Abstract
Purpose
To describe ultrasound (US) quality for hepatocellular carcinoma (HCC) screening/surveillance using the US LI-RADS scoring system, and to assess predictive factors of worse US quality scores.
Methods
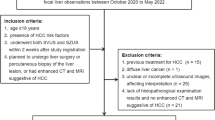
This retrospective study included adult patients (n = 470; M/F 264/206, median age 59y) at risk for HCC that underwent US for HCC screening/surveillance. US examinations were independently reviewed by 2 radiologists that assigned a visualization score (A: no/minimal, B: moderate, C: severe limitation) and US diagnostic category (US LI-RADS 1: negative, US LI-RADS 2: subthreshold, US LI-RADS 3: positive) to each study. A generalized linear mixed model was used to assess the predictive factors of worse visualization score using OR (odds ratio) statistics. Simple Kappa coefficient (K) assessed inter-reader agreement.
Results
For readers 1 and 2, 295/320 (62.8%/68.1%) cases were scored A, 153/134 (32.6%/28.5%) were scored B, and 22/16 (4.6%/3.4%) were scored C, respectively. There was moderate inter-reader agreement for US LI-RADS visualization score (K = 0.478) and 100% concordance for US diagnostic category (K = 1), with 30 (6.4%) cases scored as positive (US LI-RADS 3). Cirrhosis and obesity were significant independent predictors of worse visualization scores (B/C) (cirrhosis: OR 10.4 confidence intervals: [4.25–25.48], p < 0.001; obesity: OR 3.61 [2.11–6.20], p < 0.001). Of the 30 lesions scored as US LI-RADS 3, 9 were characterized as probable or definite HCC on confirmatory CT/MRI, yielding a PPV of 30% (9/30) and a false-positive rate of 70% (21/30).
Conclusion
Moderate to severe limitations in quality of US performed for HCC screening/surveillance was observed in approximately one-third of patients. Patients with cirrhosis and/or elevated BMI have poorer quality US studies and may benefit from other screening modalities such as CT or MRI.




Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- ALD:
-
Alcoholic liver disease
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HCC:
-
Hepatocellular carcinoma
- LI-RADS:
-
Liver imaging reporting and data system
- MRI:
-
Magnetic resonance imaging
- NASH:
-
Nonalcoholic steatohepatitis
- US:
-
Ultrasound
References
Tang, A., et al., Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol (NY), 2018. 43(1): p. 13-25.
Jemal, A., et al., Annual Report to the Nation on the Status of Cancer, 1975-2014, Featuring Survival. J Natl Cancer Inst, 2017. 109(9).
Tzartzeva, K., et al., Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients With Cirrhosis: A Meta-analysis. Gastroenterology, 2018. 154(6): p. 1706-1718.e1.
Singal, A.G., A. Pillai, and J. Tiro, Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med, 2014. 11(4): p. e1001624.
Kansagara, D., et al., Screening for hepatocellular carcinoma in chronic liver disease: a systematic review. Ann Intern Med, 2014. 161(4): p. 261-9.
Zhang, B.H., B.H. Yang, and Z.Y. Tang, Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol, 2004. 130(7): p. 417-22.
Morgan, T.A., et al., US LI-RADS: ultrasound liver imaging reporting and data system for screening and surveillance of hepatocellular carcinoma. Abdom Radiol (NY), 2018. 43(1): p. 41-55.
Song, P., et al., The clinical management of hepatocellular carcinoma worldwide: A concise review and comparison of current guidelines from 2001 to 2017. Biosci Trends, 2017. 11(4): p. 389-398.
Fetzer, D.T., et al., Screening and Surveillance of Hepatocellular Carcinoma: An Introduction to Ultrasound Liver Imaging Reporting and Data System. Radiol Clin North Am, 2017. 55(6): p. 1197-1209.
Radiology, A.C.o. Ultrasound LI-RADS v2017. [cited 2022 January 19]; Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/Ultrasound-LI-RADS-v2017.
Millet, J.D., et al., ACR Ultrasound Liver Reporting and Data System: Multicenter Assessment of Clinical Performance at One Year. J Am Coll Radiol, 2019. 16(12): p. 1656-1662.
Kiri, L., et al., US LI-RADS Visualization Score: Interobserver Variability and Association With Cause of Liver Disease, Sex, and Body Mass Index. Can Assoc Radiol J, 2022. 73(1): p. 68-74.
Hernandez-Meza, G., et al., MRI is the most commonly used imaging modality for HCC screening at a tertiary care transplant center. Abdom Radiol (NY), 2021. 46(11): p. 5142-5151.
Radiology, A.C.o. Ultrasound LI-RADS® v2017. 2017 06/01/2021]; Available from: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/Ultrasound-LI-RADS-v2017.
Landis, J.R. and G.G. Koch, The measurement of observer agreement for categorical data. Biometrics, 1977. 33(1): p. 159-74.
Sevco, T.J., et al., Ultrasound (US) LI-RADS: Outcomes of Category US-3 Observations. AJR Am J Roentgenol, 2021. 217(3): p. 644-650.
Samoylova, M.L., et al., Predictors of Ultrasound Failure to Detect Hepatocellular Carcinoma. Liver Transpl, 2018. 24(9): p. 1171-1177.
Simmons, O., et al., Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther, 2017. 45(1): p. 169-177.
Brahee, D.D., et al., Body Mass Index and Abdominal Ultrasound Image Quality:A Pilot Survey of Sonographers. Journal of Diagnostic Medical Sonography, 2013. 29(2): p. 66-72.
Paladini, D., Sonography in obese and overweight pregnant women: clinical, medicolegal and technical issues. Ultrasound Obstet Gynecol, 2009. 33(6): p. 720-9.
Joshi, K., et al., Hepatocellular carcinoma surveillance: a national survey of current practices in the USA. Dig Dis Sci, 2014. 59(12): p. 3073-7.
Kim, S.Y., et al., MRI With Liver-Specific Contrast for Surveillance of Patients With Cirrhosis at High Risk of Hepatocellular Carcinoma. JAMA Oncol, 2017. 3(4): p. 456-463.
Colli, A., et al., Accuracy of ultrasonography, spiral CT, magnetic resonance, and alpha-fetoprotein in diagnosing hepatocellular carcinoma: a systematic review. Am J Gastroenterol, 2006. 101(3): p. 513-23.
Arguedas, M.R., et al., Screening for hepatocellular carcinoma in patients with hepatitis C cirrhosis: a cost-utility analysis. Am J Gastroenterol, 2003. 98(3): p. 679-90.
Tiyarattanachai, T., D.T. Fetzer, and A. Kamaya, Multicenter Study of ACR Ultrasound LI-RADS Visualization Scores on Serial Examinations: Implications for Changes in Surveillance Strategies. AJR Am J Roentgenol, 2022.
An, J.Y., et al., Abbreviated MRI for Hepatocellular Carcinoma Screening and Surveillance. Radiographics, 2020. 40(7): p. 1916-1931.
Bartolotta, T.V., et al., Contrast-enhanced ultrasound of hepatocellular carcinoma: where do we stand? Ultrasonography, 2019. 38(3): p. 200-214.
Besa, C., et al., Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdominal Radiology, 2017. 42(1): p. 179-190.
Vietti Violi, N., et al., Abbreviated Magnetic Resonance Imaging for HCC Surveillance. Clin Liver Dis (Hoboken), 2021. 17(3): p. 133-138.
Acknowledgements
The remaining authors did not receive support from any organization for the submitted work.
Funding
The remaining authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
Bachir Taouli, MD, MHA: Research support/grant: Bayer, Takeda, Regeneron, Helio Health, Siemens, Echosens. Consultant: Bayer, Guerbet.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
King, M.J., Lee, K.M., Rosberger, S. et al. HCC screening with ultrasound: assessment of quality using ultrasound LI-RADS score. Abdom Radiol 48, 263–270 (2023). https://doi.org/10.1007/s00261-022-03702-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03702-2