Abstract
Purpose
We have now applied our MORF/cMORF pretargeting technology to the targeting of CWR22 prostate tumor in nude mice.
Methods
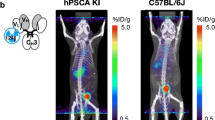
The antiTAG-72 antibody B72.3 was conjugated with an 18 mer MORF while the cMORF was radiolabeled with 99mTc. The specific binding of the antibody to the CWR22 cells was first confirmed in an assay placing the radiolabeled B72.3 antibody in competition with increasing concentrations of native B72.3. Thereafter, a group of four CWR22 tumored mice intravenously received the MORF-B72.3 and, 3 days later, the 99mTc-cMORF, and were killed at 3 h postradioactivity injection. The dosage of the labeled cMORF was selected on the basis of previous experience in LS174T tumored mice. As controls, four animals received only the radiolabeled cMORF and another four received only the 111In-B72.3. The maximum percent tumor accumulation (MPTA) of the labeled cMORF was subsequently determined by a dosage study of labeled cMORF. Both a multipinhole SPECT image and a planar gamma camera image were obtained of a representative mouse.
Results
The CWR22 tumor was confirmed to be TAG-72-positive. The MPTA of the labeled cMORF in the CWR22 tumor was 2.22%ID/g compared to only 0.12%ID/g in control mice without pretargeting. Both the planar and tomographic images confirmed the success of the CWR22 pretargeting.
Conclusions
The MORF/cMORF pretargeting approach has been successfully applied to tumor targeting of the prostate xenograft CWR22. However, the MPTA in this tumor model is lower than that in the LS174T tumor model investigated earlier, possibly due to a lower tumor blood supply.





Similar content being viewed by others
Reference
Karacay H, Brard PY, Sharkey RM, Chang CH, Rossi EA, McBride WJ, et al. Therapeutic advantage of pretargeted radioimmunotherapy using a recombinant bispecific antibody in a human colon cancer xenograft. Clin Cancer Res 2005;11:7879–85.
Sharkey RM, Cardillo TM, Rossi EA, Chang CH, Karacay H, McBride WJ, et al. Signal amplification in molecular imaging by pretargeting a multivalent, bispecific antibody. Nat Med 2005;11:1250–5.
Pagel JM, Hedin N, Subbiah K, Meyer D, Mallet R, Axworthy D, et al. Comparison of anti-CD20 and anti-CD45 antibodies for conventional and pretargeted radioimmunotherapy of B-cell lymphomas. Blood 2003;101:2340–8.
Subbiah K, Hamlin DK, Pagel JM, Wilbur DS, Meyer DL, Axworthy DB, et al. Comparison of immunoscintigraphy, efficacy, and toxicity of conventional and pretargeted radioimmunotherapy in CD20-expressing human lymphoma xenografts. J Nucl Med 2003;44:437–45.
Magnani P, Paganelli G, Modorati G, Zito F, Songini C, Sudati F, et al. Quantitative comparison of direct antibody labeling and tumor pretargeting in uveal melanoma. J Nucl Med 1996;37:967–71.
Sung C, van Osdol WW. Pharmacokinetic comparison of direct antibody targeting with pretargeting protocols based on streptavidin-biotin binding. J Nucl Med 1995;36:867–76.
Reardan DT, Meares CF, Goodwin DA, McTigue M, David GS, Stone MR, et al. Antibodies against metal chelates. Nature 1985;316 6025:265–8.
Goodwin DA, Meares CF, MnTigue M, et al. Rapid localization of haptens in sites containing previously administrated antibody for immunoscintigraphy with short half-life tracers [abstract]. J Nucl Med 1986;27:959 (suppl).
Hnatowich DJ, Virzi F, Rusckowski M. Investigations of avidin and biotin for imaging applications. J Nucl Med 1987;28:1294–302.
Liu G, Mang’era K, Liu N, Gupta S, Rusckowski M, Hnatowich DJ. Tumor pretargeting in mice using 99mTc-labeled morpholino, a DNA analog. J Nucl Med 2002;43:384–91.
Liu G, He J, Dou S, Gupta S, Vanderheyden JL, Rusckowski M, et al. Pretargeting in tumored mice with radiolabeled morpholino oligomer showing low kidney uptake. Eur J Nucl Med Mol Imaging 2004;31:417–24.
Liu G, He J, Dou S, Gupta S, Rusckowski M, Hnatowich DJ. Further investigations of morpholino pretargeting in mice—establishing quantitative relations in tumor. Eur J Nucl Med Mol Imaging 2005;32:1115–23.
Liu G, Dou S, He J, Liu X, Rusckowski M, Hnatowich DJ. Predicting the biodistribution of radiolabeled cMORF effector in MORF-pretargeted mice. Eur J Nucl Med Mol Imaging 2007;34:237–46
Scher HI, Buchanan G, Gerald W, Butler LM, Tilley WD. Targeting the androgen receptor: improving outcomes for castration-resistant prostate cancer. Endocr Relat Cancer 2004;11:459–76.
Miyamoto H, Messing EM. Androgen deprivation therapy for prostate cancer: current status and future prospects. Prostate 2004;61:332–53.
Nagabhushan M, Miller CM, Pretlow TP, Giaconia JM, Edgehouse NL, Schwartz S, et al. CWR22: the first human prostate cancer xenograft with strongly androgen-dependent and relapsed strains both in vivo and in soft agar. Cancer Res 1996;56:3042–6.
Mazur MT, Shultz JJ. Prostatic adenocarcinoma. Evaluation of immunoreactivity to monoclonal antibody B72.3. Am J Clin Pathol 1990;93:466–70.
Badalament RA, Burgers JK, Petty LR, Mojzisik CM, Berens A, Marsh W, et al. Radioimmunoguided radical prostatectomy and lymphadenectomy. Cancer 1993;71:2268–75.
Myers RB, Meredith RF, Schlom J, LoBuglio AF, Bueschen AJ, Wheeler RH, et al. Tumor associated glycoprotein-72 is highly expressed in prostatic adenocarcinomas. J Urol 1994;152:243–6.
Myers RB, Schlom J, Srivastava S, Grizzle WE. Expression of tumor-associated glycoprotein 72 in prostatic intraepithelial neoplasia and prostatic adenocarcinoma. Mod Pathol 1995;8:260–5.
Meredith RF, Bueschen AJ, Khazaeli MB, Plott WE, Grizzle WE, Wheeler RH, et al. Treatment of metastatic prostate carcinoma with radiolabeled antibody CC49. J Nucl Med 1994;35:1017–22.
Brenner PC, Rettig WJ, Sanz-Moncasi MP, Reuter V, Aprikian A, Old LJ, et al. TAG-72 expression in primary, metastatic and hormonally treated prostate cancer as defined by monoclonal antibody CC49. J Urol 1995;153:1575–9.
Thor A, Gorstein F, Ohuchi N, Szpak CA, Johnston WW, Schlom J. Tumor-associated glycoprotein (TAG-72) in ovarian carcinomas defined by monoclonal antibody B72.3. J Natl Cancer Inst 1986;76:995–1006.
Thor A, Ohuchi N, Szpak CA, Johnston WW, Schlom J. Distribution of oncofetal antigen tumor-associated glycoprotein-72 defined by monoclonal antibody B72.3. Cancer Res 1986;46:3118–24.
Loy TS, Nashelsky MB. Reactivity of B72.3 with adenocarcinomas. An immunohistochemical study of 476 cases. Cancer 1993;72:2495–8.
Starling JJ, Maciak RS, Law KL, Hinson NA, Briggs SL, Laguzza BC, et al. In vivo antitumor activity of a monoclonal antibody-Vinca alkaloid immunoconjugate directed against a solid tumor membrane antigen characterized by heterogeneous expression and noninternalization of antibody–antigen complexes. Cancer Res 1991;51:2965–72.
Winnard P Jr, Chang F, Rusckowski M, Mardirossian G, Hnatowich DJ. Preparation and use of NHS-MAG3 for technetium-99m labeling of DNA. Nucl Med Biol 1997;24:425–32.
Liu G, Dou S, He J, Yin D, Gupta S, Zhang S, et al. Radiolabeling of MAG3-morpholino oligomers with 188Re at high labeling efficiency and specific radioactivity for tumor pretargeting. Appl Radiat Isot 2006;64:971–8.
He J, Liu G, Dou S, Gupta S, Rusckowski M, Hnatowich DJ. An improved method for covalently conjugating morpholino oligomers to antitumor antibodies. Bioconjug Chem 2007;18:983–8.
Zou JX, Zhong Z, Shi XB, Tepper CG, deVere White RW, Kung HJ, et al. ACTR/AIB1/SRC-3 and androgen receptor control prostate cancer cell proliferation and tumor growth through direct control of cell cycle genes. Prostate 2006;66:1474–86.
van Schaijk FG, Oosterwijk E, Molkenboer-Kuenen JD, Soede AC, McBride BJ, Goldenberg DM, et al. Pretargeting with bispecific anti-renal cell carcinoma x anti-DTPA (In) antibody in 3 RCC models. J Nucl Med 2005;46:495–501.
van Schaijk FG, Broekema M, Oosterwijk E, van Eerd JE, McBride BJ, Goldenberg DM, et al. Residualizing iodine markedly improved tumor targeting using bispecific antibody-based pretargeting. J Nucl Med 2005;46:1016–22.
Agus DB, Golde DW, Sgouros G, Ballangrud A, Cordon-Cardo C, Scher HI. Positron emission tomography of a human prostate cancer xenograft: association of changes in deoxyglucose accumulation with other measures of outcome following androgen withdrawal. Cancer Res 1998;58:3009–14.
Oyama N, Kim J, Jones LA, Mercer NM, Engelbach JA, Sharp TL, et al. MicroPET assessment of androgenic control of glucose and acetate uptake in the rat prostate and a prostate cancer tumor model. Nucl Med Biol 2002;29:783–90.
Oyama N, Ponde DE, Dence C, Kim J, Tai YC, Welch MJ. Monitoring of therapy in androgen-dependent prostate tumor model by measuring tumor proliferation. J Nucl Med 2004;45:519–25.
Chen X, Park R, Hou Y, Tohme M, Shahinian AH, Bading JR, et al. MicroPET and autoradiographic imaging of GRP receptor expression with 64Cu-DOTA-[Lys3]bombesin in human prostate adenocarcinoma xenografts. J Nucl Med 2004;45:1390–7.
Acknowledgements
The authors are grateful to Dr. Pretlow (Case Western Reserve University School of Medicine, Cleveland, OH, USA) for the CWR22 tumor cells, to Dr. Aurigemma (NCI BRB Preclinical Repository, Rockville, MD, USA) for the B72.3 antibody, and to Dr. Shayne Squires for helping with the tumor model development. Financial support was provided in part by NIH (CA107360 and CA94994).
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support: CA107360 and CA94994.
Appendix
Appendix
If we define a space containing the whole tumor, the amount of labeled effector dQ (ng) accumulated in tumor in an infinitely short period of time dt is:
where F is the cardiac output in grams of blood per second (g/s), f is the blood fraction flowing into tumor, E is the trapping efficiency, i.e., the fraction of the effector reaching the tumor that is retained, and C is the blood concentration of the effector in nanograms of effector per gram of blood (ng/g). Given that the F and f are constants for a given tumor model (i.e., animal, tumor type, location, and tumor size), the total tumor accumulation Q over the entire period from administration to the complete clearance of free effector will be:
Dividing both sides of the equation by the injected dosage of effector (ng) and the tumor weight W and multiplying by 100, the accumulation of effector now in percent of injected dosage per gram of tumor (%ID/g) becomes:
As described earlier and verified experimentally [12, 13], Q is a constant when the dosage of effector is below that required to saturate the MORF-antibody in the tumor. Because the product F × f × W −1 is also constant, the integral \( {\int\limits_{t = 0}^{t = \infty } {E \times C{\left( {{{\text{\% ID}}} \mathord{\left/ {\vphantom {{{\text{\% ID}}} {\text{g}}}} \right. \kern-\nulldelimiterspace} {\text{g}}} \right)}_{{{\text{blood}}}} } } \times dt \) must also be a constant under these conditions. Furthermore, \( {\int\limits_{t = 0}^{t = \infty } {C{\left( {{{\text{\% ID}}} \mathord{\left/ {\vphantom {{{\text{\% ID}}} {\text{g}}}} \right. \kern-\nulldelimiterspace} {\text{g}}} \right)}_{{{\text{blood}}}} } } \times dt \) is a constant for the free labeled effector alone. In pretargeted mice, if the antibody concentration in normal tissues is sufficiently low, to a first approximation, the integral will be unchanged from the effector alone condition. Therefore, E must be a constant and can also be put outside of the integral. However, at dosages of effector greater than required to saturate the MORF antibody in tumor, E will become zero at some point when there is no longer MORF in tumor available to retain the effector, resulting in a smaller percent accumulation. Therefore, the accumulation before saturation of pretargeting agent in tumor will be the MPTA:
This equation shows that the MPTA is independent of the pretargeting agent and dependent only on the tumor and the effector.
Rights and permissions
About this article
Cite this article
Liu, G., Dou, S., Pretorius, P.H. et al. Pretargeting CWR22 prostate tumor in mice with MORF-B72.3 antibody and radiolabeled cMORF. Eur J Nucl Med Mol Imaging 35, 272–280 (2008). https://doi.org/10.1007/s00259-007-0606-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0606-z