Abstract
Introduction
Abdominal injuries in abused children are less common than musculoskeletal and craniocerebral injuries; however they carry high mortality and morbidity rates. In every case of trauma, regardless of aetiology, radiologists are responsible for the documentation and evaluation of injuries.
Injuries
Any abdominal injury pattern maybe observed following physical abuse and none is specific for abuse. However, a high index of suspicion should be maintained for every case of pancreatic, hollow viscous and other solid organ injuries, especially when there is delay in seeking help, a history of trauma to the child or siblings, young age, undernourishment, ecchymosis in non-ambulatory children or a non-plausible explanation for the injuries based on the provided history and the psychomotor condition of the child.
Imaging modalities
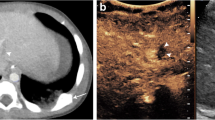
CT with intravenous contrast material is the imaging modality of choice in every suspected inflicted abdominal injury. US could be the first imaging test for abused children with a low probability of abdominal injury and for follow-up. Upper gastrointestinal series could reveal acute or resolving mural haematomas in children with equivocal CT or US findings.
Conclusion
Child abuse should be considered in the differential diagnosis of acute abdominal symptoms in young children.


















Similar content being viewed by others
References
Roaten JB, Partrick DA, Nydam TL et al (2006) Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. J Pediatr Surg 41:2013–2015
DiScala C, Sege R, Li G et al (2000) Child abuse and unintentional injuries: a 10-year retrospective. Arch Pediatr Adolesc Med 154:16–22
Cooper A, Floyd T, Barlow B et al (1988) Major blunt abdominal trauma due to child abuse. J Trauma 28:1483–1487
Lonergan GJ, Baker AM, Morey MK et al (2003) From the archives of the AFIP. Child abuse: radiologic-pathologic correlation. Radiographics 23:811–845
Wood J, Rubin DM, Nance ML et al (2005) Distinguishing inflicted versus accidental abdominal injuries in young children. J Trauma 59:1203–1208
Sanders T, Cobley C (2005) Identifying non-accidental injury in children presenting to A&E departments: an overview of the literature. Accid Emerg Nurs 13:130–136
Barnes PM, Norton CM, Dunstan FD et al (2005) Abdominal injury due to child abuse. Lancet 366:234–235
Trokel M, Discala C, Terrin NC et al (2006) Patient and injury characteristics in abusive abdominal injuries. Pediatr Emerg Care 22:700–704
Rothrock SG, Green SM, Morgan R (2000) Abdominal trauma in infants and children: prompt identification and early management of serious and life-threatening injuries. Part I: injury patterns and initial assessment. Pediatr Emerg Care 16:106–115
Ledbetter DJ, Hatch EI Jr, Feldman KW et al (1988) Diagnostic and surgical implications of child abuse. Arch Surg 123:1101–1105
Kleinman PK, Raptopoulos VD, Brill PW (1981) Occult nonskeletal trauma in the battered-child syndrome. Radiology 141:393–396
Kleinman PK (1990) Diagnostic imaging in infant abuse. AJR 155:703–712
Gornall P, Ahmed S, Jolleys A et al (1972) Intra-abdominal injuries in the battered baby syndrome. Arch Dis Child 47:211–214
Sivit CJ, Taylor GA, Eichelberger MR (1989) Visceral injury in battered children: a changing perspective. Radiology 173:659–661
Leventhal JM, Martin KD, Asnes AG (2010) Fractures and traumatic brain injuries: abuse versus accidents in a US database of hospitalized children. Pediatrics 126:e104–115
Reece RM, Sege R (2000) Childhood head injuries. Accidental or inflicted? Arch Pediatr Adolesc Med 154:11–15
Canty TG Sr, Canty TG Jr, Brown C (1999) Injuries of the gastrointestinal tract from blunt trauma in children: a 12-year experience at a designated pediatric trauma center. J Trauma 46:234–240
Lam JP, Eunson GJ, Munro FD et al (2001) Delayed presentation of handlebar injuries in children. BMJ 322:1288–1289
Pierce MC, Kaczor K, Aldridge S et al (2010) Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics 125:67–74
Adamsbaum C, Grabar S, Mejean N et al (2010) Abusive head trauma: judicial admissions highlight violent and repetitive shaking. Pediatrics 126:546–555
Rao P (2002) Emergency imaging in non-accidental injury. In: Carty H (ed) Emergency Pediatric Radiology, 2nd edn. Springer-Verlag, Berlin, pp 347–380
Waseem M, Perales O (2008) Pancreatic injury: accidental or nonaccidental. Pediatr Emerg Care 24:679–681
Hobbs CJ, Bilo RA (2009) Nonaccidental trauma: clinical aspects and epidemiology of child abuse. Pediatr Radiol 39:457–460
Kellogg ND, American Academy of Pediatrics Committee on Child Abuse and Neglect (2007) Evaluation of suspected child physical abuse. Pediatrics 119:1232–1241
No authors disclosed (2000) Diagnostic imaging of child abuse. Section on Radiology; American Academy of Pediatrics. Pediatrics 105:1345–1348
Di Pietro MA, Brody AS, Cassady CI et al (2009) Diagnostic imaging of child abuse. Section on Radiology; American Academy of Pediatrics. Pediatrics 123:1430–1435
Roaten JB, Partrick DA, Bensard DD et al (2005) Visceral injuries in nonaccidental trauma: spectrum of injury and outcomes. Am J Surg 190:827–829
Ng CS, Hall CM, Shaw DG (1997) The range of visceral manifestations of non-accidental injury. Arch Dis Child 77:167–174
Touloukian RJ (1983) Protocol for the nonoperative treatment of obstructing intramural duodenal hematoma during childhood. Am J Surg 145:330–334
Sivit CJ, Eichelberger MR, Taylor GA (1994) CT in children with rupture of the bowel caused by blunt trauma: diagnostic efficacy and comparison with hypoperfusion complex. AJR 163:1195–1198
Strouse PJ, Close BJ, Marshall KW et al (1999) CT of bowel and mesenteric trauma in children. Radiographics 19:1237–1250
Bulas DI, Eichelberger MR, Sivit CJ et al (1993) Hepatic injury from blunt trauma in children: follow-up evaluation with CT. AJR 160:347–351
Carty H (1991) The non skeletal injuries of child abuse. Part 2. The body. In: 1991 Year book of pediatric radiology, Vol 3, pp 143–187
Patrick LE, Ball TI, Atkinson GO et al (1992) Pediatric blunt abdominal trauma: periportal tracking at CT. Radiology 183:689–691
DiGiacomo JC, Frankel H, Haskell RM et al (2000) Unsuspected child abuse revealed by delayed presentation of periportal tracking and myoglobinuria. J Trauma 49:348–350
Kirks DR (1983) Radiological evaluation of visceral injuries in the battered child syndrome. Pediatr Ann 12:888–893
Cobb LM, Vinocur CD, Wagner CW et al (1986) Intestinal perforation due to blunt trauma in children in an era of increased nonoperative treatment. J Trauma 26:461–463
Kleinman PK, Brill PW, Winchester P (1986) Resolving duodenal-jejunal hematoma in abused children. Radiology 160:747–750
Kunin JR, Korobkin M, Ellis JH et al (1993) Duodenal injuries caused by blunt abdominal trauma: value of CT in differentiating perforation from hematoma. AJR 160:1221–1223
Sivit CJ, Taylor GA, Bulas DI et al (1992) Posttraumatic shock in children: CT findings associated with hemodynamic instability. Radiology 182:723–726
Sivit CJ (2009) Imaging children with abdominal trauma. AJR 192:1179–1189
King LR, Siegel MJ, Balfe DM (1995) Acute pancreatitis in children: CT findings of intra- and extrapancreatic fluid collections. Radiology 195:196–200
Sivit CJ, Eichelberger MR, Taylor GA et al (1992) Blunt pancreatic trauma in children: CT diagnosis. AJR 158:1097–1100
Emery KH, Babcock DS, Borgman AS et al (1999) Splenic injury diagnosed with CT: US follow-up and healing rate in children and adolescents. Radiology 212:515–518
Benya EC, Bulas DI, Eichelberger MR et al (1995) Splenic injury from blunt abdominal trauma in children: follow-up evaluation with CT. Radiology 195:685–688
Nimkin K, Teeger S, Wallach MT et al (1994) Adrenal hemorrhage in abused children: imaging and postmortem findings. AJR 162:661–663
Peebles J, Losek JD (2007) Child physical abuse and rhabdomyolysis: case report and literature review. Pediatr Emerg Care 23:474–477
Hobbs CJ, Osman J (2007) Genital injuries in boys and abuse. Arch Dis Child 92:328–331
Hilfer CL, Holgersen LO (1995) Massive chylous ascites and transected pancreas secondary to child abuse: successful non-surgical management. Pediatr Radiol 25:117–119
Boysen BE (1975) Chylous ascites. Manifestation of the battered child syndrome. Am J Dis Child 129:1338–1339
Sivit CJ, Cutting JP, Eichelberger MR (1995) CT diagnosis and localization of rupture of the bladder in children with blunt abdominal trauma: significance of contrast material extravasation in the pelvis. AJR 164:1243–1246
Shankar KR, Lloyd DA, Kitteringham L et al (1999) Oral contrast with computed tomography in the evaluation of blunt abdominal trauma in children. Br J Surg 86:1073–1077
Slovis TL, Smith WL, Strain JD et al (2005) Expert Panel on Pediatric Imaging. Suspected physical abuse-child. Reston (VA): (ACR) 5 p. 33 http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonPediatricImaging/SuspectedPhysicalAbuseChildDoc9.aspx
Lorente-Ramos RM, Santiago-Hernando A, Del Valle-Sanz Y et al (1999) Sonographic diagnosis of intramural duodenal hematomas. J Clin Ultrasound 27:213–316
Valentino M, Serra C, Pavlica P et al (2008) Blunt abdominal trauma: diagnostic performance of contrast-enhanced US in children–initial experience. Radiology 246:903–909
Navarro O, Babyn PS, Pearl RH (2000) The value of routine follow-up imaging in pediatric blunt liver trauma. Pediatr Radiol 30:546–550
Pranikoff T, Hirschl RB, Schlesinger AE et al (1994) Resolution of splenic injury after nonoperative management. J Pediatr Surg 29:1366–1369
Lindberg D, Makoroff K, Harper N et al (2009) Utility of hepatic transaminases to recognize abuse in children. Pediatrics 124:509–516
Jindal A, Velmahos GC, Rofougaran R (2002) Computed tomography for evaluation of mild to moderate pediatric trauma: are we overusing it? World J Surg 26:13–16
Coant PN, Kornberg AE, Brody AS et al (1992) Markers for occult liver injury in cases of physical abuse in children. Pediatrics 89:274–278
Lane WG, Dubowitz H, Langenberg P (2009) Screening for occult abdominal trauma in children with suspected physical abuse. Pediatrics 124:1595–1602
Adamson WT, Hebra A, Thomas PB et al (2003) Serum amylase and lipase alone are not cost-effective screening methods for pediatric pancreatic trauma. J Pediatr Surg 38:354–357
Matsuno WC, Huang CJ, Garcia NM et al (2009) Amylase and lipase measurements in paediatric patients with traumatic pancreatic injuries. Injury 40:66–71
Author information
Authors and Affiliations
Corresponding author
Additional information
CME Activity
This article has been selected as the CME Activity for the current month. Please visit the SPR website at www.pedrad.org on the Education page and follow the instructions to complete this CME Activity.
Rights and permissions
About this article
Cite this article
Raissaki, M., Veyrac, C., Blondiaux, E. et al. Abdominal imaging in child abuse. Pediatr Radiol 41, 4–16 (2011). https://doi.org/10.1007/s00247-010-1882-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1882-5