Abstract
Objective
To assess sacroiliac joint (SIJ) modifications on MRI and their ability to predict axial spondyloarthritis (SpA) with the purpose of identifying parameters for future prospective studies.
Methods
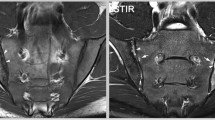
Retrospective study was carried out of 110 consecutive patients referred for SIJ MRI with coronal, axial short TI inversion recovery (STIR), and axial T1 sequences over 6 months. Factors associated with SpA, including MRI SIJ modifications (fat deposition, structural abnormalities on T1-weighted images, and bone marrow edema [BME] on STIR sequences) and age were explored using multivariate logistic regression. The reference diagnosis was made 1–1.5 years later based on clinical, radiological, and biological findings, according to Assessment of SpondyloArthritis International Society (ASAS) criteria.
Results
Twenty-eight patients were diagnosed with SpA (female/male: 19/9, age 41 ± 13 years). Abnormal findings were found in up to 21 % of patients without SpA (including 11 % with BME), versus 64 % of SpA patients (50 % with BME). A threshold age of 42.6 years was found to discriminate SpA patients (ROC AUC: 0.71, 95 % CI: 0.59–0.81). BME location in the sacral (OR: 7.07 [1.05, 47.6], p = 0.044) and both sacral and iliac areas (OR: 36.0 [5.61, 231], p = 0.0002), as well as age (OR: 0.95 [0.92, 0.98], p = 0.0019) were found to be independent predictors of SpA. 83.6 % of patients were effectively diagnosed using BME location and patient age in a classification and regression tree (CART) algorithm (sensitivity: 61 %, specificity: 91 %, PPV: 71 %, NPV: 87 %).
Conclusion
The BME location combined with the patient’s age (threshold 42.6 years) could help predict SpA. Further studies are required before these features can be used by radiologists to boost their confidence in reporting SIJ MRI.





Similar content being viewed by others
References
Khan MA, van der Linden SM. Ankylosing spondylitis and other spondyloarthropathies. Rheum Dis Clin North Am. 1990;16(3):551–79.
Goie The HS, Steven MM, van der Linden SM, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a comparison of the Rome, New York and modified New York criteria in patients with a positive clinical history screening test for ankylosing spondylitis. Br J Rheumatol. 1985;24(3):242–9.
Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27(4):361–8.
Rudwaleit M, Jurik AG, Hermann KG, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis. 2009;68(10):1520–7.
Rudwaleit M, Landewe R, van der Heijde D, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis. 2009;68(6):770–6.
Aydin SZ, Maksymowych WP, Bennett AN, McGonagle D, Emery P, Marzo-Ortega H. Validation of the ASAS criteria and definition of a positive MRI of the sacroiliac joint in an inception cohort of axial spondyloarthritis followed up for 8 years. Ann Rheum Dis. 2012;71(1):56–60.
Weber U, Zubler V, Pedersen SJ, et al. Development and validation of an MRI reference criterion for defining a positive SIJ MRI in spondyloarthritis. Arthritis Care Res. 2013;65(6):977–85.
Zanetti M, Bruder E, Romero J, Hodler J. Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology. 2000;215(3):835–40.
Xu L, Hayashi D, Roemer FW, Felson DT, Guermazi A. Magnetic Resonance Imaging of Subchondral Bone Marrow Lesions in Association with Osteoarthritis. Semin Arthritis Rheum. 2012;42(2):105–18.
Rudwaleit M, Braun J, Sieper J. ASAS classification criteria for axial spondyloarthritis. Z Rheumatol. 2009;68(7):591–3.
Landis JR. The measurement of observer agreement for categorical data. Biometrics 1977;33(1):159–74.
Breiman LFJ, Olshen R, Stone C. Classification and regression trees. Belmont: Wadsworth; 1984.
Weber U, Lambert RG, Ostergaard M, Hodler J, Pedersen SJ, Maksymowych WP. The diagnostic utility of magnetic resonance imaging in spondylarthritis: an international multicenter evaluation of one hundred eighty-seven subjects. Arthritis Rheum. 2010;62(10):3048–58.
McLauchlan GJ, Gardner DL. Sacral and iliac articular cartilage thickness and cellularity: relationship to subchondral bone end-plate thickness and cancellous bone density. Rheumatology (Oxford). 2002;41(4):375–80.
Bollow M, Hermann KG, Biedermann T, Sieper J, Schontube M, Braun J. Very early spondyloarthritis: where the inflammation in the sacroiliac joints starts. Ann Rheum Dis. 2005;64(11):1644–6.
Bollow M, Biedermann T, Kannenberg J, et al. Use of dynamic magnetic resonance imaging to detect sacroiliitis in HLA-B27 positive and negative children with juvenile arthritides. J Rheumatol. 1998;25(3):556–64.
Madsen KB, Egund N, Jurik AG. Grading of inflammatory disease activity in the sacroiliac joints with magnetic resonance imaging: comparison between short-tau inversion recovery and gadolinium contrast-enhanced sequences. J Rheumatol. 2009;37(2):393–400.
Weber U, Lambert RG, Pedersen SJ, Hodler J, Ostergaard M, Maksymowych WP. Assessment of structural lesions in sacroiliac joints enhances diagnostic utility of magnetic resonance imaging in early spondylarthritis. Arthritis Care Res. 2010;62(12):1763–71.
Weber U PS, Hodler J, Ostergaard M, Lambert RG, Maksymowych WP Does fat infiltration in sacroiliac joint contribute to the diagnostic utility of MRI in ankylosing spondylitis? Arthrtis Rheum. 2009;(Suppl 10):54.
Puhakka KB, Jurik AG, Egund N, et al. Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol. 2003;44(2):218–29.
Weber U, Pedersen SJ, Ostergaard M, Rufibach K, Lambert RG, Maksymowych WP. Can erosions on MRI of the sacroiliac joints be reliably detected in patients with ankylosing spondylitis?—A cross-sectional study. Arthritis Res Ther. 2012;14(3):R124.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Larbi, A., Viala, P., Molinari, N. et al. Assessment of MRI abnormalities of the sacroiliac joints and their ability to predict axial spondyloarthritis: a retrospective pilot study on 110 patients. Skeletal Radiol 43, 351–358 (2014). https://doi.org/10.1007/s00256-013-1789-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-013-1789-y