Abstract
Purpose
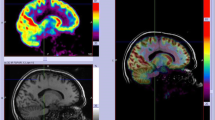
This study aims to evaluate the performance of 18F-FDG PET for distinguishing the epileptogenic zone (EZ) from propagation and non-involved zones at brain area level, as defined using stereo-EEG (SEEG), in patients with pharmacoresistant epilepsy due to malformations of cortical development (MCD). Additionally, we seek to determine the relationship between 18F-FDG-PET data and post-surgical seizure outcome.
Methods
Thirty-eight patients with MCD were explored with 18F-FDG PET and SEEG. We compared PET metabolism of each patient to a control population of healthy subjects. Based on MRI and SEEG, we separated 4 distinct zones at individual level: lesional, epileptogenic non-lesional, propagation, and non-involved. Then, we analysed (1) difference of PET metabolism within these four distinct zones; (2) performance of PET in defining the EZ within the SEEG-sampled areas; and (3) relation between extension of PET hypometabolism and post-surgical seizure outcome.
Results
We found (1) a gradient of PET hypometabolism from non-involved to propagation, then to epileptogenic and lesional zones (p < 0.001); (2) good performance of PET in defining the EZ (AUC of ROC curve = 0.82); (3) poorer post-surgical prognosis associated with PET hypometabolism extension beyond SEEG sampling (p = 0.024).
Conclusion
18F-FDG-PET has good accuracy in determining EZ in patients with MCD even if the hypometabolism is not limited to the EZ. Furthermore, hypometabolic extension is unfavourably associated with post-surgical prognosis.





Similar content being viewed by others
References
Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CGCGCG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. 2017;377:1648–56.
Cloppenborg T, May TW, Blümcke I, Grewe P, Hopf LJ, Kalbhenn T, et al. Trends in epilepsy surgery: stable surgical numbers despite increasing presurgical volumes. J Neurol Neurosurg Psychiatry. 2016:1–8.
Baud MO, Perneger T, Attila R. European trends in epilepsy surgery. Neurology. 2018:1–12.
Guerrini R, Duchowny M, Jayakar P, Krsek P, Kahane P, Tassi L, et al. Diagnostic methods and treatment options for focal cortical dysplasia. Epilepsia. 2015;56:1669–86.
Rowland NC, Englot DJ, Cage TA, Sughrue ME, Barbaro NM, Chang EF. A meta-analysis of predictors of seizure freedom in the surgical management of focal cortical dysplasia. J Neurosurg. 2012;116:1035–41.
Faramand AM, Barnes N, Harrison S, Gunny R, Jacques T, Tahir ZM, et al. Seizure and cognitive outcomes after resection of glioneuronal tumors in children. Epilepsia. 2017:1–9.
Englot DJ, Berger MS, Barbaro NM, Chang EF. Factors associated with seizure freedom in the surgical resection of glioneuronal tumors. Epilepsia. 2012;53:51–7.
Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74.
Giulioni M, Marucci G, Pelliccia V, Gozzo F, Barba C, Didato G, et al. Epilepsy surgery of “low grade epilepsy associated neuroepithelial tumors”: a retrospective nationwide Italian study. Epilepsia. 2017:1–10.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. Springer Berlin Heidelberg. 2016;131:803–20.
Isnard J, Taussig D, Bartolomei F, Bourdillon P, Catenoix H, Chassoux F, et al. French guidelines on stereoelectroencephalography (SEEG). Elsevier Masson SAS: Neurophysiol Clin; 2017.
Salamon N, Kung J, Shaw SJ, Koo J, Koh S, Wu JY, et al. FDG-PET/MRI coregistration improves detection of cortical dysplasia in patients with epilepsy. Neurology. 2008;71:1594–601.
Chassoux F, Landré E, Mellerio C, Turak B, Mann MW, Daumas-Duport C, et al. Type II focal cortical dysplasia: electroclinical phenotype and surgical outcome related to imaging. Epilepsia. 2012;53:349–58.
Desarnaud S, Mellerio C, Semah F, Laurent A, Landre E, Devaux B, et al. 18F-FDG PET in drug-resistant epilepsy due to focal cortical dysplasia type 2: additional value of electroclinical data and coregistration with MRI (European Journal of Nuclear Medicine and Molecular Imaging, (2018), 45, 8, (1449-1460), 10. Eur J Nucl Med Mol Imaging 2018;45:1465.
Rubí S, Setoain X, Donaire A, Bargalló N, Sanmartí F, Carreño M, et al. Validation of FDG-PET/MRI coregistration in nonlesional refractory childhood epilepsy. Epilepsia. 2011;52:2216–24.
Lee SK, Choe G, Hong KS, Nam HW, Kim JY, Chung CK, et al. Neuroimaging findings of cortical dyslamination with cytomegaly. Epilepsia. 2001;42:850–6.
Chugani HT, Shields WD, Shewmon DA, Olson DM, Phelps ME, Peacock WJ. Infantile spasms: I. PET identifies focal cortical dysgenesis in cryptogenic cases for surgical treatment. Ann Neurol. 1990;27:406–13.
Kim YK, Lee DS, Lee SK, Chung CK, Chung J-K, Lee MC. (18)F-FDG PET in localization of frontal lobe epilepsy: comparison of visual and SPM analysis. J Nucl Med. 2002;43:1167–74.
Kim YH, Kang HC, Kim DS, Kim SH, Shim KW, Kim HDH, et al. Neuroimaging in identifying focal cortical dysplasia and prognostic factors in pediatric and adolescent epilepsy surgery. Epilepsia. 2011;52:722–7.
Casse R, Rowe CCCC, Newton M, Berlangieri SUSU, Scott AMAM. Positron emission tomography and positron emission. Mol Imaging Biol. 2004;6:72–3.
Kudr M, Krsek P, Marusic P, Tomasek M, Trnka J, Michalova K, et al. SISCOM and FDG-PET in patients with non-lesional extratemporal epilepsy: correlation with intracranial EEG, histology, and seizure outcome. Epileptic Disord. 2013;15:3–13.
Juhász C, Chugani DC, Muzik O, Watson C, Shah J, Shah A, et al. Is epileptogenic cortex truly hypometabolic on interictal positron emission tomography? Ann Neurol. 2000;48:88–96.
Lamarche F, Job AS, Deman P, Bhattacharjee M, Hoffmann D, Gallazzini-Crépin C, et al. Correlation of FDG-PET hypometabolism and SEEG epileptogenicity mapping in patients with drug-resistant focal epilepsy. Epilepsia. 2016;57:2045–55.
Alkonyi B, Juhász C, Muzik O, Asano E, Saporta A, Shah A, et al. Quantitative brain surface mapping of an electrophysiologic/metabolic mismatch in human neocortical epilepsy. Epilepsy Res. 2009;87:77–87.
Aubert S, Wendling F, Regis J, McGonigal A, Figarella-Branger D, Peragut JC, et al. Local and remote epileptogenicity in focal cortical dysplasias and neurodevelopmental tumours. Brain. 2009;132:3072–86.
Lagarde S, Bonini F, McGonigal A, Chauvel P, Gavaret M, Scavarda D, et al. Seizure-onset patterns in focal cortical dysplasia and neurodevelopmental tumors: relationship with surgical prognosis and neuropathologic subtypes. Epilepsia. 2016;57:1426–35.
Jayakar P, Gotman J, Harvey AS, Palmini A, Tassi L, Schomer D, et al. Diagnostic utility of invasive EEG for epilepsy surgery: indications, modalities, and techniques. Epilepsia. 2016;57:1735–47.
Engel J. Update on surgical treatment of the epilepsies. Summary of the Second International Palm Desert Conference on the Surgical Treatment of the Epilepsies (1992). Neurology. 1993;43:1612–7.
Lagarde S, Roehri N, Lambert I, Trebuchon A, McGonigal A, Carron R, et al. Interictal stereotactic-EEG functional connectivity in refractory focal epilepsies. Brain. 2018:1–15.
Medina Villalon S, Paz R, Roehri N, Lagarde S, Pizzo F, Colombet B, et al. EpiTools, A software suite for presurgical brain mapping in epilepsy: intracerebral EEG. J Neurosci Methods. Elsevier B.V. 2018;303:7–15.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89.
Besson P, Bandt SKK, Proix T, Lagarde S, Jirsa VK, Ranjeva J-PJ-P, et al. Anatomic consistencies across epilepsies: a stereotactic-EEG informed high-resolution structural connectivity study. Brain. 2017;140.
Bartolomei F, Chauvel P, Wendling F. Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain. 2008;131:1818–30.
Proix T, Bartolomei F, Guye M, Jirsa VK. Individual brain structure and modelling predict seizure propagation. Brain. 2017;140:641–54.
Lieberman MD, Cunningham WA. Type I and type II error concerns in fMRI research: re-balancing the scale. Soc Cogn Affect Neurosci. 2009.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J. 2005.
Perkins NJ, Schisterman EF. The Youden index and the optimal cut-point corrected for measurement error. Biom J. 2005.
Chassoux F, Rodrigo S, Semah F, Beuvon F, Landre E, Devaux B, et al. FDG-PET improves surgical outcome in negative MRI Taylor-type focal cortical dysplasias. Neurology. 2010;75:2168–75.
Hong SB, Han HJ, Roh SY, Seo DW, Kim SE, Kim MH. Hypometabolism and interictal spikes during positron emission tomography scanning in temporal lobe epilepsy. Eur Neurol. 2002;48:65–70.
Juhasz C, Chugani DC, Muzik O, Watson C, Shah J, Shah A, et al. Electroclinical correlates of flumazenil and fluorodeoxyglucose PET abnormalities in lesional epilepsy. Neurology. 2000;55:825–35.
Tepmongkol S, Srikijvilaikul T, Vasavid P. Factors affecting bilateral temporal lobe hypometabolism on 18F-FDG PET brain scan in unilateral medial temporal lobe epilepsy. Epilepsy Behav. Elsevier Inc. 2013;29:386–9.
Hong SJ, Bernhardt BC, Schrader DS, Bernasconi N, Bernasconi A. Whole-brain MRI phenotyping in dysplasia-related frontal lobe epilepsy. Neurology. 2016;86:643–50.
Hong SJ, Lee HM, Gill R, Crane J, Sziklas V, Bernhardt BC, et al. A connectome-based mechanistic model of focal cortical dysplasia. Brain. 2019;142:688–99.
Krsek P, Maton B, Korman B, Pacheco-Jacome E, Jayakar P, Dunoyer C, et al. Different features of histopathological subtypes of pediatric focal cortical dysplasia. Ann Neurol. 2008;63:758–69.
Chassoux F, Artiges E, Semah F, Laurent A, Landré E, Turak B, et al. 18 F-FDG-PET patterns of surgical success and failure in mesial temporal lobe epilepsy. Neurology. 2017;88:1045–53.
Cahill V, Sinclair B, Malpas CB, McIntosh AM, Chen Z, Vivash LE, et al. Metabolic patterns and seizure outcomes following anterior temporal lobectomy. Ann Neurol. 2019:1–10.
Higo T, Sugano H, Nakajima M, Karagiozov K, Iimura Y, Suzuki M, et al. The predictive value of FDG-PET with 3D-SSP for surgical outcomes in patients with temporal lobe epilepsy. Seizure BEA Trading Ltd. 2016;41:127–33.
Wong CH, Bleasel A, Wen L, Eberl S, Byth K, Fulham M, et al. Relationship between preoperative hypometabolism and surgical outcome in neocortical epilepsy surgery. Epilepsia. 2012;53:1333–40.
Besson P, Dinkelacker V, Valabregue R, Thivard L, Leclerc X, Baulac M, et al. Structural connectivity differences in left and right temporal lobe epilepsy. Neuroimage. Elsevier Inc. 2014;100:135–44.
Keller SS, Glenn GR, Weber B, Kreilkamp BAK, Jensen JH, Helpern JA, et al. Preoperative automated fibre quantification predicts postoperative seizure outcome in temporal lobe epilepsy. Brain. 2017;140:68–82.
Baker NL, Nesland T, Drane DL, Bonilha L, Breedlove J, Lin JJ, et al. The brain connectome as a personalized biomarker of seizure outcomes after temporal lobectomy the brain connectome as a personalized biomarker of seizure outcomes after temporal lobectomy. Neurology. 2015:1–8.
He X, Doucet GE, Pustina D, Sperling MR, Sharan AD, Tracy JI. Presurgical thalamic hubness predicts surgical outcome in temporal lobe epilepsy. Neurology. 2017;88:2285–93.
Bonilha L, Nesland T, Martz GU, Joseph JE, Spampinato MV, Edwards JC, et al. Medial temporal lobe epilepsy is associated with neuronal fibre loss and paradoxical increase in structural connectivity of limbic structures. J Neurol Neurosurg Psychiatry. 2012;83:903–9.
Bonilha L, Helpern JA, Sainju R, Nesland T, Edwards JC, Glazier SS, et al. Presurgical connectome and postsurgical seizure control in temporal lobe epilepsy. Neurology. 2013;81:1704–10.
Bernhardt BC, Hong S, Bernasconi A, Bernasconi N. Imaging structural and functional brain networks in temporal lobe epilepsy. Front Hum Neurosci. 2013;7:1–14.
Halac G, Delil S, Zafer D, Isler C, Uzan M, Comunoglu N, et al. Compatibility of MRI and FDG-PET findings with histopathological results in patients with focal cortical dysplasia. Seizure. 2017;45:80–6.
Acknowledgements
We thank Prof. Figarella-Branger for the reviewing of histological data. We thank Prof. Patrick Chauvel, Prof. Martine Gavaret, Dr. Francesca Bonini, Dr. Lisa Vaugier, Dr. Francesca Pizzo, Dr. Sandrine Aubert, Dr. Geraldine Daquin, Dr. Nathalie Villeneuve and Dr. Anne Lepine (Marseille), for the clinical management of some included patients. We thank Prof. Henry Dufour for surgical procedures and Prof. Jean Régis for SEEG procedures, in some of the selected patients.
Funding
This work has been carried out within the FHU EPINEXT and DHU-Imaging with the support of the A*MIDEX project (ANR-11-IDEX-0001-02) funded by the “Investissements d’Avenir” French Government program managed by the French National Research Agency (ANR). Part of this work was funded by a joint Agence Nationale de la Recherche (ANR) and Direction Génerale de l’Offre de Santé (DGOS) under grant “VIBRATIONS” ANR-13-PRTS-0011-01.
Author information
Authors and Affiliations
Contributions
Stanislas Lagarde, Fabrice Bartolomei and Eric Guedj participated in the Conceptualization and the Methodology of this study.
Stanislas Lagarde, Mohamed Boucekine, Laurent Boyer, Agnes Trebuchon, Romain Carron, Didier Scavarda, Mahtieu Milh, Aileen McGonigal, Fabrice Bartolomei and Eric Guedj participated in the Investigation and the Formal analysis.
Stanislas Lagarde, Mohamed Boucekine, Laurent Boyer, Agnes Trebuchon, Romain Carron, Didier Scavarda, Mahtieu Milh, Aileen McGonigal, Fabrice Bartolomei and Eric Guedj participated in the writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (French Institute of Health (IRB15226)) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurology
Rights and permissions
About this article
Cite this article
Lagarde, S., Boucekine, M., McGonigal, A. et al. Relationship between PET metabolism and SEEG epileptogenicity in focal lesional epilepsy. Eur J Nucl Med Mol Imaging 47, 3130–3142 (2020). https://doi.org/10.1007/s00259-020-04791-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04791-1