Abstract
Purpose
To validate the use of a split-bolus pancreas CTA protocol for local staging of pancreatic cancer and to evaluate its ability to detect and characterize liver lesions.
Methods
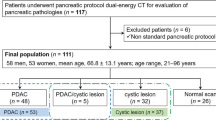
Consecutive patients with pancreatic cancer who underwent split-bolus pancreas CTA between 12/2015 and 12/2016 were included in this IRB-approved HIPAA-compliant retrospective study. Objective evaluation of the abdominal vessels, the pancreas, the liver, and lesions, if present, was performed with attenuation measurements and tumor conspicuity and contrast-to-noise ratio (CNR) calculations. An abdominal radiologist with 20 years of experience performed subjective evaluation of image quality and blindly detected and characterized liver lesions. Any inconclusive findings or grading scores were evaluated in consensus with another abdominal radiologist with 7 years of experience. Liver findings were validated using a composite reference standard to assess accuracy.
Results
There were 82 pancreatic cancer patients with a total of 91 liver findings. Tumor conspicuity and CNR were 60.8 ± 35.1 HU and 8.0 ± 5.8 for the pancreatic lesions and 58 ± 34.7 HU and 9.7 ± 6.3 for the liver lesions, respectively. The accuracy, sensitivity, and specificity of the split-bolus protocol for the hepatic findings were correspondingly 89/91 (97.8%, 95% CI 92.3–99.4), 58/60 (96.7%, 95% CI 88.6–99.1), and 33/33 (100%, 95% CI 89.6–100). The subjective image quality ratings were optimal in more than 89% of the cases for various structures, with no non-diagnostic ratings.
Conclusion
Split-bolus pancreas CTA protocol allows for detection and staging of pancreatic cancer, both for the primary tumor and detection and characterization of liver lesions.




Similar content being viewed by others
References
Vincent A, Herman J, Schulick R, Hruban RH, Goggins M (2011) Pancreatic cancer. Lancet 378(9791):607–620
Tamm E, Charnsangavej C (2001) Pancreatic cancer: current concepts in imaging for diagnosis and staging. Cancer J 7(4):298–311
Thota R, Pauff JM, Berlin JD (2014) Treatment of metastatic pancreatic adenocarcinoma: a review. Oncology 28(1):70–74
Zanini N, Lombardi R, Masetti M, et al. (2015) Surgery for isolated liver metastases from pancreatic cancer. Updates Surg 67(1):19–25
Lee ES, Lee JM (2014) Imaging diagnosis of pancreatic cancer: a state-of-the-art review. World J Gastroenterol 20(24):7864–7877
De La Cruz MS, Young AP, Ruffini MTZS (2014) Diagnosis and management of pancreatic cancer. Am Fam Physician 89(8):626–632
Scialpi M, Palumbo B, Pierotti L, et al. (2014) Detection and characterization of focal liver lesions by split-bolus multidetector-row CT: diagnostic accuracy and radiation dose in oncologic patients. Anticancer Res 4344:4335–4344
Brady A, Laoide RÓ, McCarthy P, McDermott R (2012) Discrepancy and error in radiology: concepts, causes and consequences. Ulster Med J 81:3–9
Sokolovskaya E, Shinde T, Ruchman RB, et al. (2015) The effect of faster reporting speed for imaging studies on the number of misses and interpretation errors: a pilot study. J Am Coll Radiol 12(7):683–688
Mileto A, Mazziotti S, Gaeta M, et al. (2012) Pancreatic dual-source dual-energy CT: is it time to discard unenhanced imaging? Clin Radiol 67:334–339
Brook OR, Gourtsoyianni S, Brook A, et al. (2013) Split-bolus spectral multidetector CT of the Pancreas: assessment of radiation dose and tumor conspicuity. Radiology 269(1):139–148
Schwartz LH, Gandras EJ, Colangelo SM, Ercolani MC, Panicek DM (1999) Prevalence and importance of small hepatic lesions found at CT in patients with cancer. Radiology 210(1):71–74
Scialpi M, Pierotti L, Gravante S, et al. (2014) Split-bolus versus triphasic multidetector-row computed tomography technique in the diagnosis of hepatic focal nodular hyperplasia: a case report. J Med Case Rep 8:425
Jiang J, Wang K, Xu Y, et al. (2017) Preoperative assessment of hepatocellular carcinoma with split-bolus combined phase contrast-enhanced computed tomography. Med Sci Mon 23:1834–1841
Jacobs JE, Birnbaum BA (1995) Computed tomography imaging of focal hepatic lesions. Semin Roentgenol 30(4):308–323
Prasad SR, Wang H, Rosas H, et al. (2005) Fat-containing lesions of the liver: radiologic-pathologic correlation. RadioGraphics 25(2):321–331
Macari M, Spieler B, Kim D, et al. (2010) Dual-source dual-energy MDCT of pancreatic adenocarcinoma: initial observations with data generated at 80 kVp and at simulated weighted- average 120 kVp. Am J Roentgenol 194(1):27–32
Fletcher JG, Wiersema MJ, Farrell MA, et al. (2003) Pancreatic malignancy: value of arterial, pancreatic, and hepatic phase imaging with multi-detector row CT. Radiology 229(1):81–90
Schiller I, van Smeden M, Hadgu A, et al. (2016) Bias due to composite reference standards in diagnostic accuracy studies. Stat Med 35(9):1454–1470
Naaktgeboren CA, Bertens LC, Van Smeden M (2013) Value of composite reference standards in diagnostic research. BMJ 347:1–9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors state that this work has not received any funding.
Conflicts of interest
The authors of this article declare that they have no conflicts of interest to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Appendix
Rights and permissions
About this article
Cite this article
Camacho, A., Fang, J., Cohen, M.P. et al. Split-bolus pancreas CTA protocol for local staging of pancreatic cancer and detection and characterization of liver lesions. Abdom Radiol 43, 340–350 (2018). https://doi.org/10.1007/s00261-017-1350-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1350-x