Abstract
Background
Recently, a new disease phenotype characterized by supra-normal left ventricular ejection fraction (snLVEF) has been suggested, based on large datasets demonstrating an increased all-cause mortality in individuals with an LVEF > 65%. The underlying mechanisms of this association are currently unknown.
Methods
A total of 1367 patients (352 women, mean age 63.1 ± 11.6 years) underwent clinically indicated rest/adenosine stress ECG-gated 13N-ammonia positron emission tomography (PET) between 1995 and 2017 at our institution. All patients were categorized according to LVEF. A subcohort of 698 patients (150 women) were followed for major adverse cardiac events (MACEs), a composite of cardiac death, non-fatal myocardial infarction, cardiac-related hospitalization, and revascularization.
Results
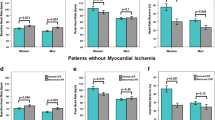
The prevalence of a snLVEF (≥ 65%) was higher in women as compared to that in men (31.3% vs 18.8%, p < 0.001). In women, a significant reduction in coronary flow reserve (CFR, p < 0.001 vs normal LVEF) and a blunted heart rate reserve (% HRR, p = 0.004 vs normal LVEF) during pharmacological stress testing—a surrogate marker for autonomic dysregulation—were associated with snLVEF. Accordingly, reduced CFR and HRR were identified as strong and independent predictors for snLVEF in women in a fully adjusted multinomial regression analysis. After a median follow-up time of 5.6 years, women with snLVEF experienced more often a MACE than women with normal (55–65%) LVEF (log rank p < 0.001), while such correlation was absent in men (log rank p = 0.76).
Conclusion
snLVEF is associated with an increased risk of MACE in women, but not in men. Microvascular dysfunction and an increased sympathetic tone in women may account for this association.




Similar content being viewed by others
Data availability statement
The dataset generated and analyzed during this study is available from the corresponding author on reasonable request.
References
Wehner GJ, Jing L, Haggerty CM, Suever JD, Leader JB, Hartzel DN, et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz550.
Ng ACT, Bax JJ. Hyperdynamic left ventricular function and the prognostic implications for heart failure with preserved ejection fraction. Eur Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz706.
Koch SE, Haworth KJ, Robbins N, Smith MA, Lather N, Anjak A, et al. Age- and gender-related changes in ventricular performance in wild-type FVB/N mice as evaluated by conventional and vector velocity echocardiography imaging: a retrospective study. Ultrasound Med Biol. 2013;39(11):2034–43. https://doi.org/10.1016/j.ultrasmedbio.2013.04.002.
Gebhard C, Stahli BE, Gebhard CE, Tasnady H, Zihler D, Wischnewsky MB, et al. Age- and gender-dependent left ventricular remodeling. Echocardiography. 2013;30(10):1143–50. https://doi.org/10.1111/echo.12264.
Gebhard C, Buechel RR, Stahli BE, Gransar H, Achenbach S, Berman DS, et al. Impact of age and sex on left ventricular function determined by coronary computed tomographic angiography: results from the prospective multicentre CONFIRM study. Eur Heart J Cardiovasc Imaging. 2017;18(9):990–1000. https://doi.org/10.1093/ehjci/jew142.
Gebhard C, Stahli BE, Gebhard CE, Fiechter M, Fuchs TA, Stehli J, et al. Gender- and age-related differences in rest and post-stress left ventricular cardiac function determined by gated SPECT. Int J Cardiovasc Imaging. 2014;30(6):1191–9. https://doi.org/10.1007/s10554-014-0431-y.
Chung AK, Das SR, Leonard D, Peshock RM, Kazi F, Abdullah SM, et al. Women have higher left ventricular ejection fractions than men independent of differences in left ventricular volume: the Dallas Heart Study. Circulation. 2006;113(12):1597–604. https://doi.org/10.1161/circulationaha.105.574400.
Gebhard C, Maredziak M, Messerli M, Buechel RR, Lin F, Gransar H, et al. Increased long-term mortality in women with high left ventricular ejection fraction: data from the CONFIRM (COronary CTAngiography EvaluatioN For Clinical Outcomes: an InteRnational Multicenter) Long-Term Registry. Eur Heart J Cardiovasc Imaging. 2019; 2020;21(4):363–374. https://doi.org/10.1093/ehjci/jez321.
Saab FA, Steg PG, Avezum A, Lopez-Sendon J, Anderson FA, Huang W, et al. Can an elderly woman’s heart be too strong? Increased mortality with high versus normal ejection fraction after an acute coronary syndrome. The Global Registry of Acute Coronary Events. Am Heart J. 2010;160(5):849–54. https://doi.org/10.1016/j.ahj.2010.07.018.
Montorsi P, Fabbiocchi F, Loaldi A, Annoni L, Polese A, De Cesare N, et al. Coronary adrenergic hyperreactivity in patients with syndrome X and abnormal electrocardiogram at rest. Am J Cardiol. 1991;68(17):1698–703.
Burger IA, Lohmann C, Messerli M, Bengs S, Becker A, Maredziak M, et al. Age- and sex-dependent changes in sympathetic activity of the left ventricular apex assessed by 18F-DOPA PET imaging. PLoS One. 2018;13(8):e0202302. https://doi.org/10.1371/journal.pone.0202302.
Hogarth AJ, Graham LN, Mary DA, Greenwood JP. Gender differences in sympathetic neural activation following uncomplicated acute myocardial infarction. Eur Heart J. 2009;30(14):1764–70. https://doi.org/10.1093/eurheartj/ehp188.
Mitoff PR, Gam D, Ivanov J, Al-hesayen A, Azevedo ER, Newton GE, et al. Cardiac-specific sympathetic activation in men and women with and without heart failure. Heart. 2011;97(5):382–7. https://doi.org/10.1136/hrt.2010.199760.
Fiechter M, Gebhard C, Ghadri JR, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Myocardial perfusion imaging with 13N-ammonia PET is a strong predictor for outcome. Int J Cardiol. 2013;167(3):1023–6. https://doi.org/10.1016/j.ijcard.2012.03.076.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54(2):150–6. https://doi.org/10.1016/j.jacc.2009.02.069.
Gebhard C, Fiechter M, Herzog BA, Lohmann C, Bengs S, Treyer V, et al. Sex differences in the long-term prognostic value of (13)N-ammonia myocardial perfusion positron emission tomography. Eur J Nucl Med Mol Imaging. 2018. https://doi.org/10.1007/s00259-018-4046-8.
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation. 2009;119(22):e561–87. https://doi.org/10.1161/circulationaha.109.192519.
Khorsand A, Graf S, Eidherr H, Wadsak W, Kletter K, Sochor H, et al. Gated cardiac 13N-NH3 PET for assessment of left ventricular volumes, mass, and ejection fraction: comparison with electrocardiography-gated 18F-FDG PET. J Nucl Med. 2005;46(12):2009–13.
Okazawa H, Takahashi M, Hata T, Sugimoto K, Kishibe Y, Tsuji T. Quantitative evaluation of myocardial blood flow and ejection fraction with a single dose of (13)NH(3) and gated PET. J Nucl Med. 2002;43(8):999–1005.
Slomka PJ, Alexanderson E, Jácome R, Jiménez M, Romero E, Meave A, et al. Comparison of clinical tools for measurements of regional stress and rest myocardial blood flow assessed with 13N-ammonia PET/CT. J Nucl Med. 2012;53(2):171–81. https://doi.org/10.2967/jnumed.111.095398.
DeGrado TR, Hanson MW, Turkington TG, Delong DM, Brezinski DA, Vallée JP, et al. Estimation of myocardial blood flow for longitudinal studies with 13N-labeled ammonia and positron emission tomography. J Nucl Cardiol. 1996;3(6 Pt 1):494–507. https://doi.org/10.1016/s1071-3581(96)90059-8.
Choi Y, Huang SC, Hawkins RA, Kim JY, Kim BT, Hoh CK, et al. Quantification of myocardial blood flow using 13N-ammonia and PET: comparison of tracer models. J Nucl Med. 1999;40(6):1045–55.
Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124(20):2215–24. https://doi.org/10.1161/circulationaha.111.050427.
Kanayama S, Matsunari I, Hirayama A, Kitayama M, Matsudaira M, Yoneyama T, et al. Assessment of global and regional left ventricular function by electrocardiographic gated N-13 ammonia positron emission tomography in patients with coronary artery disease. Circ J. 2005;69(2):177–82. https://doi.org/10.1253/circj.69.177.
Paonessa JR, Brennan T, Pimentel M, Steinhaus D, Feng M, Celi LA. Hyperdynamic left ventricular ejection fraction in the intensive care unit. Crit Care (London, England). 2015;19:288. https://doi.org/10.1186/s13054-015-1012-8.
Bahrami H, McConnell M, Heidenreich P. High left ventricular ejection fraction is associated with worse outcomes in patients with and without heart failure. J Am Coll Cardiol. 2014;63(12 Supplement):A732. https://doi.org/10.1016/S0735-1097(14)60732-4.
Bravo PE, Di Carli MF, Dorbala S. Role of PET to evaluate coronary microvascular dysfunction in non-ischemic cardiomyopathies. Heart Fail Rev. 2017;22(4):455–64. https://doi.org/10.1007/s10741-017-9628-1.
Phelps ME. Positron emission tomography provides molecular imaging of biological processes. Proc Natl Acad Sci U S A. 2000;97(16):9226–33.
Nakazato R, Berman DS, Alexanderson E, Slomka P. Myocardial perfusion imaging with PET. Imaging Med. 2013;5(1):35–46. https://doi.org/10.2217/iim.13.1.
Anversa P, Palackal T, Sonnenblick EH, Olivetti G, Meggs LG, Capasso JM. Myocyte cell loss and myocyte cellular hyperplasia in the hypertrophied aging rat heart. Circ Res. 1990;67(4):871–85.
Olivetti G, Giordano G, Corradi D, Melissari M, Lagrasta C, Gambert SR, et al. Gender differences and aging: effects on the human heart. J Am Coll Cardiol. 1995;26(4):1068–79. https://doi.org/10.1016/0735-1097(95)00282-8.
Zhang XP, Vatner SF, Shen YT, Rossi F, Tian Y, Peppas A, et al. Increased apoptosis and myocyte enlargement with decreased cardiac mass; distinctive features of the aging male, but not female, monkey heart. J Mol Cell Cardiol. 2007;43(4):487–91. https://doi.org/10.1016/j.yjmcc.2007.07.048.
Howlett SE. Age-associated changes in excitation-contraction coupling are more prominent in ventricular myocytes from male rats than in myocytes from female rats. Am J Physiol Heart Circ Physiol. 2010;298(2):H659–70. https://doi.org/10.1152/ajpheart.00214.2009.
Liao Y, Cooper RS, Mensah GA, McGee DL. Left ventricular hypertrophy has a greater impact on survival in women than in men. Circulation. 1995;92(4):805–10.
Liu CC, Kuo TB, Yang CC. Effects of estrogen on gender-related autonomic differences in humans. Am J Physiol Heart Circ Physiol. 2003;285(5):H2188–93. https://doi.org/10.1152/ajpheart.00256.2003.
Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, et al. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373(10):929–38. https://doi.org/10.1056/NEJMoa1406761.
Bravo PE, Hage FG, Woodham RM, Heo J, Iskandrian AE. Heart rate response to adenosine in patients with diabetes mellitus and normal myocardial perfusion imaging. Am J Cardiol. 2008;102(8):1103–6. https://doi.org/10.1016/j.amjcard.2008.06.021.
Conradson TB, Clarke B, Dixon CM, Dalton RN, Barnes PJ. Effects of adenosine on autonomic control of heart rate in man. Acta Physiol Scand. 1987;131(4):525–31. https://doi.org/10.1111/j.1748-1716.1987.tb08272.x.
Hage FG, Heo J, Franks B, Belardinelli L, Blackburn B, Wang W, et al. Differences in heart rate response to adenosine and regadenoson in patients with and without diabetes mellitus. Am Heart J. 2009;157(4):771–6. https://doi.org/10.1016/j.ahj.2009.01.011.
Hage FG, Perry G, Heo J, Iskandrian AE. Blunting of the heart rate response to adenosine and regadenoson in relation to hyperglycemia and the metabolic syndrome. Am J Cardiol. 2010;105(6):839–43. https://doi.org/10.1016/j.amjcard.2009.11.042.
Abidov A, Hachamovitch R, Hayes SW, Ng CK, Cohen I, Friedman JD, et al. Prognostic impact of hemodynamic response to adenosine in patients older than age 55 years undergoing vasodilator stress myocardial perfusion study. Circulation. 2003;107(23):2894–9. https://doi.org/10.1161/01.cir.0000072770.27332.75.
Hage FG, Dean P, Iqbal F, Heo J, Iskandrian AE. A blunted heart rate response to regadenoson is an independent prognostic indicator in patients undergoing myocardial perfusion imaging. J Nucl Cardiol. 2011;18(6):1086–94. https://doi.org/10.1007/s12350-011-9429-1.
Gebhard CE, Maredziak M, Portmann A, Bengs S, Haider A, Fiechter M, et al. Heart rate reserve is a long-term risk predictor in women undergoing myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2019.
Kaski JC. Cardiac syndrome X in women: the role of oestrogen deficiency. Heart. 2006;92(Suppl 3):iii5–9. https://doi.org/10.1136/hrt.2005.070318.
Gulli G, Cemin R, Pancera P, Menegatti G, Vassanelli C, Cevese A. Evidence of parasympathetic impairment in some patients with cardiac syndrome X. Cardiovasc Res. 2001;52(2):208–16.
Crea F, Bairey Merz CN, Beltrame JF, Kaski JC, Ogawa H, Ong P, et al. The parallel tales of microvascular angina and heart failure with preserved ejection fraction: a paradigm shift. Eur Heart J. 2017;38(7):473–7. https://doi.org/10.1093/eurheartj/ehw461.
Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol. 1999;33(7):1948–55.
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20. https://doi.org/10.1056/NEJMoa1908655.
Funding
CG was supported by grants from the Swiss National Science Foundation (SNSF); the Olga Mayenfisch Foundation, Switzerland; the OPO Foundation, Switzerland; the Novartis Foundation, Switzerland; the Swiss Heart Foundation; the Helmut Horten Foundation, Switzerland; the EMDO Foundation, Switzerland; the Iten-Kohaut Foundation, Switzerland; and the University Hospital Zurich Foundation. SB was supported by the University of Zurich (UZH) Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have the following to disclose: the University Hospital of Zurich holds a research contract with GE Healthcare. CG has received research grants from the Novartis Foundation, Switzerland.
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The study was approved by the local ethics committee (BASEC No. 2017–01112). The need for informed written consent was waived by the ethics committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology
Rights and permissions
About this article
Cite this article
Maredziak, M., Bengs, S., Portmann, A. et al. Microvascular dysfunction and sympathetic hyperactivity in women with supra-normal left ventricular ejection fraction (snLVEF). Eur J Nucl Med Mol Imaging 47, 3094–3106 (2020). https://doi.org/10.1007/s00259-020-04892-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04892-x