Abstract
Objective
To evaluate trochlear morphology as a potential risk factor for patellofemoral osteoarthritis, determined by morphological and quantitative measurements of cartilage degeneration using 3-T magnetic resonance imaging (MRI) of the knee.
Materials and methods
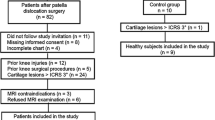
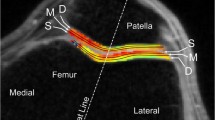
MRI of the right knees of 304 randomly selected subjects, aged 45–60 years, from the Osteoarthritis Initiative (OAI) progression cohort were screened for trochlear dysplasia, defined by an abnormal trochlear depth. Out of 304 subjects, n = 85 demonstrated a shallow trochlea (depth ≤3 mm; 28 %). In these, and also in a random sample of controls with normal trochlear depth (n = 50), the facet ratio and the sulcus angle were calculated and knee structural abnormalities were assessed by using a modified Whole Organ MR Imaging Score (WORMS). Cartilage segmentation was performed and T2 relaxation times and patellar cartilage volume were determined. ANOVA and multivariate regression models were used for statistical analysis of the association of MRI structural measures and trochlear morphology.
Results
Knees with a shallow trochlea showed higher patellofemoral degeneration (WORMS mean ± standard deviation, 11.2 ± 0.5 versus 5.7 ± 0.6; multivariate regression, P < 0.001) and lower patellar cartilage volume than controls (900 ± 664 mm3 versus 1,671 ± 671 mm3; P < 0.001). Knees with an abnormal medial-to-lateral facet ratio (<0.4) showed increased patellofemoral WORMS scores (12.3 ± 0.9 versus 8.3 ± 0.5; P < 0.001). Knees with an abnormal sulcus angle (>170°) also showed increased WORMS scores (12.2 ± 1.1 versus 8.6 ± 0.6; P = 0.003). T2 values at the patella were significantly lower in the dysplasia group with a shallow trochlea. However, significance was lost after adjustment for cartilage volume (P = 0.673).
Conclusion
Trochlear dysplasia, defined by a shallow trochlea, was associated with higher WORMS scores and lower cartilage volume, indicating more advanced osteoarthritis at the patellofemoral joint.



Similar content being viewed by others
References
Christian SR, Anderson MB, Workman R, Conway WF, Pope TL. Imaging of anterior knee pain. Clin Sports Med. 2006;25(4):681–702.
Hedayati B, Saifuddin A. Focal lesions of the patella. Skeletal Radiol. 2009;38(8):741–9.
Tecklenburg K, Dejour D, Hoser C, Fink C. Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):235–40.
Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: Relation to patellar dislocation. Radiology. 1989;170(2):507–10.
Grelsamer RP, Tedder JL. The lateral trochlear sign. Femoral trochlear dysplasia as seen on a lateral view roentgenograph. Clin Orthop Relat Res. 1992;281:159–62.
Pfirrmann CW, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology. 2000;216(3):858–64.
Koeter S, Bongers EM, de Rooij J, van Kampen A. Minimal rotation aberrations cause radiographic misdiagnosis of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):713–7.
Salzmann GM, Weber TS, Spang JT, Imhoff AB, Schottle PB. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with trochlear dysplasia. Arch Orthop Trauma Surg. 2010;130(3):335–40.
Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: Injury patterns and assessment of risk factors. Radiographics. 2010;30(4):961–81.
Toms AP, Cahir J, Swift L, Donell ST. Imaging the femoral sulcus with ultrasound, CT, and MRI: Reliability and generalizability in patients with patellar instability. Skeletal Radiol. 2009;38(4):329–38.
Fitoussi F, Akoure S, Chouteau Y, Bouger D. Hollow femoral trochlea and femoro-patellar osteoarthritis. Rev Chir Orthop Reparatrice Appar Mot. 1994;80(6):520–4.
Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(1):45–54.
Crema MD, Roemer FW, Marra MD, Burstein D, Gold GE, Eckstein F, et al. Articular cartilage in the knee: Current MR imaging techniques and applications in clinical practice and research. Radiographics. 2011;31(1):37–61.
Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–62.
Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage. 2008;16(12):1433–41.
Peterfy CG, Guermazi A, Zaim S, Tirman PFJ, Miaux Y, White D, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12(3):177–90.
Stehling C, Lane NE, Nevitt MC, Lynch J, McCulloch CE, Link TM. Subjects with higher physical activity levels have more severe focal knee lesions diagnosed with 3T MRI: Analysis of a non-symptomatic cohort of the osteoarthritis initiative. Osteoarthritis Cartilage. 2010;18(6):776–86.
Baum T, Stehling C, Joseph GB, Carballido-Gamio J, Schwaiger BJ, Muller-Hocker C, et al. Changes in knee cartilage T2 values over 24 months in subjects with and without risk factors for knee osteoarthritis and their association with focal knee lesions at baseline: data from the osteoarthritis initiative. J Magn Reson Imaging. 2012;35(2):370–8.
Baum T, Joseph GB, Nardo L, Virayavanich W, Arulanandan A, Alizai H, et al. Correlation of magnetic resonance imaging-based knee cartilage T2 measurements and focal knee lesions with body mass index: thirty-six-month followup data from a longitudinal, observational multicenter study. Arthritis Care Res (Hoboken). 2013;65(1):23–33
Stehling C, Baum T, Mueller-Hoecker C, Liebl H, Carballido-Gamio J, Joseph GB, et al. A novel fast knee cartilage segmentation technique for T2 measurements at MR imaging–data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2011;19(8):984–9.
Jungmann P, Kraus M, Nardo L, Liebl H, Alizai H, Joseph G, et al. T2 relaxation time measurements are limited in monitoring progression, once advanced cartilage defects at the knee occur. Longitudinal data from the Osteoarthritis Initiative. J Magn Reson Imaging. 2013; In press.
Dandy DJ. Chronic patellofemoral instability. J Bone Joint Surg Br. 1996;78(2):328–35.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26.
Fucentese SF, Schottle PB, Pfirrmann CW, Romero J. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):168–74.
Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76(5):693–8.
Van Huyssteen AL, Hendrix MR, Barnett AJ, Wakeley CJ, Eldridge JD. Cartilage-bone mismatch in the dysplastic trochlea. An MRI study. J Bone Joint Surg Br. 2006;88(5):688–91.
Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):529–33.
Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 Relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232(2):592–8.
Pan J, Pialat JB, Joseph T, Kuo D, Joseph GB, Nevitt MC, et al. Knee cartilage T2 characteristics and evolution in relation to morphologic abnormalities detected at 3-T MR imaging: a longitudinal study of the normal control cohort from the Osteoarthritis Initiative. Radiology. 2011;261(2):507–15
David-Vaudey E, Ghosh S, Ries M, Majumdar S. T2 relaxation time measurements in osteoarthritis. Magn Reson Imaging. 2004;22(5):673–82.
Akizuki S, Mow VC, Muller F, Pita JC, Howell DS. Tensile properties of human knee joint cartilage. II. Correlations between weight bearing and tissue pathology and the kinetics of swelling. J Orthop Res. 1987;5(2):173–86.
Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, et al. Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1{rho} and T2–initial experience with 1-year follow-up. Radiology. 2011;258(2):505–14.
Acknowledgements
This study was funded by NIH U01 AR059507 and P50 AR060752 as well as through the OAI, which is a public–private partnership comprising five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health.
Conflict of interest
No conflict of interest to declare for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jungmann, P.M., Tham, SC., Liebl, H. et al. Association of trochlear dysplasia with degenerative abnormalities in the knee: data from the Osteoarthritis Initiative. Skeletal Radiol 42, 1383–1392 (2013). https://doi.org/10.1007/s00256-013-1664-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-013-1664-x