Abstract
Purpose
Gastroesophageal reflux (GER) is very common in pre-term infants. The diagnosis based on symptoms is always questionable. The incidence of GER in symptomatic babies varies from 22% to 85%, but literature regarding the incidence of reflux in asymptomatic pre-term infants is lacking. We used radionuclide scintigraphy to evaluate the incidence of GER in symptomatic as well as asymptomatic pre-term neonates and to assess whether symptoms have any relation with positive scintigraphy.
Methods
We studied 106 pre-term infants (52 symptomatic, 54 asymptomatic) of less than 34 weeks of gestation, who fulfilled the eligibility criteria. Babies were considered symptomatic in the presence of vomiting, regurgitation, apnea, de-saturations, unexplained bradycardia and recurrent lung collapses. Radionuclide scintigraphy was conducted at post-conceptional age of 32–34 weeks when they were clinically stable for 72 h. Feeding was avoided for 2 h preceding the study. 99mTc sulphur colloid was administered in a dose of 1.85 MBq (0.05 mCi) in 1 ml, followed by milk (full feed) through an orogastric tube, prior to imaging under a gamma camera. Reflux was graded as low or high, and reflux episodes during the study were counted.
Results
The incidence of GER in the symptomatic group was 71.2% and in asymptomatic babies 61.1% (p = 0.275). High-grade reflux was more common (71.4%) than low-grade (28.6%) in both groups (p = 0.449). Mean number of reflux episodes in 20 min was 4.4 ± 2.4 in symptomatic babies and 4.9 ± 2.2 in asymptomatic babies (p = 0.321). Babies with positive scintigraphy were similar in birth weight, gestation, time to achieve full feeds, weight and age at discharge to those with negative scintigraphy.
Conclusions
GER is common in pre-term infants of less than 34 weeks gestation. The incidence of positive scintigraphy and grade of reflux is not significantly different in symptomatic vs. asymptomatic babies. Though radionuclide scintigraphy is a simple, quick and non-invasive investigation in suspected cases of GER, positive scintigraphy has no correlation with symptoms.
Similar content being viewed by others
Introduction
Gastroesophageal reflux (GER) is a common condition in pre-term infants. The condition is physiological in most of these infants and has a self-limiting course. However, the symptoms of GER could vary from vomiting, regurgitation, recurrent apnea and de-saturations to none. The significance of these symptoms in the diagnosis of GER and the best method to detect GER are controversial. The incidence of GER in symptomatic patients has been quoted as 22% to 85% [1–4]. This wide variation in incidence may be attributed to different methods and criteria used for the diagnosis of GER. Most of these methods are not comparable with each other because of different methods to detect GER by different pathophysiologic mechanisms. GER is also very common in asymptomatic pre-term infants, but literature regarding its incidence in asymptomatic babies is scanty.
In most of the previous studies, investigators have used 24-h oesophageal pH monitoring for the diagnosis of GER [1, 2, 5–9]. This method detects only acid reflux. In pre-term infants, most of the reflux episodes are post-prandial non-acid refluxes, which are not detected by 24-h oesophageal pH monitoring. In addition, this investigation is invasive and needs patient admission to the hospital, and the presence of the probe in the oesophagus may itself alter the GER.
Among other modes of diagnosis, barium oesophagogram is outdated because of its low sensitivity and high dose of irradiation during the study [10–12]. Its only utility in infants is to evaluate anatomical abnormalities like oesophageal fistula and strictures.
Multiple intra-luminal impedance is a recent technique for the diagnosis of GER [13]. This technique evaluates oesophageal bolus transit and reflux in a manner similar to the barium study but without the hazards of radiation exposure. The limitations of the impedance method include the lack of universal availability, complexity of interpretation and invasiveness.
Radionuclide scintigraphy is a simple, highly physiological, sensitive [14, 15] non-invasive test [10] for the detection of GER. The sensitivity of radionuclide scintigraphy is reported to be between 75% and 100% [10, 14, 16]. The standard to which it has been compared is either acid reflux or prolonged pH monitoring of the oesophagus and in one study histopathology [16]. The specificity of scintigraphy is between 81.2% and 100% [10]. Scintigraphy allows the quantification of reflux and calculation of gastric emptying time and oesophageal clearance time, detects both acid and non-acid reflux and allows prolonged and repeated observation and possibly absolute correlation between reflux and aspiration. While radionuclide scintigraphy is a good screening test for the detection of GER, it is not yet standardized in pre-term infants. We therefore planned this study to find out the incidence of GER in symptomatic vs. asymptomatic babies using radionuclide scintigraphy and also to see whether the symptoms usually attributed to GER have any relation with positive scintigraphy.
Materials and methods
This prospective study was conducted by the division of neonatology, department of paediatrics in collaboration with the department of nuclear medicine, Post-Graduate Institute of Medical Education and Research, Chandigarh, India, over a period of 14 months. The study was approved by the Institute Research Ethics Committee, and written informed consent was obtained from all parents before conducting the scintigraphic study.
Inclusion criteria
The study included:
-
1.
Pre-term neonates of less than 34 weeks gestation
-
2.
Neonates with regurgitation, vomiting, apnoea, recurrent de-saturations (spO2 < 85%), unexplained bradycardia (<100 per minute) and recurrent lung collapses (twice or more) were considered symptomatic
-
3.
Babies without the above symptoms were in the asymptomatic group
Exclusion criteria
The exclusion criteria of the study were:
-
1.
Babies with major life-threatening congenital malformations
-
2.
Babies on a ventilator
Pre-term neonates of less than 34 weeks of gestation were enrolled soon after birth, on arrival to the neonatal intensive care and special care nursery. These babies were prospectively followed up for development of any symptoms suggestive of GER. Relevant maternal and neonatal details were recorded in a structured proforma. All neonatal illnesses and medications likely to affect GER were noted. Details of feeding like onset and method of feeding, amount of feed and achievement of full feeds were also recorded. In those with symptoms suggestive of GER, the details of symptoms were recorded.
Radionuclide scintigraphy was performed when the babies reached a post-conceptional age (PCA) of 32–34 weeks and were stable for at least 72 h prior to the study (defined as babies on full feeds (150–180 ml kg−1 day−1), FiO2 requirement of less than 30%, respiratory rate of not more than 60 to 80 per minute and heart rate of 120 to 160 per minute).
Medications like aminophylline, metoclopramide, domperidone and erythromycin, known to affect GER, were stopped at least 3 days before the scintigraphic study. The babies were kept nil orally for 2 h prior to scintigraphy and shifted to the nuclear medicine department in a transport incubator. 99mTc-sulphur colloid (1.85 MBq [0.05 mCi] in 1 ml) was administered through an orogastric tube followed by the amount of feed the baby was receiving on that day through the same tube. The tube was then removed after closing the outer end to avoid contamination of the oesophagus and oropharynx with the radionuclide solution. The babies were placed in the supine position inside the incubator under the gamma camera (Millennium MPR, GE Medical systems, Milwaukee, USA), and sequential images were acquired for a total duration of 20 min at the rate of 15 s per frame in a 128 × 128 matrix (total 80 frames in 20 min). The camera was positioned close to the top surface of the incubator, so that the distance between the infants’ chest and the collimator surface was not more than 12 cm in any study. At the end of the acquisition period, a radionuclide marker was positioned at the level of oral cavity. A single static image was also acquired for 30 s in a 128 × 128 matrix immediately after the dynamic phase of the study. No sedation was used during the procedure. The images were stored on an online computer and subsequently assessed independently by two experienced nuclear medicine physicians for any retrograde movement of radiotracer into the oesophagus.
Clear visualization of retrograde movement of tracer from the stomach into the oesophagus in at least one image during the 20-min study was labelled as positive for GER. Reflux was graded as low grade when observed in the lower half of the oesophagus and high grade if it reached the upper oesophagus and/or oropharynx. We used only two grades of GER because of the short length of the oesophagus in pre-term infants. The number of episodes of reflux during the 20 min of study was also counted and recorded.
Statistical analysis
The incidence of GER in symptomatic and asymptomatic pre-term infants was compared using the Chi-square test. All categorical variables were analysed by using the Chi-square test. Mann–Whitney U test was used for analysing the skewed data and Student’s t test for the normally distributed data. Only one variable (amount of feed) was normally distributed, and all other continuous variables had skewed distribution. Logistic regression was applied to see the association of GER with the symptoms like vomiting, regurgitation, apnoea, dips in saturation, recurrent lung collapse and feeding characteristics like amount of feed and duration of tube feed.
Results
The study included 106 pre-term infants of less than 34 weeks of gestation, of which 52 were symptomatic (35 male, 17 female) and 54 asymptomatic (29 male, 25 female) for GER. Mean gestation at birth was 30.5 ± 1.6 weeks, and the mean birth weight was 1,358 ± 294 g. Gestation and birth weight were significantly less in the symptomatic group (p < 0.001) compared to asymptomatic group (29.8 ± 1.5 vs. 31.2 ± 1.4 weeks and 1,250.5 ± 225.4 vs. 1,462 ± 316.8 g, respectively). Scintigraphy was performed at the median chronological age of 9 days in asymptomatic babies and 18.5 days in symptomatic babies. No adverse effects were observed in any of the patients following the scintigraphic study.
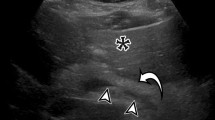
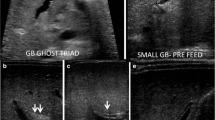
Scintigraphy was positive for GER in 61.1% of the asymptomatic pre-term infants and in 71.2% of the symptomatic pre-term infants; the difference is statistically not significant (p = 0.275; Fig. 1). High-grade reflux was the predominant grade of reflux in both the groups (71.4%) and present in 75.8% and 67.6% of infants in the asymptomatic and symptomatic groups, respectively. However, the difference between the two groups was statistically not significant (p = 0.449; Table 1). The mean number of reflux episodes during the 20-min study was 4.9 ± 2.2 in the asymptomatic group as compared to 4.4 ± 2.4 in the symptomatic group (p = 0.321). Low- and high-grade refluxes are shown in Figs. 2 and 3, respectively.
Table 2 depicts the incidence of positive scintigraphy in patients with suspected symptoms of GER. In the presence of vomiting, regurgitation, apnoea, dips in saturation and unexplained bradycardia, the incidence of positive scintigraphy were 73.7%, 73.3%, 66.7%, 65.4% and 66.75%, respectively, and those with the absence of these symptoms had positive scintigraphy in 69.7%, 68.2%, 84.6%, 76.9% and 71.7%, respectively. The difference was statistically not significant (p > 0.05). The distribution of grades of refluxes was also analysed in each symptom (Table 3). High-grade reflux was predominant when correlated to each symptom. There was only one pre-term infant with recurrent lung collapse and he showed high-grade reflux on scintigraphy.
We divided the babies into two groups: those with positive and those with negative scintigraphy. This was done to see whether any of the characteristics differed in these two groups. Table 4 depicts the comparison of characteristics at birth, at scintigraphy and at discharge between those in whom the study was positive and those in whom it was negative. There was no significant difference in any of the characteristics between these two groups (p > 0.05). The comparison of characteristics between the two groups of positive and negative scintigraphy was also done in sub-groups of symptomatic and asymptomatic groups. Weight, gestation and feeding details before the study, at the time of study and at the time of discharge were compared, and statistically, they were similar (p > 0.05).
The mean PCA (35.3 ± 2.04 weeks) and age at discharge (39.8 ± 17.29 days) were more in the symptomatic group, compared to asymptomatic group (33.6 ± 1.06 weeks and 17.5 ± 10.02 days, respectively), which was statistically significant (p < 0.001).
Discussion
GER is a common medical problem in pre-term neonates. However, the symptoms are very non-specific, and the ideal method of diagnosis is unclear. Though GER is considered to be a self-limiting condition, which improves with advancing gestational age, there is widespread concern about GER and the presence of symptoms. The treatment of GER is very controversial, and whether these babies need treatment is also unanswered.
In our study, using the radionuclide scintigraphic technique, all infants were imaged while they were inside the incubator, in consideration for the safety of the babies. Continuous monitoring of vital signs and maintenance of constant optimal body temperature were thus ensured throughout the scintigraphic procedure. We used a transport incubator for this purpose, which is smaller than the standard incubator used in the Neonatal Intensive Care Unit (NICU), and positioned the camera close to the surface of the incubator for the study. The distance of less than 12 cm between the infants’ chest and the collimator surface was sufficient to avoid any degradation in image quality at the dose of 1.85 MBq used in these small infants. Most standard protocols and guidelines on GER scintigraphy require a 60-min dynamic acquisition. However, as the babies imaged in this study were all pre-term infants, many with respiratory symptoms, the duration of the procedure was reduced to 20 min so as to minimize the time spent outside the NICU.
The incidence of GER in symptomatic and asymptomatic pre-term infants did not show any significant difference in our study. In spite of differences in weight, gestation and age, the PCA was similar in both the groups at the time of study. Previously, some studies have shown that symptomatic babies are of lesser gestation and weight than asymptomatic babies [1, 17–19]. It is therefore likely that symptoms attributed to GER are more commonly found in smaller babies.
Goyon et al. [20] also found a similar result. They used oesophageal pH monitoring to study GER in symptomatic and asymptomatic pre-term infants and found a high incidence of GER in pre-term infants, but there was no difference in the occurrence of GER in the symptomatic vis a vis asymptomatic group. The suspected symptoms of GER are therefore likely to be related to the other illnesses in these babies, rather than to the reflux.
The study conducted by Marino et al. [2] in 75 pre-term symptomatic infants using a two-channel pneumocardiogram and a 1-h oesophageal pH method found a 63% incidence of GER. This study was done at a PCA of 37–38 weeks. Latini et al. [21] studied 50 newborns with symptoms of apnoea, cyanosis and bradycardia using the scintigraphy method. Scintigraphy was positive in 40 infants, giving an incidence of 80%. Akinola et al. [6] studied 629 infants, born before 32 weeks of gestation, using extended pH monitoring and found an incidence of 63.5% in symptomatic pre-term infants. Tolia et al. [22] compared oesophageal pH-metry with gastroesophageal scintigraphy. In their study, the incidence of GER was 69.5% by pH-metry and 66.0% with gastroesophageal scintigraphy in symptomatic infants of less than 1 year of age. Newell et al. [1] studied 35 pre-term infants of 28 weeks gestation receiving intensive care by using oesophageal pH monitoring and found an incidence of 85%. However, while GER has been studied and found to occur in symptomatic pre-term infants, there is lack of data on the incidence of GER in the asymptomatic group.
We graded reflux into two grades, low and high, as the length of the oesophagus in the scintigraphic images was too small to identify three grades of reflux. Overall, high-grade reflux was found in 71.4% of babies with positive scintigraphy and was the predominant reflux detected when compared to low-grade reflux, which was detected in 28.6%. High-grade reflux was predominant in both asymptomatic and symptomatic pre-term infants. In symptomatic pre-term infants, the incidence of high-grade reflux was 67.6%, similar to that reported in various studies. We also found high-grade reflux in 75.8% of asymptomatic pre-term infants. High-grade reflux appears to have no relation with the occurrence of symptoms of GER. A study conducted by Skopnik et al. [13] showed that 75% of all the GERs detected by the intra-luminal impedance technique reached the pharyngeal space. In another study, James and Ewer [23] showed that the reflux reached the oropharyngeal cavity in 70% of the studied pre-term infants by demonstrating acid in the oropharyngeal secretions. Peter et al. [19], using the intra-luminal impedance method, found that 66% of refluxes in pre-term infants of 33 weeks PCA were of high grade. Lopez et al. [24] also found 79% of all refluxes reaching the proximal oesophagus in pre-term infants.
Lopez et al. [24] in their study by the intra-luminal impedance method found 281 reflux episodes during the 24-h study, averaging 3.9 reflux episodes per 20 min. In our study, the overall mean number of reflux episodes in those with positive scintigraphy (n = 70) were 4.67 ± 2.3 episodes in 20 min. The reflux episodes averaged 4.97 ± 2.2 in 20 min in the asymptomatic infants against 4.41 ± 2.4 episodes in the symptomatic group. This difference was not statistically significant (p = 0.321). This similarity in the number of reflux episodes may be a reflection of the comparable grades of GER in the two groups of infants.
When we analysed each symptom like vomiting, regurgitation, apnoea, dips in saturation, unexplained bradycardia and recurrent lung collapse separately, the results were similar to those with the absence of the particular symptom, with regards to the scintigraphy result and distribution of grades of refluxes.
We analysed positive and negative scintigraphic results and compared various characteristics between these two groups viz., gestation, weight, Apgar scores at birth, days taken to achieve full feeds, amount of feed, duration of tube feed, weight, PCA and age at scintigraphy and weight and PCA and age at discharge. There was no statistically significant difference in any of the characteristics between the two groups. Similarly, a separate analysis in asymptomatic and symptomatic groups showed no statistically significant difference in any of the above characteristics between those with positive scintigraphy and those with negative scintigraphy. This implies that the occurrence of GER in pre-term infants is probably physiological and has no relation with presence or absence of symptoms. Babies with positive or negative scintigraphy were similar with respect to weight, gestation at birth, days taken to achieve full feeds, amount of feed, duration of tube feeds and weight, age and PCA at discharge. Duration of hospital stay and PCA at discharge was higher in symptomatic babies probably due to smaller birth weight and gestation.
The findings of this study raise the question as to whether symptoms considered as manifestations of GER have any relevance and whether treatment based only on symptoms is justified. Radionuclide scintigraphy can be used as a safe, convenient and non-invasive modality to diagnose GER.
Conclusions
GER occurs very commonly (66%) in pre-term neonates of less than 34 weeks gestation. Occurrence of GER is not significantly different in symptomatic pre-term infants when compared to asymptomatic pre-term infants. High-grade reflux is more common in both groups, but the number of reflux episodes is similar. Infants with positive GER on scintigraphy behave similarly in all the characteristics when compared to those with negative scintigraphy. Radionuclide scintigraphy is simple, non-invasive, easy to perform and has no adverse effects in pre-term infants.
References
Newell SJ, Booth IW, Morgan ME, Durbin GM, McNeish AS. Gastroesophageal reflux in preterm infants. Arch Dis Child 1989;64:780–6.
Marino AJ, Assing E, Carbone MT, Hiatt IM, Hegyi T, Graff M. The incidence of gastroesophageal reflux in preterm infants. J Perinatol 1995;15:369–71.
Thomas EJ, Kumar R, Dasan JB, Chandrashekar N, Agarwala S, Tripathi M, et al. Radionuclide scintigraphy in the evaluation of gastroesophageal reflux in post-operative esophageal atresia and tracheoesophageal fistula patients. Nucl Med Commun 2003;24:317–20.
Dhillon AS, Ewer AK. Diagnosis and management of gastroesophageal reflux in preterm infants in neonatal intensive care units. Acta Pediatr 2004;93:88–93.
Kohelet D, Boaz M, Serour F, Cohen-Adad N, Arbel E, Gorenstein A. Esophageal pH study and symptomatology of gastroesophageal reflux in newborn infants. Am J Perinatol 2004;21:85–91.
Akinola E, Rosenkrantz TS, Pappagallo M, McKay K, Hussain N. Gastroesophageal reflux in < 32 week gestational age at birth: Lack of relationship to chronic lung disease. Am J Perinatol 2004;21:57–62.
Khalaf MN, Porat R, Brodsky NL, Bhandari V. Clinical correlations in infants in the neonatal intensive care unit with varying severity of gastroesophageal reflux. J Pediatr Gastroenterol Nutr 2001;32:45–9.
Mezzacappa MA, Goulart LM, Brunelli MM. The influence of the supine and prone positions in the esophageal pH monitoring in very low birth weight infants. Arq Gastroenterol 2004;41:42–8.
de Ajuriaguerra M, Radvanyi-Bouvet MF, Huon C, Moriette G. Gastroesophageal reflux and apnea in prematurely born infants during wakefulness and sleep. Am J Dis Child 1991;145:1132–6.
Sydney H. Gastric emptying, gastroesophageal reflux and esophageal motility. In: Michael JG, Stephen KT, editors. Effective use of computers in nuclear medicine. Practical clinical applications in the imaging laboratory. New York: McGraw-Hill; 1988. p. 412–33.
Sydney H. Gastroesophageal reflux, esophageal transit, gastric emptying and pulmonary aspiration. In: Treves ST, editor. Pediatric nuclear medicine. 2nd ed. New York: Springer; 1995. p. 430–52.
Aksglaede K, Pedersen JB, Lange A, Funch-Jensen P, Thommesen P. Gastroesophageal reflux demonstrated by radiography in infants less than 1 year of age. Comparison with pH monitoring. Acta Radiol 2003;44:136–8.
Skopnik H, Silny J, Heiber O, Schulz J, Rau G, Heimann G. Gastroesophageal reflux in infants: evaluation of a new intraluminal impedance technique. J Pediatr Gastroenterol Nutr 1996;23:591–8.
Gonzalez Fernandez F, Arguelles Martin F, Rodriguez de Quesada B, Gonzalez Hachero J, Valls Sanchez de Puerta A, Gentles M. Gastroesophageal scintigraphy: a useful screening test for gastroesophageal reflux. J Pediatr Gastroenterol Nutr 1987;6:217–9.
Tolia V, Kuhns L, Kauffman RE. Comparison of simultaneous esophageal pH monitoring and scintigraphy in infants with gastroesophageal reflux. Am J Gastroenterol 1993;88:661–4.
Kashyap R, Sharma R, Madan N, Sachdev G, Chopra MK, Chopra K. Evaluation of radionuclide gastroesophagographyas a suitable screening test for detection of gastroesophageal reflux. Indian Pediatr 1993;30:625–8.
Peter CS, Sprodowski N, Bohnhorst B, Silny J, Poets CF. Gastroesophageal reflux and apnea of prematurity: no temporal relationship. Pediatrics 2002;109:8–11.
Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying and gastroesophageal reflux in preterm infants. Arch Dis Child Fetal Neonatal Ed 1996;75:117–21.
Peter CS, Wiechers C, Bohnhorst B, Silny J, Poets CF. Influence of nasogastric tubes on gastroesophageal reflux in preterm infants: a multiple intraluminal impedance study. J Peditr 2002;141:277–9.
Goyon JB, Boggio V, Gillot I, Seigneur C. Esophageal pH monitoring in asymptomatic and symptomatic newborn infants. Arch Fr Pediatr 1988;45:237–41.
Latini G, Del Vecchio A, De Mitri B, Giannuzzi R, Presta G, Quartulli L, et al. Scintigraphic evaluation of gastroesophageal reflux in newborns. Pediatr Med Chir 1999;21:115–7.
Tolia V, Calhoun JA, Kuhns LR, Kauffman RE. Lack of correlation between extended pH monitoring and scintigraphy in the evaluation of infants with gastroesophageal reflux. J Lab Clin Med 1990;115:559–63.
James ME, Ewer AK. Acid oro-pharyngeal secretions can predict gastroesophageal reflux in preterm infants. Eur J Pediatr 1999;158:371–4.
Lopez Alonso M, Moya MJ, Cabo JA, Ribas J, Macais Mc, Silny J, et al. Acid and non acid gastroesophageal reflux in newborns. Preliminary results using intraluminal impedance. Cir Pediatr 2005;18:121–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morigeri, C., Bhattacharya, A., Mukhopadhyay, K. et al. Radionuclide scintigraphy in the evaluation of gastroesophageal reflux in symptomatic and asymptomatic pre-term infants. Eur J Nucl Med Mol Imaging 35, 1659–1665 (2008). https://doi.org/10.1007/s00259-008-0752-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-0752-y