Abstract
Purpose
To calculate the diagnostic performance of [18F]-FDG PET/MR in colorectal cancer (CRC).
Methods
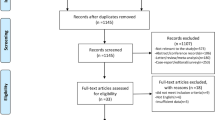
This study was designed following the PRISMA-DTA guidelines. To be included, published original articles (until December 31, 2021) that met the following criteria were considered eligible: (1) evaluated [18F]-FDG PET/MR as the diagnostic method to detect CRC; (2) compared [18F]-FDG PET/MR with histopathology as the reference standard, or clinical/imaging composite follow-up when pathology was not available; (3) provided adequate crude data for meta-analysis. The diagnostic pooled measurements were calculated at patient and lesion levels. Regarding sub-group analysis, diagnostic measurements were calculated in “TNM staging,” “T staging,” “N staging,” “M staging,” and “liver metastasis” sub-groups. Additionally, we calculated the pooled performances in “rectal cancer: patient-level” and “rectal cancer: lesion-level” sub-groups. A hierarchical method was used to pool the performances. The bivariate model was conducted to find the summary points. Analyses were performed using STATA 16.
Results
A total of 1534 patients from 18 studies were entered. The pooled sensitivities in CRC lesion detection (tumor, lymph nodes, and metastases) were 0.94 (95%CI: 0.89–0.97) and 0.93 (95%CI: 0.82–0.98) at patient-level and lesion-level, respectively. The pooled specificities were 0.89 (95%CI: 0.84–0.93) and 0.95 (95%CI: 0.90–0.98) at patient-level and lesion-level, respectively. In sub-groups, the highest sensitivity (0.97, 95%CI: 0.86–0.99) and specificity (0.99, 95%CI: 0.84–1.00) were calculated for “M staging” and “rectal cancer: lesion-level,” respectively. The lowest sensitivity (0.81, 95%CI: 0.65–0.91) and specificity (0.79, 95%CI: 0.52–0.93) were calculated for “N staging” and “T staging,” respectively.
Conclusion
This meta-analysis showed an overall high diagnostic performance for [18F]-FDG PET/MR in detecting CRC lesions/metastases. Thus, this modality can play a significant role in several clinical scenarios in CRC staging and restaging. Specifically, one of the main strengths of this modality is ruling out the existence of CRC lesions/metastases. Finally, the overall diagnostic performance was not found to be affected in the post-treatment setting.




Similar content being viewed by others
Data availability
The detailed data generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, et al. Colorectal cancer statistics, 2020. CA: a cancer journal for clinicians. 2020. 70(3): 145–164.
Granados-Romero JJ, et al. Colorectal cancer: a review. Int J Res Med Sci. 2017;5(11):4667–76.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16(12):713–32.
Hadjipetrou A, et al. Colorectal cancer, screening and primary care: a mini literature review. World J Gastroenterol. 2017;23(33):6049.
Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021;325(7):669–85.
Balyasnikova S, Brown G. Imaging advances in colorectal cancer. Curr Colorectal Cancer Rep. 2016;12(3):162–9.
Goiffon R, O'Shea A, Harisinghani M. Advances in radiological staging of colorectal cancer. Clin Radiol. 2021.
Edge SB, et al. AJCC cancer staging manual, vol. 7. New York: Springer; 2010.
Barral M, et al. Diffusion-weighted magnetic resonance imaging in colorectal cancer. J Visc Surg. 2016;153(5):361–9.
Scheenen TW, Zamecnik P. The role of magnetic resonance imaging in (future) cancer staging: note the nodes. Invest Radiol. 2021;56(1):42.
García-Figueiras R, et al. Advanced imaging of colorectal cancer: from anatomy to molecular imaging. Insights Imaging. 2016;7(3):285–309.
Mainenti PP, et al. Colorectal cancer: parametric evaluation of morphological, functional and molecular tomographic imaging. World J Gastroenterol. 2019;25(35):5233.
Maffione AM, et al. Is It Time to introduce PET/CT in colon cancer guidelines? Clin Nucl Med. 2020;45(7):525–30.
Lee DH, Lee JM. Whole-body PET/MRI for colorectal cancer staging: Is it the way forward? J Magn Reson Imaging. 2017;45(1):21–35.
Salameh J-P, et al. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): explanation, elaboration, and checklist. Bmj. 2020;370.
Higgins JP, et al. Cochrane handbook for systematic reviews of interventions. 2019: John Wiley & Sons.
Dwamena B. MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. 2009.
Harbord RM, Whiting P. Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. Stand Genomic Sci. 2009;9(2):211–29.
Mirshahvalad SA, Chavoshi M, Hekmat S. Diagnostic performance of prone-only myocardial perfusion imaging versus coronary angiography in the detection of coronary artery disease: a systematic review and meta-analysis. J Nucl Cardiol. 2022;29(3):1339–51.
Amorim BJ, et al. Clinical impact of PET/MR in treated colorectal cancer patients. Eur J Nucl Med Mol Imaging. 2019;46(11):2260–9.
Brendle C, et al. Assessment of metastatic colorectal cancer with hybrid imaging: comparison of reading performance using different combinations of anatomical and functional imaging techniques in PET/MRI and PET/CT in a short case series. Eur J Nucl Med Mol Imaging. 2016;43(1):123–32.
Catalano OA, et al. Colorectal cancer staging: comparison of whole-body PET/CT and PET/MR. Abdominal Radiology. 2017;42(4):1141–51.
Catalano OA, et al. Improving staging of rectal cancer in the pelvis: the role of PET/MRI. Eur J Nucl Med Mol Imaging. 2021;48(4):1235–45.
Crimì F, et al. 18F-FDG PET/MRI for rectal cancer TNM restaging after preoperative chemoradiotherapy: initial experience. Dis Colon Rectum. 2020;63(3):310–8.
Ferri V, et al. Quantitative analysis of 18-FDG-PET/MRI to assess pathological complete response following neoadjuvant radiochemotherapy in locally advanced rectal cancer. A prospective preliminary study. Acta Oncologica. 2019;58(9):1246–9.
Furtado FS, et al. Clinical impact of PET/MRI in oligometastatic colorectal cancer. Br J Cancer. 2021;125(7):975–82.
Kam MH, et al. Comparison of magnetic resonance imaging-fluorodeoxyglucose positron emission tomography fusion with pathological staging in rectal cancer. Br J Surg. 2010;97(2):266–8.
Kang B, et al. Added value of integrated whole-body PET/MRI for evaluation of colorectal cancer: comparison with contrast-enhanced MDCT. Am J Roentgenol. 2016;206(1):W10–20.
Lee SJ, et al. Clinical performance of whole-body 18F-FDG PET/Dixon-VIBE, T1-weighted, and T2-weighted MRI protocol in colorectal cancer. Clin Nucl Med. 2015;40(8):e392–8.
Lee DH, et al. Colorectal cancer liver metastases: diagnostic performance and prognostic value of pet/mr imaging. Radiology. 2016;280(3):782–92.
Li Y, et al. 18 f-fdg pet/mr versus mr alone in whole-body primary staging and restaging of patients with rectal cancer: what is the benefit of pet? J Clin Med. 2020;9(10):1–11.
Paspulati RM, et al. Comparison of hybrid FDG PET/MRI compared with PET/CT in colorectal cancer staging and restaging: a pilot study. Abdom Imaging. 2015;40(6):1415–25.
Plodeck V, et al. FDG-PET/MRI in patients with pelvic recurrence of rectal cancer: first clinical experiences. Eur Radiol. 2019;29(1):422–8.
Plodeck V, et al. Diagnostic performance of 18F-fluorodeoxyglucose-PET/MRI versus MRI alone in the diagnosis of pelvic recurrence of rectal cancer. Abdominal Radiology. 2021;46(11):5086–94.
Queiroz MA, et al. Diagnostic accuracy of FDG-PET/MRI versus pelvic MRI and thoracic and abdominal CT for detecting synchronous distant metastases in rectal cancer patients. Eur J Nucl Med Mol Imaging. 2021;48(1):186–95.
Yoon JH, et al. Initial M staging of rectal cancer: FDG PET/MRI with a hepatocyte-specific contrast agent versus contrast-enhanced CT. Radiology. 2020;294(2):310–9.
Zhou N, et al. The value of 18F-FDG PET/CT and abdominal PET/MRI as a one-stop protocol in patients with potentially resectable colorectal liver metastases. Frontiers in oncology. 2021;11.
Page MJ, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Benson AB, et al. Colon cancer, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2021;19(3):329–59.
Fraum TJ, Fowler KJ, McConathy J. PET/MRI: emerging clinical applications in oncology. Acad Radiol. 2016;23(2):220–36.
Crimì F, et al. [18F]FDG PET/MRI in rectal cancer. Ann Nucl Med. 2021;35(3):281–90.
Spick C, Herrmann K, Czernin J. 18F-FDG PET/CT and PET/MRI perform equally well in cancer: evidence from studies on more than 2,300 patients. J Nucl Med. 2016;57(3):420–30.
Al-Nabhani KZ, et al. Qualitative and quantitative comparison of PET/CT and PET/MR imaging in clinical practice. J Nucl Med. 2014;55(1):88–94.
Bailey JJ, et al. Does extended PET acquisition in PET/MRI rectal cancer staging improve results? Am J Roentgenol. 2018;211(4):896–900.
Beiderwellen KJ, et al. Simultaneous 68Ga-DOTATOC PET/MRI in patients with gastroenteropancreatic neuroendocrine tumors: initial results. Invest Radiol. 2013;48(5):273–9.
García-Figueiras R, et al. Advanced imaging techniques in evaluation of colorectal cancer. Radiographics. 2018;38(3):740–65.
Beets-Tan RG, Oyen WJ, Valentini V. Imaging and interventional radiology for radiation oncology. 2020;Springer.
Colosio A, et al. Value of diffusion-weighted and gadolinium-enhanced MRI for the diagnosis of pelvic recurrence from colorectal cancer. J Magn Reson Imaging. 2014;40(2):306–13.
Colosio A, et al. Local colorectal cancer recurrence: pelvic MRI evaluation. Abdom Imaging. 2013;38(1):72–81.
Liu L, et al. Correlation of MRI-detected extramural vascular invasion with regional lymph node metastasis in rectal cancer. Clin Imaging. 2016;40(3):456–60.
Wei M-Z, Zhao Z-H, Wang J-Y. The diagnostic accuracy of magnetic resonance imaging in restaging of rectal cancer after preoperative chemoradiotherapy: a meta-analysis and systematic review. J Comput Assist Tomogr. 2020;44(1):102–10.
Fraum TJ, et al. PET/MRI for gastrointestinal imaging: current clinical status and future prospects. Gastroenterol Clin North Am. 2018;47(3):691–714.
Lu Y-Y, et al. A systematic review and meta-analysis of pretherapeutic lymph node staging of colorectal cancer by 18F-FDG PET or PET/CT. Nucl Med Commun. 2012;33(11):1127–33.
Li XT, et al. Evaluating local lymph node metastasis with magnetic resonance imaging, endoluminal ultrasound and computed tomography in rectal cancer: a meta-analysis. Colorectal Dis. 2015;17(6):O129–35.
Soussan M, et al. Comparison of FDG-PET/CT and MR with diffusion-weighted imaging for assessing peritoneal carcinomatosis from gastrointestinal malignancy. Eur Radiol. 2012;22(7):1479–87.
Niekel MC, Bipat S, Stoker J. Diagnostic imaging of colorectal liver metastases with CT, MR imaging, FDG PET, and/or FDG PET/CT: a meta-analysis of prospective studies including patients who have not previously undergone treatment. Radiology. 2010;257(3):674–84.
Choi SH, et al. Diagnostic performance of CT, gadoxetate disodium-enhanced MRI, and PET/CT for the diagnosis of colorectal liver metastasis: systematic review and meta-analysis. J Magn Reson Imaging. 2018;47(5):1237–50.
Tsili AC, et al. Imaging of colorectal cancer liver metastases using contrast-enhanced US, multidetector CT, MRI, and FDG PET/CT: a meta-analysis. Acta Radiol. 2021;62(3):302–12.
Maffione AM, et al. Diagnostic accuracy and impact on management of 18 F-FDG PET and PET/CT in colorectal liver metastasis: a meta-analysis and systematic review. Eur J Nucl Med Mol Imaging. 2015;42(1):152–63.
Donati OF, et al. Value of retrospective fusion of PET and MR images in detection of hepatic metastases: comparison with F-18-FDG PET/CT and Gd-EOB-DTPA-enhanced MRI. J Nucl Med. 2010;51(5):692–9.
Zhang L, et al. Diagnostic performance of contrast-enhanced ultrasound and magnetic resonance imaging for detecting colorectal liver metastases: a systematic review and meta-analysis. Dig Liver Dis. 2019;51(9):1241–8.
Chung WS, et al. Comparison of gadoxetic acid-enhanced dynamic imaging and diffusion-weighted imaging for the preoperative evaluation of colorectal liver metastases. J Magn Reson Imaging. 2011;34(2):345–53.
Macera A, et al. Staging of colorectal liver metastases after preoperative chemotherapy. Diffusion-weighted imaging in combination with Gd-EOB-DTPA MRI sequences increases sensitivity and diagnostic accuracy. Eur Radiol. 2013;23(3):739–47.
Li X-T, et al. Evaluating rectal tumor staging with magnetic resonance imaging, computed tomography, and endoluminal ultrasound: a meta-analysis. Medicine. 2016;95(44).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
Patrick Veit-Haibach has received travel support and IIS grants from Siemens Healthineers in the last 3 years outside of this work. Ur Metser is advisor for POINT.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology—Digestive tract.
Rights and permissions
About this article
Cite this article
Mirshahvalad, S.A., Hinzpeter, R., Kohan, A. et al. Diagnostic performance of [18F]-FDG PET/MR in evaluating colorectal cancer: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 49, 4205–4217 (2022). https://doi.org/10.1007/s00259-022-05871-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-022-05871-0