Abstract
Background
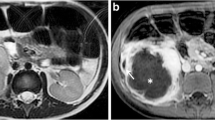
Acute appendicitis, especially if perforated at presentation, is often complicated by postoperative abscess formation. The detection of a postoperative abscess relies primarily on imaging. This has traditionally been done with contrast-enhanced computed tomography. Non-contrast magnetic resonance imaging (MRI) has the potential to accurately detect intra-abdominal abscesses, especially with the use of diffusion-weighted imaging (DWI).
Objective
To evaluate our single-center experience with a rapid non-contrast MRI protocol evaluating post-appendectomy abscesses in children with persistent postsurgical symptoms.
Materials and methods
In this retrospective, institutional review board-approved study, all patients underwent a clinically indicated non-contrast 1.5- or 3-Tesla abdomen/pelvis MRI consisting of single-shot fast spin echo, inversion recovery and DWI sequences. All MRI studies were reviewed by two blinded pediatric radiologists to identify the presence of a drainable fluid collection. Each fluid collection was further characterized as accessible or not accessible for percutaneous or transrectal drainage. Imaging findings were compared to clinical outcome.
Results
Seven of the 15 patients had a clinically significant fluid collection, and 5 of these patients were treated with percutaneous drain placement or exploratory laparotomy. The other patients had a phlegmon or a clinically insignificant fluid collection and were discharged home within 48 h.
Conclusion
Rapid non-contrast MRI utilizing fluid-sensitive and DWI sequences can be used to identify drainable fluid collections in post-appendectomy patients. This protocol can be used to triage patients between conservative management vs. abscess drainage without oral/intravenous contrast or exposure to ionizing radiation.



Similar content being viewed by others
References
Gasior AC, St Peter SD, Knott EM et al (2012) National trends in approach and outcomes with appendicitis in children. J Pediatr Surg 47:2264–2267
Cheong LH, Emil S (2014) Outcomes of pediatric appendicitis: an international comparison of the United States and Canada. JAMA Surg 149:50–55
Emil S, Laberge JM, Mikhail P et al (2003) Appendicitis in children: a ten-year update of therapeutic recommendations. J Pediatr Surg 38:236–242
Fike FB, Mortellaro VE, Juang D et al (2011) The impact of postoperative abscess formation in perforated appendicitis. J Surg Res 170:24–26
Fishman SJ, Pelosi L, Klavon SL et al (2000) Perforated appendicitis: prospective outcome analysis for 150 children. J Pediatr Surg 35:923–926
Neubauer H, Platzer I, Mueller VR et al (2012) Diffusion-weighted MRI of abscess formations in children and young adults. World J Pediatr 8:229–234
Oto A, Schmid-Tannwald C, Agrawal G et al (2011) Diffusion-weighted MR imaging of abdominopelvic abscesses. Emerg Radiol 18:515–524
Ikeda H, Ishimaru Y, Takayasu H et al (2004) Laparoscopic versus open appendectomy in children with uncomplicated and complicated appendicitis. J Pediatr Surg 39:1680–1685
Emil S, Elkady S, Shbat L et al (2014) Determinants of postoperative abscess occurrence and percutaneous drainage in children with perforated appendicitis. Pediatr Surg Int 30:1265–1271
Fraser JD, Aguayo P, Sharp SW et al (2010) Physiologic predictors of postoperative abscess in children with perforated appendicitis: subset analysis from a prospective randomized trial. Surgery 147:729–732
Obayashi J, Ohyama K, Manabe S et al (2015) Are there reliable indicators predicting post-operative complications in acute appendicitis? Pediatr Surg Int 31:1189–1193
Chavhan GB, Caro-Dominguez P (2016) Diffusion-weighted imaging in pediatric body magnetic resonance imaging. Pediatr Radiol 46:847–857
Ream JM, Dillman JR, Adler J et al (2013) MRI diffusion-weighted imaging (DWI) in pediatric small bowel Crohn disease: correlation with MRI findings of active bowel wall inflammation. Pediatr Radiol 43:1077–1085
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Lee, M.H., Eutsler, E.P., Sheybani, E.F. et al. Rapid non-contrast magnetic resonance imaging for post appendectomy intra-abdominal abscess in children. Pediatr Radiol 47, 935–941 (2017). https://doi.org/10.1007/s00247-017-3860-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3860-7