Abstract
Background
The value of late-gadolinium-enhancement (LGE) imaging in the diagnosis and management of pediatric and congenital heart disease is clear; however current acquisition techniques are susceptible to error and artifacts when performed in children because of children’s higher heart rates, higher prevalence of sinus arrhythmia, and inability to breath-hold. Commonly used techniques in pediatric LGE imaging include breath-held segmented FLASH (segFLASH) and steady-state free precession-based (segSSFP) imaging. More recently, single-shot SSFP techniques with respiratory motion-corrected averaging have emerged.
Objective
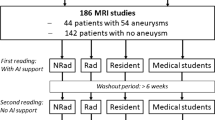
This study tested and compared single-shot free-breathing LGE techniques with standard segmented breath-held techniques in children undergoing LGE imaging.
Materials and methods
Thirty-two consecutive children underwent clinically indicated late-enhancement imaging using intravenous gadobutrol 0.15 mmol/kg. Breath-held segSSFP, breath-held segFLASH, and free-breathing single-shot SSFP LGE sequences were performed in consecutive series in each child. Two blinded reviewers evaluated the quality of the images and rated them on a scale of 1–5 (1 = poor, 5 = superior) based on blood pool–myocardial definition, presence of cardiac motion, presence of respiratory motion artifacts, and image acquisition artifact. We used analysis of variance (ANOVA) to compare groups.
Results
Patients ranged in age from 9 months to 18 years, with a mean +/− standard deviation (SD) of 13.3 +/− 4.8 years. R-R interval at the time of acquisition ranged 366–1,265 milliseconds (ms) (47–164 beats per minute [bpm]), mean +/− SD of 843+/−231 ms (72+/−21 bpm). Mean +/− SD quality ratings for long-axis imaging for segFLASH, segSSFP and single-shot SSFP were 3.1+/−0.9, 3.4+/−0.9 and 4.0+/−0.9, respectively (P < 0.01 by ANOVA). Mean +/− SD quality ratings for short-axis imaging for segFLASH, segSSFP and single-shot SSFP were 3.4+/−1, 3.8+/−0.9 and 4.3+/−0.7, respectively (P < 0.01 by ANOVA).
Conclusion
Single-shot late-enhancement imaging with motion-corrected averaging is feasible in children, robust at high heart rates and with variable R-R intervals, and can be performed without breath-holding with higher image quality ratings than standard breath-held techniques. Use of free-breathing single-shot motion-corrected technique does not compromise LGE image quality in children who can hold their breath, and it can significantly improve image quality in children who cannot hold their breath or who have significant arrhythmia.




Similar content being viewed by others
References
Babu-Narayan SV, Kilner PJ, Li W et al (2006) Ventricular fibrosis suggested by cardiovascular magnetic resonance in adults with repaired tetralogy of Fallot and its relationship to adverse markers of clinical outcome. Circulation 113:405–413
Secinaro A, Ntsinjana H, Tann O et al (2011) Cardiovascular magnetic resonance findings in repaired anomalous left coronary artery to pulmonary artery connection (ALCAPA). J Cardiovasc Magn Reson 13:27
Hor KN, Taylor MD, Al-Khalidi HR et al (2013) Prevalence and distribution of late gadolinium enhancement in a large population of patients with Duchenne muscular dystrophy: effect of age and left ventricular systolic function. J Cardiovasc Magn Reson 15:107
Chan RH, Maron BJ, Olivotto I et al (2014) Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation 130:484–495
Mavrogeni S, Bratis K, Georgakopoulos D et al (2012) Evaluation of myocarditis in a pediatric population using cardiovascular magnetic resonance and endomyocardial biopsy. Int J Cardiol 160:192–195
Ylänen K, Poutanen T, Savikurki-Heikkilä P et al (2013) Cardiac magnetic resonance imaging in the evaluation of the late effects of anthracyclines among long-term survivors of childhood cancer. J Am Coll Cardiol 61:1539–1547
Simonetti OP, Kim RJ, Fieno DS et al (2001) An improved MR imaging technique for the visualization of myocardial infarction. Radiology 218:215–223
Rangamani S, Varghese J, Li L et al (2012) Safety of cardiac magnetic resonance and contrast angiography for neonates and small infants: a 10-year single-institution experience. Pediatr Radiol 42:1339–1346
Huber A, Schoenberg SO, Spannagl B et al (2006) Single-shot inversion recovery TrueFISP for assessment of myocardial infarction. AJR Am J Roentgenol 186:627–633
Huber A, Bauner K, Wintersperger BJ et al (2006) Phase-sensitive inversion recovery (PSIR) single-shot TrueFISP for assessment of myocardial infarction at 3 tesla. Investig Radiol 41:148–153
Kellman P, Larson AC, Hsu L-Y et al (2005) Motion-corrected free-breathing delayed enhancement imaging of myocardial infarction. Magn Reson Med 53:194–200
Ledesma-Carbayo MJ, Kellman P, Hsu L-Y et al (2007) Motion corrected free-breathing delayed-enhancement imaging of myocardial infarction using nonrigid registration. J Magn Reson Imaging 26:184–190
Kellman P, Arai AE (2012) Cardiac imaging techniques for physicians: late enhancement. J Magn Reson Imaging 36:529–542
Piehler KM, Wong TC, Puntil KS et al (2013) Free-breathing, motion-corrected late gadolinium enhancement is robust and extends risk stratification to vulnerable patients. Circ Cardiovasc Imaging 6:423–432
Chefd’hotel C, Hermosillo G, Faugeras O (2002) Flows of diffeomorphisms for multimodal image registration. Proc IEEE Int Symp Biomed Imaging, pp 753–756. doi:10.1109/ISBI.2002.1029367
Hermosillo G, Chefd’hotel C, Faugeras O (2002) Variational methods for multimodal image matching. Int J Comput Vis 50:329–343
Acknowledgments
This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Heart, Lung, and Blood Institute, and through NHLBI contract award HHSN268201500001C.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Olivieri, L., Cross, R., O’Brien, K.J. et al. Free-breathing motion-corrected late-gadolinium-enhancement imaging improves image quality in children. Pediatr Radiol 46, 983–990 (2016). https://doi.org/10.1007/s00247-016-3553-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3553-7