Abstract
Purpose
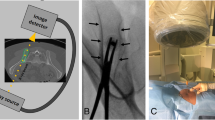
To assess the safety of fluoroscopically guided drill-assisted bone marrow aspirate and biopsy in severely thrombocytopenic patients.
Materials and methods
The study was approved by the IRB with waiver of informed consent. Retrospective review of 111 bone marrow aspirate and biopsies (BMAB) performed in 94 patients who received a CT scan which included the pelvis and biopsy site within the 7 days following the BMAB. The 94 patients were subdivided based on their platelet count: severe thrombocytopenia (< 20 platelets × 109/L), thrombocytopenia (20–50 platelets × 109/L), and control (> 50 platelets × 109/L). The procedure report was reviewed for sedation time, aspirate volume, and aggregate size of core biopsy specimens. The electronic medical record was reviewed for specimen adequacy; pathologic diagnosis; body mass index; pre- and post-procedure labs including platelet count, hemoglobin (HGB), hematocrit (HCT), prothrombin time (PT), and international normalized ratio (INR) levels; post-procedural transfusion; and complications including mortality at 30 and 90 days. CT scans were independently reviewed by 2 fellowship-trained radiologists for the presence of post-procedural hemorrhage.
Results
There was no significant difference in CT-identified post-procedural hematoma, or change in the hemoglobin and hematocrit levels pre- and post-procedure between the three groups. There was no significant difference in complication rate or all-cause mortality. There was a significant difference in transfusion at 30 days with thrombocytopenic and severely thrombocytopenic patients more likely to receive transfusion within the 30 days post-procedure.
Conclusion
Fluoroscopically guided BMAB can be safely performed in patients with severe thrombocytopenia.

Similar content being viewed by others
References
Bain BJ. Bone marrow aspiration. J Clin Pathol. 2001;54:657–63.
Nguyen PL. Collection, processing, and examination of bone marrow specimens. In: Jaffe E, Arber D, Campo E, Quintanilla-Martinez L, Orazi A, editors. Hematopathology. Second ed. Philadelphia: Elsevier Inc.; 2016. p. 29–40.
Martí J, Antón E, Valentí C. Complications of bone marrow biopsy. Br J Haematol. 2004;124:557–8.
Bain BJ. Bone marrow biopsy morbidity: review of 2003. J Clin Pathol. 2005;58:406–8.
Bain BJ. Bone marrow biopsy morbidity and mortality. Br J Haematol. 2003;121:949–51.
Roth JS, Newman EC. Gluteal compartment syndrome and sciatica after bone marrow biopsy: a case report and review of the literature. Am Surg. 2002;68:791–4.
Le Dieu R, Luckit J, Sundarasun M. Complications of trephine biopsy. Br J Haematol. 2003;121:822.
Chamisa I. Fatal vascular retroperitoneal injury following bone marrow biopsy. S Afr Med J. 2007;97:246.
Pedersen LM, Jarner D, Winge J. Bone-marrow biopsy of the iliac bone followed by severe retroperitoneal hemorrhage. Eur J Haematol. 1993;51:52.
Ge PS, Ng G, Ishaque BM, Gelabert H, de Virgilio C. Iatrogenic pseudoaneurysm of the superior gluteal artery presenting as pelvic mass with foot drop and sciatica: case report and review of literature. Vasc Endovasc Surg. 2010;44:64–8.
Long JR, Stensby JD, Wiesner EL, Bryson WN, Hillen TJ, Jennings JW. Efficacy and safety of bone marrow aspiration and biopsy using fluoroscopic guidance and a drill-powered needle: clinical experience from 775 cases [published online ahead of print June 9, 2020]. Eur Radiol doi: https://doi.org/10.1007/s00330-020-06987-3
Bayer WL, Bodensteiner DC, Tilzer LL, Adams ME. Use of platelets and other transfusion products in patients with malignancy. Semin Thromb Hemost. 1992;18:380–91.
Gmür J, Burger J, Schanz U, Fehr J, Schaffner A. Safety of stringent prophylactic platelet transfusion policy for patients with acute leukaemia. Lancet. 1991;338:1223–6.
Eikelboom JW. Bone marrow biopsy in thrombocytopenic or anticoagulated patients. Br J Haematol. 2005;129:562–3.
Patel IJ, Rahim S, Davidson JC, Hanks SE, Tam AL, Walker TG, et al. Society of Interventional Radiology consensus guidelines for the periprocedural management of thrombotic and bleeding risk in patients undergoing percutaneous image-guided interventions-part II: recommendations: endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol. 2019;30:1168–1184.e1.
Schiffer CA, Anderson KC, Bennett CL, Bernstein S, Elting LS, Goldsmith M, et al. Platelet transfusion for patients with cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol. 2001;19:1519–38.
Liu B, Limback J, Kendall M, Valente M, Armaly J, Grekoski V, et al. Safety of CT-guided bone marrow biopsy in thrombocytopenic patients: a retrospective review. J Vasc Interv Radiol. 2017;28:1727–31.
Lowenthal RM, Taylor BV, Jones R, Beasley A. Severe persistent sciatic pain and weakness due to a gluteal artery pseudoaneurysm as a complication of bone marrow biopsy. J Clin Neurosci. 2006;13:384–5.
Arellano-Rodrigo E, Real MI, Muntañola A, Burrel M, Rozman M, Fraire GV, et al. Successful treatment by selective arterial embolization of severe retroperitoneal hemorrhage secondary to bone marrow biopsy in post-polycythemic myelofibrosis. Ann Hematol. 2004;83:67–70.
Al Zahrani Y, Peck D. Median sacral artery injury following a bone marrow biopsy successfully treated with selective trans-arterial embolization: a case report. J Med Case Rep. 2016;10:42.
Wojciechowski A, Duckert M, Hartmann J, Bullinger L, Matzdorff A. Retroperitoneal hematoma after bone marrow biopsy: the first cut should not be the deepest. Oncol Res Treat. 2019;42:283–8.
Salem P, Wolverson MK, Reimers HJ, Kudva GC. Complications of bone marrow biopsy. Br J Haematol. 2003;121:821.
Neesse A, Kalinowski M, Walthers EM, Görg C, Neubauer A. Clinical management of massive retroperitoneal hemorrhage after bone marrow biopsy. Leuk Lymphoma. 2009;50:475–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stensby JD and Long JR declare that they have no conflict of interest.
Hillen TJ is a consultant for Consultant Medtronic, SI Bone, ERT, and Ultragenyx.
Jennings JW is a consultant for Merit Medical System, Medtronic, Stryker, Bard, and Teleflex Arrow.
Informed consent
The project was approved by the IRB with a waiver of informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stensby, J., Long, J., Hillen, T. et al. Safety of bone marrow aspiration and biopsy in severely thrombocytopenic patients. Skeletal Radiol 50, 915–920 (2021). https://doi.org/10.1007/s00256-020-03623-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03623-5