Abstract
Purpose
Testicular stromal tumors are uncommon, although mostly benign. The purpose of this study is to assess the role of multi-parametric MRI in differentiating benign testicular stromal tumors from malignant testicular neoplasms (non-stromal and stromal).
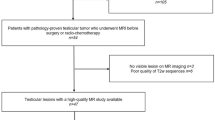
Methods
A single-center retrospective study comparing benign stromal tumors (STs) to malignant testicular neoplasms (MTNs) was conducted. MR imaging assessment included tumor size, T2- and T1-weighted signal intensity, T2- and T1-weighted texture pattern, diffusion restriction, presence of hemorrhage and/or necrosis, and measurement of apparent diffusion coefficient and dynamic contrast enhancement (DCE). Inter-observer agreement was assessed using Cohen’s kappa and Bland–Altman and data were compared using independent t-tests or χ2. Receiver operating characteristic curve analysis was used to test models incorporating various imaging features.
Results
Radical orchiectomy and histopathology revealed 20 testicular neoplasms: seven STs (35%) and thirteen MTNs (65%). MTNs were significantly larger in size than STs (5.1 ± 2.36 cm vs. 1.27 ± 0.56 cm; p-value < 0.001). STs demonstrated more hypointense T2W signal (85.7% vs. 46.2%; p-value < 0.09), less T2W heterogeneous texture (14.3% vs. 61.5%; p-value < 0.04), and less diffusion restriction (16.7% vs. 83.3%; p-value < 0.01) in comparison to MTNs. STs demonstrated mainly homogenous post-contrast enhancement pattern (71.4% vs. 7.7%; p-value < 0.004), while MTNs showed primarily heterogeneous enhancement pattern (77% vs. 14.3%; p-value < 0.02). STs revealed greater corrected venous phase enhancement (STs: 0.59 ± 0.29; MTNs: 0.25 ± 0.25; p-value < 0.03). STs showed higher ADC values, though the difference was not statistically significant (p-value < 0.25). A model combining T2W, DWI, and DCE features showed the best overall diagnostic accuracy with area under ROC curve of 0.99 and confidence interval ranging from 0.94 to 1.
Conclusion
Multi-parametric MRI can potentially differentiate benign stromal tumors from malignant testicular neoplasms, which can help to avoid radical orchiectomy. However, future studies using larger sample sizes are needed to validate our results.






Similar content being viewed by others
References
Coursey Moreno C, Small WC, Camacho JC, Master V, Kokabi N, Lewis M, Hartman M, Mittal PK (2015) Testicular tumors: what radiologists need to know–differential diagnosis, staging, and management. Radiographics 35 (2):400-415. https://doi.org/10.1148/rg.352140097
Einhorn LH (2002) Curing metastatic testicular cancer. Proceedings of the National Academy of Sciences 99 (7):4592-4595. https://doi.org/10.1073/pnas.072067999
Garner MJ, Turner MC, Ghadirian P, Krewski D (2005) Epidemiology of testicular cancer: an overview. Int J Cancer 116 (3):331-339. https://doi.org/10.1002/ijc.21032
Liu S, Wen SW, Mao Y, Mery L, Rouleau J (1999) Birth cohort effects underlying the increasing testicular cancer incidence in Canada. Can J Public Health 90 (3):176-180
Ulbright TM (2005) Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues. Mod Pathol 18 Suppl 2:S61-79. https://doi.org/10.1038/modpathol.3800310
Krag Jacobsen G, Barlebo H, Olsen J, Schultz HP, Starklint H, Sogaard H, Vaeth M (1984) Testicular germ cell tumours in Denmark 1976-1980. Pathology of 1058 consecutive cases. Acta Radiol Oncol 23 (4):239-247. https://doi.org/10.3109/02841868409136019
Tsili AC, Argyropoulou MI, Giannakis D, Sofikitis N, Tsampoulas K (2010) MRI in the characterization and local staging of testicular neoplasms. AJR Am J Roentgenol 194 (3):682-689. https://doi.org/10.2214/AJR.09.3256
Mohrs OK, Thoms H, Egner T, Brunier A, Eiers M, Kauczor HU, Hallscheidt P (2012) MRI of patients with suspected scrotal or testicular lesions: diagnostic value in daily practice. AJR Am J Roentgenol 199 (3):609-615. https://doi.org/10.2214/AJR.11.7349
Tsili AC, Tsampoulas C, Giannakopoulos X, Stefanou D, Alamanos Y, Sofikitis N, Efremidis SC (2007) MRI in the histologic characterization of testicular neoplasms. AJR Am J Roentgenol 189 (6):W331-337. https://doi.org/10.2214/AJR.07.2267
Tsili AC, Argyropoulou MI, Giannakis D, Tsampalas S, Sofikitis N, Tsampoulas K (2012) Diffusion-weighted MR imaging of normal and abnormal scrotum: preliminary results. Asian J Androl 14 (4):649-654. https://doi.org/10.1038/aja.2011.172
Watanabe Y, Dohke M, Ohkubo K, Ishimori T, Amoh Y, Okumura A, Oda K, Hayashi T, Dodo Y, Arai Y (2000) Scrotal disorders: evaluation of testicular enhancement patterns at dynamic contrast-enhanced subtraction MR imaging. Radiology 217 (1):219-227. https://doi.org/10.1148/radiology.217.1.r00oc41219
Algebally AM, Tantawy HI, Yousef RR, Szmigielski W, Darweesh A (2015) Advantage of Adding Diffusion Weighted Imaging to Routine MRI Examinations in the Diagnostics of Scrotal Lesions. Pol J Radiol 80:442-449. https://doi.org/10.12659/PJR.894399
Reinges MHT, Kaiser WA, Miersch WD, Vogel J, Reiser M (1995) Dynamic MRI of benign and malignant testicular lesions: preliminary observations. European Radiology 5 (6). https://doi.org/10.1007/bf00190927
Tsili AC, Bertolotto M, Turgut AT, Dogra V, Freeman S, Rocher L, Belfield J, Studniarek M, Ntorkou A, Derchi LE, Oyen R, Ramchandani P, Secil M, Richenberg J (2018) MRI of the scrotum: Recommendations of the ESUR Scrotal and Penile Imaging Working Group. Eur Radiol 28 (1):31-43. https://doi.org/10.1007/s00330-017-4944-3
El Sanharawi I, Correas JM, Glas L, Ferlicot S, Izard V, Ducot B, Bellin MF, Benoit G, Rocher L (2016) Non-palpable incidentally found testicular tumors: Differentiation between benign, malignant, and burned-out tumors using dynamic contrast-enhanced MRI. Eur J Radiol 85 (11):2072-2082. https://doi.org/10.1016/j.ejrad.2016.09.021
Tsitouridis I, Maskalidis C, Panagiotidou D, Kariki EP (2014) Eleven patients with testicular leydig cell tumors: clinical, imaging, and pathologic correlation. J Ultrasound Med 33 (10):1855-1864. https://doi.org/10.7863/ultra.33.10.1855
Giannarini G, Dieckmann KP, Albers P, Heidenreich A, Pizzocaro G (2010) Organ-sparing surgery for adult testicular tumours: a systematic review of the literature. Eur Urol 57 (5):780-790. https://doi.org/10.1016/j.eururo.2010.01.014
Giannarini G, Mogorovich A, Menchini Fabris F, Morelli G, De Maria M, Manassero F, Loggini B, Pingitore R, Cavazzana A, Selli C (2007) Long-term followup after elective testis sparing surgery for Leydig cell tumors: a single center experience. J Urol 178 (3 Pt 1):872-876; quiz 1129. https://doi.org/10.1016/j.juro.2007.05.077
Loeser A, Vergho DC, Katzenberger T, Brix D, Kocot A, Spahn M, Gerharz EW, Riedmiller H (2009) Testis-sparing surgery versus radical orchiectomy in patients with Leydig cell tumors. Urology 74 (2):370-372. https://doi.org/10.1016/j.urology.2009.03.014
Suardi N, Strada E, Colombo R, Freschi M, Salonia A, Lania C, Cestari A, Carmignani L, Guazzoni G, Rigatti P, Montorsi F (2009) Leydig cell tumour of the testis: presentation, therapy, long-term follow-up and the role of organ-sparing surgery in a single-institution experience. BJU Int 103 (2):197-200. https://doi.org/10.1111/j.1464-410X.2008.08016.x
Matei DV, Vartolomei MD, Renne G, Tringali VML, Russo A, Bianchi R, Cozzi G, Bottero D, Musi G, Mazzarol G, Ferro M, de Cobelli O (2017) Reliability of Frozen Section Examination in a Large Cohort of Testicular Masses: What Did We Learn? Clin Genitourin Cancer 15 (4):e689-e696. https://doi.org/10.1016/j.clgc.2017.01.012
Heidenreich A, Paffenholz P, Nestler T, Pfister D (2019) European Association of Urology Guidelines on Testis Cancer: Important Take Home Messages. Eur Urol Focus 5 (5):742-744. https://doi.org/10.1016/j.euf.2019.08.002
Hansford BG, Peng Y, Jiang Y, Vannier MW, Antic T, Thomas S, McCann S, Oto A (2015) Dynamic Contrast-enhanced MR Imaging Curve-type Analysis: Is It Helpful in the Differentiation of Prostate Cancer from Healthy Peripheral Zone? Radiology 275 (2):448-457. https://doi.org/10.1148/radiol.14140847
Shaida N, Berman LH (2012) Percutaneous testicular biopsy for indeterminate testicular lesions. Br J Radiol 85 Spec No 1:S54-58. https://doi.org/10.1259/bjr/30496032
Sun MR, Ngo L, Genega EM, Atkins MB, Finn ME, Rofsky NM, Pedrosa I (2009) Renal cell carcinoma: dynamic contrast-enhanced MR imaging for differentiation of tumor subtypes–correlation with pathologic findings. Radiology 250 (3):793-802. https://doi.org/10.1148/radiol.2503080995
Koo HR, Cho N, Song IC, Kim H, Chang JM, Yi A, Yun BL, Moon WK (2012) Correlation of perfusion parameters on dynamic contrast-enhanced MRI with prognostic factors and subtypes of breast cancers. J Magn Reson Imaging 36 (1):145-151. https://doi.org/10.1002/jmri.23635
Thomassin-Naggara I, Bazot M, Darai E, Callard P, Thomassin J, Cuenod CA (2008) Epithelial ovarian tumors: value of dynamic contrast-enhanced MR imaging and correlation with tumor angiogenesis. Radiology 248 (1):148-159. https://doi.org/10.1148/radiol.2481071120
Tsili AC, Argyropoulou MI, Astrakas LG, Ntoulia EA, Giannakis D, Sofikitis N, Tsampoulas K (2013) Dynamic contrast-enhanced subtraction MRI for characterizing intratesticular mass lesions. AJR Am J Roentgenol 200 (3):578-585. https://doi.org/10.2214/AJR.12.9064
Cornelis F, Tricaud E, Lasserre AS, Petitpierre F, Bernhard JC, Le Bras Y, Yacoub M, Bouzgarrou M, Ravaud A, Grenier N (2014) Routinely performed multiparametric magnetic resonance imaging helps to differentiate common subtypes of renal tumours. Eur Radiol 24 (5):1068-1080. https://doi.org/10.1007/s00330-014-3107-z
Tsili AC, Sylakos A, Ntorkou A, Stavrou S, Astrakas LG, Sofikitis N, Argyropoulou MI (2015) Apparent diffusion coefficient values and dynamic contrast enhancement patterns in differentiating seminomas from nonseminomatous testicular neoplasms. Eur J Radiol 84 (7):1219-1226. https://doi.org/10.1016/j.ejrad.2015.04.004
Manganaro L, Vinci V, Pozza C, Saldari M, Gianfrilli D, Pofi R, Bernardo S, Cantisani V, Lenzi A, Scialpi M, Catalano C, Isidori AM (2015) A prospective study on contrast-enhanced magnetic resonance imaging of testicular lesions: distinctive features of Leydig cell tumours. Eur Radiol 25 (12):3586-3595. https://doi.org/10.1007/s00330-015-3766-4
Talakic E TS SH, Manfred T (2014) Diffusion Weighted Imaging of Testicular Tumors – Is there a Value for Differentiation between Benign and Malignant?. Radiological Society of North America
Serra AD, Hricak H, Coakley FV, Kim B, Dudley A, Morey A, Tschumper B, Carroll PR (1998) Inconclusive Clinical and Ultrasound Evaluation of the Scrotum: Impact of Magnetic Resonance Imaging on Patient Management and Cost. Urology 51 (6):1018-1021. https://doi.org/10.1016/s0090-4295(98)00097-1
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khanna, M., Abualruz, A.R., Yadav, S.K. et al. Diagnostic performance of multi-parametric MRI to differentiate benign sex cord stromal tumors from malignant (non-stromal and stromal) testicular neoplasms. Abdom Radiol 46, 319–330 (2021). https://doi.org/10.1007/s00261-020-02621-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02621-4