Abstract.
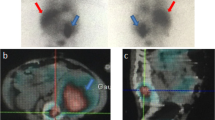
The usefulness and complementarity of gallium (67Ga) scintigraphy and computed tomography (CT) in the management of patients with lymphoma have been extensively demonstrated. Owing to a lack of anatomical landmarks and physiological distribution of the tracer, precise localisation of abnormalities on 67Ga scintigraphy can be difficult. As fusion imaging techniques between single-photon emission tomography (SPET) and CT have been developed recently, we investigated whether use of CT/67Ga SPET fusion imaging could help in the interpretation of 67Ga scintigraphy. From November 1999 to May 2001, 52 consecutive fusion studies were performed in 38 patients [22 patients with Hodgkin's disease (HD) and 16 patients with non-Hodgkin's lymphoma (NHL)] as part of pre-treatment staging (n=13), treatment evaluation (n=20) or evaluation of suspected recurrence (n=19). 67Ga scintigraphy was carried out 2 and 6 days following the injection of 185–220 MBq 67Ga citrate. On day 2, 67Ga SPET and CT were performed, focussing on the chest and/or the abdomen/pelvis. Data from each imaging method were co-registered using external markers. 67Ga scintigraphy and CT were initially interpreted independently by nuclear medicine physicians and radiologists. CT/67Ga SPET fusion studies were then jointly interpreted and both practitioners indicated when fusion provided additional information in comparison with CT and 67Ga SPET alone. Image fusion was considered to be of benefit in 12/52 (23%) studies which were performed for initial staging (n=4), treatment evaluation (n=4) or evaluation of suspected recurrence (n=4). In these cases, image fusion allowed either confirmation and/or localisation of pathological gallium uptake (n=10) or detection of lesions not visible on CT scan (n=2). Fusion was relevant for discrimination between osseous lesions and lymph node involvement adjacent to bone, especially in the thoracic and lumbar spine and pelvis. In the abdomen and pelvis, fusion helped to differentiate physiological bowel elimination from abnormal uptake, and assisted in precisely locating uptake in neighbouring viscera of the left hypochondrium, including the spleen, left liver lobe, coeliac area, stomach wall and even the splenic flexure. At the thoracic level, fusion also proved useful for demonstrating clearly the relationships of abnormal foci to the pleura, hepatic dome, mediastinum, ribs or thoracic spine. Clinical management was altered by fusion imaging in one patient (chemotherapy was given instead of radiotherapy) and was potentially affected in three other patients (in that, in conjunction with other factors, the results of fusion imaging had an influence on the decision regarding use of irradiation and especially the treatment volume). In conclusion, CT/67Ga SPET fusion imaging allowed precise localisation of gallium uptake and correct attribution to the involved viscera, thereby altering the diagnosis in 20%–25% of studies in comparison with CT and 67Ga SPET analyses alone. CT/67Ga SPET fusion therefore appears valuable in facilitating the interpretation of 67Ga scintigraphy and we recommend its use in patients with lymphoma when CT and 67Ga scintigraphy are planned.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Electronic Publication
Rights and permissions
About this article
Cite this article
Chajari, M., Lacroix, J., Peny, AM. et al. Gallium-67 scintigraphy in lymphoma: is there a benefit of image fusion with computed tomography?. Eur J Nucl Med 29, 380–387 (2002). https://doi.org/10.1007/s00259-001-0704-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-001-0704-2