Abstract
Purpose
Precise determination of neuroendocrine tumor (NET) disease status and response to therapy remains a rate-limiting concern for disease management. This reflects limitations in biomarker specificity and resolution capacity of imaging. In order to evaluate biomarker precision and identify if combinatorial blood molecular markers and imaging could provide added diagnostic value, we assessed the concordance between 68Ga-somatostatin analog (SSA) positron emission tomography (PET), circulating NET gene transcripts (NETest), chromogranin A (CgA), and Ki-67 in NETs.
Methods
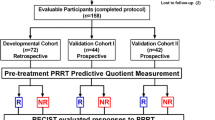
We utilized two independent patient groups with positive 68Ga-SSA PET: data set 1 (68Ga-SSA PETs undertaken for peptide receptor radionuclide therapy (PRRT), as primary or salvage treatment, n = 27) and data set 2 (68Ga-SSA PETs performed in patients referred for initial disease staging or restaging after various therapies, n = 22). We examined the maximum standardized uptake value (SUVmax), circulating gene transcripts, CgA levels, and baseline Ki-67. Regression analyses, generalized linear modeling, and receiver-operating characteristic (ROC) analyses were undertaken to determine the strength of the relationships.
Results
SUVmax measured in two centers were mathematically evaluated (regression modeling) and determined to be comparable. Of 49 patients, 47 (96 %) exhibited a positive NETest. Twenty-six (54 %) had elevated CgA (χ2 = 20.1, p < 2.5×10−6). The majority (78 %) had Ki-67 < 20 %. Gene transcript scores were predictive of imaging with >95 % concordance and significantly correlated with SUVmax (R 2 = 0.31, root-mean-square error = 9.4). The genes MORF4L2 and somatostatin receptors SSTR1, 3, and 5 exhibited the highest correlation with SUVmax. Progressive disease was identified by elevated levels of a quotient of MORF4L2 expression and SUVmax [ROC-derived AUC (R 2 = 0.7, p < 0.05)]. No statistical relationship was identified between CgA and Ki-67 and no relationship with imaging parameters was evident.
Conclusion
68Ga-SSA PET imaging parameters (SUVmax) correlated with a circulating NET transcript signature. Disease status could be predicted by an elevated quotient of gene expression (MORF4L2) and SUVmax. These observations provide the basis for further exploration of strategies that combine imaging parameters and disease-specific molecular data for the improvement of NET management.





Similar content being viewed by others
References
Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 2008;9(1):61–72. doi:10.1016/s1470-2045(07)70410-2.
Hallet J, Law CH, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer 2015;121(4):589–97. doi:10.1002/cncr.29099.
Kanakis G, Kaltsas G. Biochemical markers for gastroenteropancreatic neuroendocrine tumours (GEP-NETs). Best Pract Res Clin Gastroenterol 2012;26(6):791–802. doi:10.1016/j.bpg.2012.12.006.
Kulke MH, Siu LL, Tepper JE, Fisher G, Jaffe D, Haller DG, et al. Future directions in the treatment of neuroendocrine tumors: consensus report of the National Cancer Institute Neuroendocrine Tumor clinical trials planning meeting. J Clin Oncol Off 2011;29(7):934–43. doi:10.1200/jco.2010.33.2056.
Modlin IM, Moss SF, Chung DC, Jensen RT, Snyderwine E. Priorities for improving the management of gastroenteropancreatic neuroendocrine tumors. J Natl Cancer Inst 2008;100(18):1282–9. doi:10.1093/jnci/djn275.
de Mestier L, Dromain C, d’Assignies G, Scoazec JY, Lassau N, Lebtahi R, et al. Evaluating neuroendocrine tumors progression and therapeutic response: state of the art. Endocr Relat Cancer 2013;18:18.
Sundin A, Rockall A. Therapeutic monitoring of gastroenteropancreatic neuroendocrine tumors: the challenges ahead. Neuroendocrinology 2012;96(4):261–71. doi:10.1159/000342270.
Castaño JP, Sundin A, Maecke HR, Villabona C, Vazquez-Albertino R, Navarro E, et al. Gastrointestinal neuroendocrine tumors (NETs): new diagnostic and therapeutic challenges. Cancer Metastasis Rev 2014;33:353–9. doi:10.1007/s10555-013-9465-1.
Faivre S, Ronot M, Dreyer C, Serrate C, Hentic O, Bouattour M, et al. Imaging response in neuroendocrine tumors treated with targeted therapies: the experience of sunitinib. Target Oncol 2012;7(2):127–33. doi:10.1007/s11523-012-0216-y.
Toumpanakis C, Kim MK, Rinke A, Bergestuen DS, Thirlwell C, Khan MS, et al. Combination of cross-sectional and molecular imaging studies in the localization of gastroenteropancreatic neuroendocrine tumors. Neuroendocrinology 2014;99:63–74.
Bodei L, Kidd M, Prasad V, Baum RP, Drozdov I, Modlin IM. The future of nuclear medicine imaging of neuroendocrine tumors: on a clear day one might see forever. Eur J Nucl Med Mol Imaging 2014;41:2189–93. doi:10.1007/s00259-014-2836-1.
Modlin I, Drozdov I, Alaimo D, Callahan S, Teixeira N, Bodei L, et al. A multianalyte PCR blood test outperforms single analyte ELISAs (chromogranin A, pancreastatin, neurokinin A) for neuroendocrine tumor detection. Endocr Relat Cancer 2014;21:615–28.
Rindi G, Petrone G, Inzani F. The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol 2014;25(2):186–92. doi:10.1007/s12022-014-9313-z.
Yang Z, Tang LH, Klimstra DS. Gastroenteropancreatic neuroendocrine neoplasms: historical context and current issues. Semin Diagn Pathol 2013;30(3):186–96. doi:10.1053/j.semdp.2013.06.005.
Modlin IM, Gustafsson BI, Pavel M, Svejda B, Lawrence B, Kidd M. A nomogram to assess small-intestinal neuroendocrine tumor (‘carcinoid’) survival. Neuroendocrinology 2010;92(3):143–57. doi:10.1159/000319784.
Modlin IM, Drozdov I, Kidd M. The identification of gut neuroendocrine tumor disease by multiple synchronous transcript analysis in blood. PLoS One 2013;8(5):e63364. doi:10.1371/journal.pone.0063364.
Modlin I, Drozdov I, Kidd M. A multitranscript blood neuroendocrine tumor molecular signature to identify treatment efficacy and disease progress. J Clin Oncol 2013;31(Suppl):abstract 4137.
Modlin I, Drozdov I, Kidd M. Gut neuroendocrine tumor blood qPCR fingerprint assay: characteristics and reproducibility. Clin Chem Lab Med 2014;52(3):419–29.
Giandomenico V, Modlin IM, Ponten F, Nilsson M, Landegren U, Bergqvist J, et al. Improving the diagnosis and management of neuroendocrine tumors: utilizing new advances in biomarker and molecular imaging science. Neuroendocrinology 2013;98(1):16–30. doi:10.1159/000348832.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5(6):649–55.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45(2):228–47. doi:10.1016/j.ejca.2008.10.026.
Virgolini I, Ambrosini V, Bomanji JB, Baum RP, Fanti S, Gabriel M, et al. Procedure guidelines for PET/CT tumour imaging with 68Ga-DOTA-conjugated peptides: 68Ga-DOTA-TOC, 68Ga-DOTA-NOC, 68Ga-DOTA-TATE. Eur J Nucl Med Mol Imaging 2010;37(10):2004–10. doi:10.1007/s00259-010-1512-3.
Baum RP, Kulkarni HR. THERANOSTICS: from molecular imaging using Ga-68 labeled tracers and PET/CT to personalized radionuclide therapy - the Bad Berka experience. Theranostics 2012;2(5):437–47. doi:10.7150/thno.3645.
Rindi G, Klimstra DS, Arnold R, Kloppel G, Bosman FT, Komminoth P, et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of the digestive system. 4th ed. Lyon: International Agency for Research on Cancer; 2010.
Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC. Pathology and genetics of tumours of the lung, pleura, thymus and heart. 2004.
Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw 2010;33(1):1–22.
Kuhn M. Building predictive models in R using the caret package. J Stat Softw 2008;28(5):1–26.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982;143(1):29–36.
Treglia G, Castaldi P, Rindi G, Giordano A, Rufini V. Diagnostic performance of gallium-68 somatostatin receptor PET and PET/CT in patients with thoracic and gastroenteropancreatic neuroendocrine tumours: a meta-analysis. Endocrine 2012;42(1):80–7. doi:10.1007/s12020-012-9631-1.
Ruf J, Schiefer J, Kropf S, Furth C, Ulrich G, Kosiek O, et al. Quantification in Ga-DOTA(0)-Phe(1)-Tyr(3)-octreotide positron emission tomography/computed tomography: can we be impartial about partial volume effects? Neuroendocrinology 2013;97(4):369–74. doi:10.1159/000350418.
Campana D, Ambrosini V, Pezzilli R, Fanti S, Labate AM, Santini D, et al. Standardized uptake values of (68)Ga-DOTANOC PET: a promising prognostic tool in neuroendocrine tumors. J Nucl Med 2010;51(3):353–9. doi:10.2967/jnumed.109.066662.
Haug AR, Auernhammer CJ, Wängler B, Schmidt GP, Uebleis C, Göke B, et al. 68Ga-DOTATATE PET/CT for the early prediction of response to somatostatin receptor-mediated radionuclide therapy in patients with well-differentiated neuroendocrine tumors. J Nucl Med 2010;51(9):1349–56. doi:10.2967/jnumed.110.075002.
Sharma P, Naswa N, Kc SS, Alvarado LA, Dwivedi AK, Yadav Y, et al. Comparison of the prognostic values of 68Ga-DOTANOC PET/CT and 18F-FDG PET/CT in patients with well-differentiated neuroendocrine tumor. Eur J Nucl Med Mol Imaging 2014;41:2194–202.
Kwekkeboom DJ, Kam BL, van Essen M, Teunissen JJ, van Eijck CH, Valkema R, et al. Somatostatin-receptor-based imaging and therapy of gastroenteropancreatic neuroendocrine tumors. Endoc Relat Cancer 2010;17(1):R53–73. doi:10.1677/erc-09-0078.
Walenkamp A, Crespo G, Fierro Maya F, Fossmark R, Igaz P, Rinke A, et al. Hallmarks of gastrointestinal neuroendocrine tumours: implications for treatment. Endocr Relat Cancer 2014;21(6):R445–60. doi:10.1530/erc-14-0106.
Kaemmerer D, Peter L, Lupp A, Schulz S, Sänger J, Prasad V, et al. Molecular imaging with (68)Ga-SSTR PET/CT and correlation to immunohistochemistry of somatostatin receptors in neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2011;38(9):1659–68. doi:10.1007/s00259-011-1846-5.
Corleto VD, Nasoni S, Panzuto F, Cassetta S, Delle Fave G. Somatostatin receptor subtypes: basic pharmacology and tissue distribution. Dig Liver Dis 2004;36 Suppl 1:S8–16.
Velikyan I, Sundin A, Sörensen J, Lubberink M, Sandström M, Garske-Román U, et al. Quantitative and qualitative intrapatient comparison of 68Ga-DOTATOC and 68Ga-DOTATATE: net uptake rate for accurate quantification. J Nucl Med 2014;55(2):204–10. doi:10.2967/jnumed.113.126177.
Scheibe M, Arnoult N, Kappei D, Buchholz F, Decottignies A, Butter F, et al. Quantitative interaction screen of telomeric repeat-containing RNA reveals novel TERRA regulators. Genome Res 2013;23(12):2149–57. doi:10.1101/gr.151878.112. Epub 2013 Aug 6.
Marinoni I, Kurrer AS, Vassella E, Dettmer M, Rudolph T, Banz V, et al. Loss of DAXX and ATRX are associated with chromosome instability and reduced survival of patients with pancreatic neuroendocrine tumors. Gastroenterology 2014;146(2):453–60. doi:10.1053/j.gastro.2013.10.020.
Kayani I, Bomanji JB, Groves A, Conway G, Gacinovic S, Win T, et al. Functional imaging of neuroendocrine tumors with combined PET/CT using 68Ga-DOTATATE (DOTA-DPhe1, Tyr3-octreotate) and 18F-FDG. Cancer 2008;112(11):2447–55. doi:10.1002/cncr.23469.
Ezziddin S, Lohmar J, Yong-Hing CJ, Sabet A, Ahmadzadehfar H, Kukuk G, et al. Does the pretherapeutic tumor SUV in 68Ga DOTATOC PET predict the absorbed dose of 177Lu octreotate? Clin Nucl Med 2012;37(6):e141–7. doi:10.1097/RLU.0b013e31823926e5.
Lindholm DP, Oberg K. Biomarkers and molecular imaging in gastroenteropancreatic neuroendocrine tumors. Horm Metab Res 2011;43(12):832–7. doi:10.1055/s-0031-1287794.
Jakobsen AM, Andersson P, Saglik G, Andersson E, Kölby L, Erickson JD, et al. Differential expression of vesicular monoamine transporter (VMAT) 1 and 2 in gastrointestinal endocrine tumours. J Pathol 2001;195(4):463–72.
Rozenblatt-Rosen O, Hughes CM, Nannepaga SJ, Shanmugam KS, Copeland TD, Guszczynski T, et al. The parafibromin tumor suppressor protein is part of a human Paf1 complex. Mol Cell Biol 2005;25(2):612–20.
Öberg K, Knigge U, Kwekkeboom D, Perren A. Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2012;23(Suppl 7):vii124–30.
Compliance with ethical standards
Conflicts of interest
None.
Research involving human participants and/or animals
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
L. Bodei and M. Kidd contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Principal competent analysis (A) and hierarchical clustering (B) of information from 68Ga-DOTATOC and 68Ga-DOTANOC scanned patients. Scanned values from DOTANOC were identified as outliers and were not statistically comparable from values for DOTANOC-scanned patients. DIM dimension, D600 and DLS are different scanners used for DOTATOC (GIF 368 kb)
Rights and permissions
About this article
Cite this article
Bodei, L., Kidd, M., Modlin, I.M. et al. Gene transcript analysis blood values correlate with 68Ga-DOTA-somatostatin analog (SSA) PET/CT imaging in neuroendocrine tumors and can define disease status. Eur J Nucl Med Mol Imaging 42, 1341–1352 (2015). https://doi.org/10.1007/s00259-015-3075-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-015-3075-9