binding oligomerization domain
- NY-ESO-1:
-
New York esophageal squamous cell carcinoma 1
- PD:
-
Progressive disease
- PDGF:
-
Platelet-derived growth factor
- PS:
-
Performance status
- QOL:
-
Quality of life
- qRT-PCR:
-
Quantitative real-time PCR
- RECIST:
-
Response evaluation criteria in solid tumors
- SAE:
-
Severe adverse event
- s.c.:
-
Subcutaneously
- SCF:
-
Stem cell factor
- SCGF:
-
Stem cell growth factor
- SD:
-
Stable disease
- SDF:
-
Stromal cell-derived factor
- SEREX:
-
Serological expression cloning
- UC:
-
Urothelial cancer
References
Hailemichael Y, Dai Z, Jaffarzad N, Ye Y, Medina MA, Huang XF, Dorta-Estremera SM, Greeley NR, Nitti G, Peng W, Liu C, Lou Y, Wang Z, Ma W, Rabinovich B, Sowell RT, Schluns KS, Davis RE, Hwu P, Overwijk WW (2013) Persistent antigen at vaccination sites induces tumor-specific CD8(+) T cell sequestration, dysfunction and deletion. Nat Med 19(4):465–472. https://doi.org/10.1038/nm.3105
Adams S, O'Neill DW, Nonaka D, Hardin E, Chiriboga L, Siu K, Cruz CM, Angiulli A, Angiulli F, Ritter E, Holman RM, Shapiro RL, Berman RS, Berner N, Shao Y, Manches O, Pan L, Venhaus RR, Hoffman EW, Jungbluth A, Gnjatic S, Old L, Pavlick AC, Bhardwaj N (2008) Immunization of malignant melanoma patients with full-length NY-ESO-1 protein using TLR7 agonist imiquimod as vaccine adjuvant. J Immunol 181(1):776–784
Aoki M, Ueda S, Nishikawa H, Kitano S, Hirayama M, Ikeda H, Toyoda H, Tanaka K, Kanai M, Takabayashi A, Imai H, Shiraishi T, Sato E, Wada H, Nakayama E, Takei Y, Katayama N, Shiku H, Kageyama S (2009) Antibody responses against NY-ESO-1 and HER2 antigens in patients vaccinated with combinations of cholesteryl pullulan (CHP)-NY-ESO-1 and CHP-HER2 with OK-432. Vaccine 27(49):6854–6861. https://doi.org/10.1016/j.vaccine.2009.09.018
Kakimi K, Isobe M, Uenaka A, Wada H, Sato E, Doki Y, Nakajima J, Seto Y, Yamatsuji T, Naomoto Y, Shiraishi K, Takigawa N, Kiura K, Tsuji K, Iwatsuki K, Oka M, Pan L, Hoffman EW, Old LJ, Nakayama E (2011) A phase I study of vaccination with NY-ESO-1f peptide mixed with Picibanil OK-432 and Montanide ISA-51 in patients with cancers expressing the NY-ESO-1 antigen. Int J Cancer 129(12):2836–2846. https://doi.org/10.1002/ijc.25955
Karbach J, Neumann A, Atmaca A, Wahle C, Brand K, von Boehmer L, Knuth A, Bender A, Ritter G, Old LJ, Jager E (2011) Efficient in vivo priming by vaccination with recombinant NY-ESO-1 protein and CpG in antigen naive prostate cancer patients. Clin Cancer Res 17(4):861–870. https://doi.org/10.1158/1078-0432.ccr-10-1811
Wada H, Isobe M, Kakimi K, Mizote Y, Eikawa S, Sato E, Takigawa N, Kiura K, Tsuji K, Iwatsuki K, Yamasaki M, Miyata H, Matsushita H, Udono H, Seto Y, Yamada K, Nishikawa H, Pan L, Venhaus R, Oka M, Doki Y, Nakayama E (2014) Vaccination with NY-ESO-1 overlapping peptides mixed with Picibanil OK-432 and montanide ISA-51 in patients with cancers expressing the NY-ESO-1 antigen. J Immunotherap (Hagerstown, MD 1997) 37(2):84–92. doi: 10.1097/CJI.0000000000000017
Chen JL, Dawoodji A, Tarlton A, Gnjatic S, Tajar A, Karydis I, Browning J, Pratap S, Verfaille C, Venhaus RR, Pan L, Altman DG, Cebon JS, Old LL, Nathan P, Ottensmeier C, Middleton M, Cerundolo V (2015) NY-ESO-1 specific antibody and cellular responses in melanoma patients primed with NY-ESO-1 protein in ISCOMATRIX and boosted with recombinant NY-ESO-1 fowlpox virus. Int J Cancer 136(6):E590–E601. https://doi.org/10.1002/ijc.29118
Takeoka T, Nagase H, Kurose K, Ohue Y, Yamasaki M, Takiguchi S, Sato E, Isobe M, Kanazawa T, Matsumoto M, Iwahori K, Kawashima A, Morimoto-Okazawa A, Nishikawa H, Oka M, Pan L, Venhaus R, Nakayama E, Mori M, Doki Y, Wada H (2017) NY-ESO-1 protein cancer vaccine with poly-ICLC and OK-432: rapid and strong induction of NY-ESO-1-specific immune responses by poly-ICLC. J Immunotherap (Hagerstown, MD 1997) 40(4):140–147(148). doi:10.1097/cji.0000000000000162
Muraoka D, Kato T, Wang L, Maeda Y, Noguchi T, Harada N, Takeda K, Yagita H, Guillaume P, Luescher I, Old LJ, Shiku H, Nishikawa H (2010) Peptide vaccine induces enhanced tumor growth associated with apoptosis induction in CD8+ T cells. J Immunol 185(6):3768–3776. https://doi.org/10.4049/jimmunol.0903649
Girvan RC, Knight DA, O'Loughlin CJ, Hayman CM, Hermans IF, Webster GA (2011) MIS416, a non-toxic microparticle adjuvant derived from Propionibacterium acnes comprising immunostimulatory muramyl dipeptide and bacterial DNA promotes cross-priming and Th1 immunity. Vaccine 29(3):545–557. https://doi.org/10.1016/j.vaccine.2010.10.040
Chen YT, Boyer AD, Viars CS, Tsang S, Old LJ, Arden KC (1997) Genomic cloning and localization of CTAG, a gene encoding an autoimmunogenic cancer-testis antigen NY-ESO-1, to human chromosome Xq28. Cytogenet Cell Genet 79(3–4):237–240. https://doi.org/10.1159/000134734
Gnjatic S, Nishikawa H, Jungbluth AA, Gure AO, Ritter G, Jager E, Knuth A, Chen YT, Old LJ (2006) NY-ESO-1: review of an immunogenic tumor antigen. Adv Cancer Res 95:1–30. https://doi.org/10.1016/S0065-230X(06)95001-5
Kurashige T, Noguchi Y, Saika T, Ono T, Nagata Y, Jungbluth A, Ritter G, Chen YT, Stockert E, Tsushima T, Kumon H, Old LJ, Nakayama E (2001) NY-ESO-1 expression and immunogenicity associated with transitional cell carcinoma: correlation with tumor grade. Cancer Res 61(12):4671–4674
Dyrskjot L, Zieger K, Kissow Lildal T, Reinert T, Gruselle O, Coche T, Borre M, Orntoft TF (2012) Expression of MAGE-A3, NY-ESO-1, LAGE-1 and PRAME in urothelial carcinoma. Br J Cancer 107(1):116–122. https://doi.org/10.1038/bjc.2012.215
Yin B, Liu G, Wang XS, Zhang H, Song YS, Wu B (2012) Expression profile of cancer-testis genes in transitional cell carcinoma of the bladder. Urol Oncol 30(6):886–892. https://doi.org/10.1016/j.urolonc.2010.08.017
Nakada T, Noguchi Y, Satoh S, Ono T, Saika T, Kurashige T, Gnjatic S, Ritter G, Chen YT, Stockert E, Nasu Y, Tsushima T, Kumon H, Old LJ, Nakayama E (2003) NY-ESO-1 mRNA expression and immunogenicity in advanced prostate cancer. Cancer Immunity 3:10
Fossa A, Berner A, Fossa SD, Hernes E, Gaudernack G, Smeland EB (2004) NY-ESO-1 protein expression and humoral immune responses in prostate cancer. Prostate 59(4):440–447. https://doi.org/10.1002/pros.20025
Robbins PF, Morgan RA, Feldman SA, Yang JC, Sherry RM, Dudley ME, Wunderlich JR, Nahvi AV, Helman LJ, Mackall CL, Kammula US, Hughes MS, Restifo NP, Raffeld M, Lee CC, Levy CL, Li YF, El-Gamil M, Schwarz SL, Laurencot C, Rosenberg SA (2011) Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol 29(7):917–924. https://doi.org/10.1200/jco.2010.32.2537
Lai JP, Robbins PF, Raffeld M, Aung PP, Tsokos M, Rosenberg SA, Miettinen MM, Lee CC (2012) NY-ESO-1 expression in synovial sarcoma and other mesenchymal tumors: significance for NY-ESO-1-based targeted therapy and differential diagnosis. Modern Pathol 25(6):854–858. https://doi.org/10.1038/modpathol.2012.31
Harada N, Hoshiai K, Takahashi Y, Sakaguchi Y, Kuno T, Hishida T, Shiku H (2008) Preclinical safety pharmacology study of a novel protein-based cancer vaccine CHP-NY-ESO-1. Kobe J Med Sci 54(1):E23–E34
Kawabata R, Wada H, Isobe M, Saika T, Sato S, Uenaka A, Miyata H, Yasuda T, Doki Y, Noguchi Y, Kumon H, Tsuji K, Iwatsuki K, Shiku H, Ritter G, Murphy R, Hoffman E, Old LJ, Monden M, Nakayama E (2007) Antibody response against NY-ESO-1 in CHP-NY-ESO-1 vaccinated patients. Int J Cancer 120(10):2178–2184. https://doi.org/10.1002/ijc.22583
Uenaka A, Wada H, Isobe M, Saika T, Tsuji K, Sato E, Sato S, Noguchi Y, Kawabata R, Yasuda T, Doki Y, Kumon H, Iwatsuki K, Shiku H, Monden M, Jungbluth AA, Ritter G, Murphy R, Hoffman E, Old LJ, Nakayama E (2007) T cell immunomonitoring and tumor responses in patients immunized with a complex of cholesterol-bearing hydrophobized pullulan (CHP) and NY-ESO-1 protein. Cancer Immunity 7:9
Tsuji K, Hamada T, Uenaka A, Wada H, Sato E, Isobe M, Asagoe K, Yamasaki O, Shiku H, Ritter G, Murphy R, Hoffman EW, Old LJ, Nakayama E, Iwatsuki K (2008) Induction of immune response against NY-ESO-1 by CHP-NY-ESO-1 vaccination and immune regulation in a melanoma patient. Cancer Immunol Immunother 57(10):1429–1437. https://doi.org/10.1007/s00262-008-0478-5
Wada H, Sato E, Uenaka A, Isobe M, Kawabata R, Nakamura Y, Iwae S, Yonezawa K, Yamasaki M, Miyata H, Doki Y, Shiku H, Jungbluth AA, Ritter G, Murphy R, Hoffman EW, Old LJ, Monden M, Nakayama E (2008) Analysis of peripheral and local anti-tumor immune response in esophageal cancer patients after NY-ESO-1 protein vaccination. Int J Cancer 123(10):2362–2369. https://doi.org/10.1002/ijc.23810
Kageyama S, Wada H, Muro K, Niwa Y, Ueda S, Miyata H, Takiguchi S, Sugino SH, Miyahara Y, Ikeda H, Imai N, Sato E, Yamada T, Osako M, Ohnishi M, Harada N, Hishida T, Doki Y, Shiku H (2013) Dose-dependent effects of NY-ESO-1 protein vaccine complexed with cholesteryl pullulan (CHP-NY-ESO-1) on immune responses and survival benefits of esophageal cancer patients. J Transl Med 11:246. https://doi.org/10.1186/1479-5876-11-246
Sasaki T, Ishihara M, Kanda H, Hori Y, Soga N, Harada N, Miyahara Y, Kageyama S, Shiku H, Sugimura Y (2016) PD32-05 Phase I clinical study on the combination therapy of CHP-NY-ESO-1 cancer vaccine and MIS416 for the treatment of patients with NY-ESO-1 expressing refractory urothelial cancer or castration-resistant prostate cancer. J Urol 195(4S):e762–e762. https://doi.org/10.1016/j.juro.2016.02.681
Ishihara M, Tono Y, Miyahara Y, Harada N, Kageyama S, Sasaki T, Hori Y, Soga N, Uchida K, Shiraishi T, Sato E, Kanda H, Mizuno T, Webster G, Ikeda H, Katayama N, Sugimura Y, Shiku H (2018) First-in-human phase I clinical trial of NY-ESO-1 protein cancer vaccine with a novel adjuvant MIS416, NOD2 and TLR9 stimulant, for patients with NY-ESO-1 expressing solid tumors. J Clin Oncol 36 (15_suppl):e15176–e15176. doi: 10.1200/JCO.2018.36.15_suppl.e15176
Ishihara M, Seo N, Mitsui J, Muraoka D, Tanaka M, Mineno J, Ikeda H, Shiku H (2014) Systemic CD8+ T cell-mediated tumoricidal effects by intratumoral treatment of oncolytic herpes simplex virus with the agonistic monoclonal antibody for murine glucocorticoid-induced tumor necrosis factor receptor. PLoS ONE 9(8):e104669. https://doi.org/10.1371/journal.pone.0104669
Muraoka D, Seo N, Hayashi T, Tahara Y, Fujii K, Tawara I, Miyahara Y, Okamori K, Yagita H, Imoto S, Yamaguchi R, Komura M, Miyano S, Goto M, Sawada SI, Asai A, Ikeda H, Akiyoshi K, Harada N, Shiku H (2019) Antigen delivery targeted to tumor-associated macrophages overcomes tumor immune resistance. J Clin Invest 129(3):1278–1294. https://doi.org/10.1172/jci97642
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45 (2):228–247. doi:10.1016/j.ejca.2008.10.026
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Miyahara Y, Naota H, Wang L, Hiasa A, Goto M, Watanabe M, Kitano S, Okumura S, Takemitsu T, Yuta A, Majima Y, Lemonnier FA, Boon T, Shiku H (2005) Determination of cellularly processed HLA-A2402-restricted novel CTL epitopes derived from two cancer germ line genes, MAGE-A4 and SAGE. Clin Cancer Res 11(15):5581–5589. https://doi.org/10.1158/1078-0432.ccr-04-2585
Fujii K, Miyahara Y, Harada N, Muraoka D, Komura M, Yamaguchi R, Yagita H, Nakamura J, Sugino S, Okumura S, Imoto S, Miyano S, Shiku H (2017) Identification of an immunogenic neo-epitope encoded by mouse sarcoma using CXCR3 ligand mRNAs as sensors. Oncoimmunology 6(5):e1306617. https://doi.org/10.1080/2162402x.2017.1306617
Luckey AM, Anderson T, Silverman MH, Webster G (2015) Safety, tolerability and pharmacodynamics of a novel immunomodulator, MIS416, in patients with chronic progressive multiple sclerosis. Multiple sclerosis J Exp Transl Clin 1:2055217315583385. https://doi.org/10.1177/2055217315583385
Liang Z, Xie B, Li J, Wang X, Wang S, Meng S, Ji A, Zhu Y, Xu X, Zheng X, Xie L (2016) Hypertension and risk of prostate cancer: a systematic review and meta-analysis. Sci Rep 6:31358. https://doi.org/10.1038/srep31358
Wen Y, Crowley SD (2019) Renal effects of cytokines in hypertension. Adv Exp Med Biol 1165:443–454. https://doi.org/10.1007/978-981-13-8871-2_21
Mestas J, Hughes CC (2004) Of mice and not men: differences between mouse and human immunology. J Immunol 172(5):2731–2738
White M, Webster G, O'Sullivan D, Stone S, La Flamme AC (2014) Targeting innate receptors with MIS416 reshapes Th responses and suppresses CNS disease in a mouse model of multiple sclerosis. PLoS ONE 9(1):e87712. https://doi.org/10.1371/journal.pone.0087712
Fujii S, Shimizu K, Shimizu T, Lotze MT (2001) Interleukin-10 promotes the maintenance of antitumor CD8(+) T-cell effector function in situ. Blood 98(7):2143–2151. https://doi.org/10.1182/blood.v98.7.2143
Emmerich J, Mumm JB, Chan IH, LaFace D, Truong H, McClanahan T, Gorman DM, Oft M (2012) IL-10 directly activates and expands tumor-resident CD8(+) T cells without de novo infiltration from secondary lymphoid organs. Cancer Res 72(14):3570–3581. https://doi.org/10.1158/0008-5472.can-12-0721
Pollack SM, Jungbluth AA, Hoch BL, Farrar EA, Bleakley M, Schneider DJ, Loggers ET, Rodler E, Eary JF, Conrad EU, Jones RL, Yee C (2012) NY-ESO-1 is a ubiquitous immunotherapeutic target antigen for patients with myxoid/round cell liposarcoma. Cancer 118(18):4564–4570. https://doi.org/10.1002/cncr.27446
Bethune MT, Li XH, Yu J, McLaughlin J, Cheng D, Mathis C, Moreno BH, Woods K, Knights AJ, Garcia-Diaz A, Wong S, Hu-Lieskovan S, Puig-Saus C, Cebon J, Ribas A, Yang L, Witte ON, Baltimore D (2018) Isolation and characterization of NY-ESO-1-specific T cell receptors restricted on various MHC molecules. Proc Natl Acad Sci USA 115(45):E10702–e10711. https://doi.org/10.1073/pnas.1810653115
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, Oudard S, Theodore C, James ND, Turesson I, Rosenthal MA, Eisenberger MA (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351(15):1502–1512. https://doi.org/10.1056/NEJMoa040720
Tanaka N, Nishimura K, Okajima E, Ina K, Ogawa O, Nagata H, Akakura K, Fujimoto K, Gotoh M, Teramukai S, Hirao Y (2017) The efficacy and safety of docetaxel-based chemotherapy combined with dexamethasone 1 mg daily oral administration: JMTO Pca 10–01 phase II trial. Jpn J Clin Oncol 47(3):247–251. https://doi.org/10.1093/jjco/hyw193
Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, Miller K, Logothetis CJ, Shore ND, Small EJ, Carles J, Flaig TW, Taplin ME, Higano CS, de Souza P, de Bono JS, Griffin TW, De Porre P, Yu MK, Park YC, Li J, Kheoh T, Naini V, Molina A, Rathkopf DE (2015) Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 16(2):152–160. https://doi.org/10.1016/s1470-2045(14)71205-7
Chi KN, Protheroe A, Rodriguez-Antolin A, Facchini G, Suttman H, Matsubara N, Ye Z, Keam B, Damiao R, Li T, McQuarrie K, Jia B, De Porre P, Martin J, Todd MB, Fizazi K (2018) Patient-reported outcomes following abiraterone acetate plus prednisone added to androgen deprivation therapy in patients with newly diagnosed metastatic castration-naive prostate cancer (LATITUDE): an international, randomised phase 3 trial. Lancet Oncol 19(2):194–206. https://doi.org/10.1016/s1470-2045(17)30911-7
Small EJ, Schellhammer PF, Higano CS, Redfern CH, Nemunaitis JJ, Valone FH, Verjee SS, Jones LA, Hershberg RM (2006) Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol 24(19):3089–3094. https://doi.org/10.1200/jco.2005.04.5252
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF (2010) Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med 363(5):411–422. https://doi.org/10.1056/NEJMoa1001294
Yoshimura K, Minami T, Nozawa M, Kimura T, Egawa S, Fujimoto H, Yamada A, Itoh K, Uemura H (2016) A phase 2 randomized controlled trial of personalized peptide vaccine immunotherapy with low-dose dexamethasone versus dexamethasone alone in chemotherapy-naive castration-resistant prostate cancer. Eur Urol 70(1):35–41. https://doi.org/10.1016/j.eururo.2015.12.050
Cheever MA, Allison JP, Ferris AS, Finn OJ, Hastings BM, Hecht TT, Mellman I, Prindiville SA, Viner JL, Weiner LM, Matrisian LM (2009) The prioritization of cancer antigens: a national cancer institute pilot project for the acceleration of translational research. Clin Cancer Res 15(17):5323–5337. https://doi.org/10.1158/1078-0432.ccr-09-0737
Vansteenkiste JF, Cho BC, Vanakesa T, De Pas T, Zielinski M, Kim MS, Jassem J, Yoshimura M, Dahabreh J, Nakayama H, Havel L, Kondo H, Mitsudomi T, Zarogoulidis K, Gladkov OA, Udud K, Tada H, Hoffman H, Bugge A, Taylor P, Gonzalez EE, Liao ML, He J, Pujol JL, Louahed J, Debois M, Brichard V, Debruyne C, Therasse P, Altorki N (2016) Efficacy of the MAGE-A3 cancer immunotherapeutic as adjuvant therapy in patients with resected MAGE-A3-positive non-small-cell lung cancer (MAGRIT): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 17(6):822–835. https://doi.org/10.1016/s1470-2045(16)00099-1
Dreno B, Thompson JF, Smithers BM, Santinami M, Jouary T, Gutzmer R, Levchenko E, Rutkowski P, Grob JJ, Korovin S, Drucis K, Grange F, Machet L, Hersey P, Krajsova I, Testori A, Conry R, Guillot B, Kruit WHJ, Demidov L, Thompson JA, Bondarenko I, Jaroszek J, Puig S, Cinat G, Hauschild A, Goeman JJ, van Houwelingen HC, Ulloa-Montoya F, Callegaro A, Dizier B, Spiessens B, Debois M, Brichard VG, Louahed J, Therasse P, Debruyne C, Kirkwood JM (2018) MAGE-A3 immunotherapeutic as adjuvant therapy for patients with resected, MAGE-A3-positive, stage III melanoma (DERMA): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. https://doi.org/10.1016/s1470-2045(18)30254-7
Acknowledgements
We thank Ms. S. Sugino, Ms. K. Shirakura, Ms. J. Nakamura and Ms. T. Hayashi for technical assistance; Mr. Y. Ota and Prof. M. Nishikawa for data collection and administrative support; and Dr. S. Tamaru, Dr. I. Tanaka and Dr. M. Masuya for safety monitoring.
Funding
This study was supported by Grants from the Cancer Research Institute (New York, USA) and the Mie University School of Medicine. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
MI, NH, SK, YS and HS contributed to the design of the study. MI, YT, YM, NH, SK, TS, YH, NS, KU, TS, ES, HK, TM, HI, NK and YS contributed to patient recruitment, treatment and clinical data collection. DM and NH contributed to preclinical data collection and analysis. MI, YT, YM, NH, SK, GW and HS interpreted the data. MI and YT performed the statistical analyses. MI, YT, YM, NH, SK, GW and HS wrote the manuscript. All authors contributed to draft revisions and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
CHP-NY-ESO-1 was supplied by ImmunoFrontier Inc. (Osaka, Japan). N. Harada is a former employee of ImmunoFrontier Inc. H. Shiku is a stockholder of ImmunoFrontier Inc. MIS416 was supplied by Innate Immunotherapeutics Ltd. (Victoria, Australia). G.A. Webster is an employee of Innate Immunotherapeutics Ltd. The other authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in our studies involving human participants were conducted in accordance with Japanese Ethical Guidelines for Clinical Research, Japanese Guidelines for Medical and Health Research Involving Human Subjects, and the Helsinki declaration. The Institutional Review Board reviewed and approved the protocol and the informed consent documents and their amendments before use (Mie University approval numbers 817, 2201, 2203 and 2366). All animal experiments were conducted in accordance with the Fundamental Guidelines for Proper Conduct of Animal Experiment and Related Activities in Academic Research Institutions and approved by Mie University (Approval Number 24-14).
Animal source
Female BALB/c mice aged 6–10 weeks were purchased from Japan SLC, Inc. (Shizuoka, Japan).
Note regarding a previous publication
This study was presented in part at the 2016 Annual Meeting of the American Urological Association (AUA), May 8, 2016, San Diego, California, USA, Abstract 16-3843 [26] and at the 2018 Annual Meeting of the American Society of Clinical Oncology (ASCO), June 1–5, 2018, Chicago, Illinois, USA, Abstract e15176 [27].
Cell line authentication
The CT26 cell line (CRL-2638) was purchased from the American Type Culture Collection (Virginia, USA) and stably transfected with human NY-ESO-1 cDNA as described previously [9, 28].
Informed consent
Written informed consent to participate in the study and for the use of clinical data for research and publication was obtained from all patients included in the studies (Mie University Approval Numbers 2201, 2203 and 2366). Blood from healthy volunteers was obtained by laboratory members with the approval of Mie University (Approval Number 817). All healthy donors provided written informed consent to the use of their specimens for research and publication.
Availability of data and materials
To protect patient information in the clinical trial database, the datasets generated and/or analyzed in the present study are not publicly available, but they are available from the corresponding author on request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishihara, M., Tono, Y., Miyahara, Y. et al. First-in-human phase I clinical trial of the NY-ESO-1 protein cancer vaccine with NOD2 and TLR9 stimulants in patients with NY-ESO-1-expressing refractory solid tumors. Cancer Immunol Immunother 69, 663–675 (2020). https://doi.org/10.1007/s00262-020-02483-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-020-02483-1