Abstract
Purpose
To examine outcomes and complications of percutaneous transhepatic biliary drainage (PTBD) performed via the right or left lobe and different entry levels (lobar, segmental, subsegmental, sub-subsegmental).
Methods
The records of patients who underwent PTBD for obstructive jaundice from 2008 to 2015 were retrospectively reviewed. Logistic regression analysis was performed to determine factors associated with outcomes and complications based on entry side and entry level. PTBD success was defined as a total bilirubin decrease after catheter placement.
Results
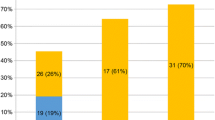
The data of 446 patients (mean age 68.4 years) were included. Multivariate logistic regression revealed a decrease of bilirubin level was associated with left lobe (vs. right) entry [adjusted odds ratio (aOR) = 2.657, 95% confidence interval (CI) 1.160, 6.087], external drainage (aOR = 2.908, 95% CI 1.226, 6.897), and liver volume undrained <50% (aOR = 2.623, 95% CI 1.045, 6.581). PTBD success was increased with left lobe entry (aOR = 1.853, 95% CI 1.167, 2.940) and associated with entry level (subsegmental vs. lobar, aOR = 2.992, 95% CI 1.258, 7.114; sub-subsegmental vs. lobar, aOR = 3.711, 95% CI 1.383, 9.956). Complications were significantly decreased with left lobe entry (aOR = 0.450, 95% CI 0.263, 0.769) and associated with entry level (segmental vs. lobar, aOR = 0.359, 95% CI 0.148, 0.873; subsegmental vs. lobar, aOR = 0.248, 95% CI 0.10, 0.615; sub-subsegmental vs. lobar, aOR = 0.129, 95% CI 0.041, 0.411).
Conclusions
The success and complications of PTBD vary with entry side and level.


Similar content being viewed by others
References
Fidelman N (2015) Benign biliary strictures: diagnostic evaluation and approaches to percutaneous treatment. Tech Vasc Interv Radiol 18(4):210–217
Sutter CM, Ryu RK (2015) Percutaneous management of malignant biliary obstruction. Tech Vasc Interv Radiol 18(4):218–226
Chandrashekhara SH, Gamanagatti S, Singh A, Bhatnagar S (2016) Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: a review. Indian J Palliat Care 22:378–387
Papadopoulos V, Filippou D, Manolis E, Mimidis K (2007) Haemostasis impairment in patients with obstructive jaundice. J Gastrointestin Liver Dis 16(2):177–186
Hara K, Yamao K, Mizuno N, et al. (2016) Endoscopic ultrasonography-guided biliary drainage: who, when, which, and how? World J Gastroenterol 22(3):1297–1303
Wiggers JK, Coelen RJ, Rauws EA, et al. (2015) Preoperative endoscopic versus percutaneous transhepatic biliary drainage in potentially resectable perihilar cholangiocarcinoma (DRAINAGE trial): design and rationale of a randomized controlled trial. BMC Gastroenterol 15:20. doi:10.1186/s12876-015-0251-0
Shimizu H, Kato A, Takayashiki T, et al. (2015) Peripheral portal vein-oriented non-dilated bile duct puncture for percutaneous transhepatic biliary drainage. World J Gastroenterol 21(44):12628–12634
Winick AB, Waybill PN, Venbrux AC (2001) Complications of percutaneous transhepatic biliary interventions. Tech Vasc Interv Radiol 4(3):200–206
Bret PM, de Stempel JV, Atri M, Lough JO, Illescas FF (1998) Intrahepatic bile duct and portal vein anatomy revisited. Radiology 169(2):405–407
Kitami M, Takase K, Murakami G, et al. (2006) Types and frequencies of biliary tract variations associated with a major portal venous anomaly: analysis with multi-detector row CT cholangiography. Radiology 238(1):156–166
Cho A, Okazumi S, Yoshinaga Y, et al. (2003) Relationship between left biliary duct system and left portal vein: evaluation with three-dimensional portocholangiography. Radiology 228(1):246–250
Jaques PF, Mandell VS, Delany DJ, et al. (1982) Percutaneous transhepatic biliary drainage: advantages of the left-lobe subxiphoid approach. Radiology 145(2):534–536
Hayashi N, Sakai T, Kitagawa M, et al. (1997) US-guided left-sided biliary drainage: nine-year experience. Radiology 204(1):119–122
Rivera-Sanfeliz GM, Assar OS, LaBerge JM, et al. (2004) Incidence of important hemobilia following transhepatic biliary drainage: left-sided versus right-sided approaches. Cardiovasc Interv Radiol 27(2):137–139
Hamada T, Yasunaga H, Nakai Y, et al. (2015) Severe bleeding after percutaneous transhepatic drainage of the biliary system: effect of antithrombotic agents–analysis of 34 606 cases from a Japanese nationwide administrative database. Radiology 274(2):605–613
Catalano OA, Singh AH, Uppot RN, et al. (2008) Vascular and biliary variants in the liver: implications for liver surgery. Radiographics 28(2):359–378
Fidelman N, Bloom AI, Kerlan RK Jr, et al. (2008) Hepatic arterial injuries after percutaneous biliary interventions in the era of laparoscopic surgery and liver transplantation: experience with 930 patients. Radiology 247(3):880–886
Lucatelli P, Corradini SG, Corona M, et al. (2016) Risk factors for immediate and delayed-onset fever after percutaneous transhepatic biliary drainage. Cardiovasc Interv Radiol 39(5):746–755
Sumiyoshi T, Shima Y, Okabayashi T, et al. (2014) Functional discrepancy between two liver lobes after hemilobe biliary drainage in patients with jaundice and bile duct cancer: an appraisal using (99m)Tc-GSA SPECT/CT fusion imaging. Radiology 273(2):444–451
Choi SH, Gwon D, Ko GY, et al. (2011) Hepatic arterial injuries in 3110 patients following percutaneous transhepatic biliary drainage. Radiology 261(3):969–975
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, YS., Lin, CY., Chuang, MT. et al. Success and complications of percutaneous transhepatic biliary drainage are influenced by liver entry segment and level of catheter placement. Abdom Radiol 43, 713–722 (2018). https://doi.org/10.1007/s00261-017-1258-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1258-5