Abstract
Brain ultrasonography plays a central role in the detection and management of neonatal disease in the preterm infant. Although morphological study, using high-frequency transducers, remains the cornerstone of imaging, pulsed and colour Doppler scans provide additional information and improve the diagnostic and prognostic accuracy of ultrasonography. Particular features of normal brain US in the extremely preterm infant are reported. Cerebral haemorrhage and its different patterns (intraventricular haemorrhage and periventricular hemorrhagic infarction) are described. The value of Doppler techniques is emphasized, e.g. demonstration of coloured signal within the aqueduct of Sylvius, visualization of patency of the terminal veins, demonstration of Doppler spectrum fluctuations, recognition of low blood flow, and the detection of vasodilatation. The sonographic diagnosis of periventricular leucomalacia and its difficulties are documented. Some uncommon brain lesions of the premature infant are illustrated, e.g. gangliothalamic ischaemic damage, cortical necrosis, focal infarcts, etc. The importance of repeating the US examinations until near term is highlighted.
Similar content being viewed by others
Introduction
Since the 1980s, and the beginning of our experience of preterm brain ultrasonography [1], the spectrum of brain disease has changed considerably, with an increased number of extremely preterm infants, and a decreased incidence of haemorrhagic complications and macrocystic periventricular leucomalacia (PVL). In this evolution, ultrasonography has played a role: it is a non-invasive, radiation-free and reproducible procedure that can be performed at the bedside, in the intensive care unit, and on the intubated ventilated baby.
Intraventricular–periventricular haemorrhagic disease (IVH-PVH)
Intraventricular haemorrhage (IVH) versus germinal matrix haemorrhage (GMH)
When intraventricular bleeding is substantial, its morphological diagnosis is easy. The highly echogenic image is obviously located within the ventricular lumen. The role of ultrasonography is to appreciate the amount of blood and severity of injury.
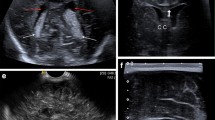
Differentiating an intraluminal bleed from a large GMH may be difficult (Fig. 1). A colour Doppler scan may provide diagnostic information [2] when it demonstrates coloured signals, alternately coded red and blue, in the Sylvian aqueduct (Fig. 1). This is explained by the presence of small particles in the CSF that produce turbulent flow in the CSF pathways. The most sensitive area is the narrowest portion of the aqueduct of Sylvius. The coloured CSF signal may be seen spontaneously, but is more common with patient activity, e.g. sucking, crying, leg movements, etc. It may be produced by some manoeuvres that are easy to perform in a ventilated sedated newborn, such as abdominal palpation or intermittent compression of the anterior fontanelle. This finding lacks specificity since it may be observed in postinfectious ventriculitis, but is especially informative in the context of the preterm newborn.
Germinal matrix and intraventricular haemorrhages. a On this coronal scan, bilateral germinal matrix haemorrhages are obvious, but is there an associated intraventricular bleed? b, c Colour Doppler, midline sagittal scans. Alternate red and blue coloured signals (thick arrows) are detected within the aqueduct of Sylvius and intraventricular haemorrhage is confirmed (1 anterior cerebral artery, 2 basilar artery, 3 pericallosal artery, 4 internal cerebral vein, 5 fourth ventricle)
Periventricular haemorrhagic infarction
When ultrasonography shows a large, strongly echogenic area, round or fan-shaped, lateral to the external angle of the lateral ventricle, associated with a large ipsilateral IVH (Fig. 2), the diagnosis of periventricular haemorrhagic infarction (PVHI) is made [3]. The volume of periventricular infarct should be assessed. Almost the whole hemispheric white matter may be involved (Fig. 2), resulting in extensive macrocystic destruction. At the opposite extreme, the infarct may remain focal and small (Fig. 2). It progressively cavitates, decreases in size and becomes confluent with the ventricular lumen.
Ischaemic–haemorrhagic infarction. a Coronal scan demonstrates a large intraventricular haemorrhage associated with a fan-shaped, hyperechoic, right parenchymal ischaemic–haemorrhagic infarction (arrowheads). b Oblique sagittal scan, lateral to the right ventricle. The haemorrhagic infarct involves almost the whole hemispheric white matter. c In this different neonate, the infarction remains focal, small and round in shape
Periventricular infarction probably results from compression or obstruction of terminal veins (that drain the white matter via the medullary veins) by a large GMH or IVH [4, 5]. In normal infants, and on the normal side, the terminal vein is always easily shown by colour Doppler scan [6]. By contrast, when PVHI has occurred, flow is no longer detectable in the terminal vein [7]. This is interesting because disappearance of venous flow precedes the imaging of the periventricular infarct. Thus, it is part of the examination to look for terminal vein flow when a large clot is visible, in order to predict the subsequent occurrence of periventricular infarction that is grade IV haemorrhage. In patients with large intraventricular bleeding and patent terminal vein flow, PVHI does not occur [6].
Other white-matter disease may be encountered associated with IVH [8], especially PVL (Fig. 3). It is important to distinguish this damage from ischaemic–haemorrhagic infarction since their pathogenesis, sonographic features and neurodevelopmental outcome differ [3].
IVH-PVH and cerebral blood flow velocities
The pathogenic mechanisms that are responsible for haemorrhagic damage are multifactorial, but are mainly the result of intravascular factors [9–11]. Assessing cerebral blood flow (CBF) velocities by pulsed Doppler scan is now possible; thus, this procedure is proposed to detect situations at high risk of haemorrhage. Perlman et al. [12] were the first to describe a Doppler pattern characterized by beat-to-beat variability along the spectrum (Fig. 4). These fluctuations were mainly observed when the infant was breathing out of synchrony with the ventilator and were considered to result from the loss of cerebral autoregulation with direct transmission of arterial blood pressure variations to the cerebral blood circulation, as a pressure passive state [10, 13]. Other circumstances may be responsible for this state, such as upper airway obstruction, pneumothorax, manoeuvres of routine care, rapid volume expansion, etc [11]. A correlation between the fluctuating pattern and subsequent development of IVH [12], and between the elimination of this aspect and a decreased incidence of IVH [14] has been documented. These studies alerted paediatricians to the importance of avoiding these high-risk situations, and nowadays identification of a fluctuating Doppler trace has become extremely rare.
Normal values of velocities have been defined in preterm and full-term neonates [6]. Arterial velocities increase with age, and is significantly higher at term than at 32 weeks of gestation (Fig. 5), while resistive index (RI) does not significantly differ between these two age groups. This is one of the arguments that highlights the great importance of measuring the velocities and not only RI. However, in preterm infants less than 32 weeks of gestation, the normal values of velocities are lower.
It is important to keep in mind that a haemodynamic study should never be interpreted alone, but should be correlated with the systemic haemodynamic state, the postnatal age [15–17], and blood gas concentrations. Hypoxia and hypercapnia are strong vasodilators that induce increases in diastolic velocities and decreases in RI. When a normal newborn is stimulated (as by cutaneous stimulation) [6], the heart rate increases and the peak-systolic velocity does not change, but end-diastolic velocity and, as a consequence, time-average velocity significantly increase, resulting in a decrease in RI. Velocities return to normal later than the end of stimulation and normalization of heart rate. This is normal autoregulation. The same changes occur after a transient bradycardia or hypoxia.
Thus the main role of the brain US Doppler scan is to detect haemodynamic situations at high risk of resulting in ischaemic–haemorrhagic injury, especially when the US examination is performed early after birth, before day 2. It may be a fluctuating Doppler curve [12], a severe increase in CBF (high velocities, mainly diastolic, with low RI) [18], or a severe decrease in CBF velocities [19].
Despite its interest, Doppler investigation represents a limited approach to neonatal cerebral haemodynamics since it assesses only flow velocities during a short period of examination. Thus, only abnormal results have predictive or prognostic value.
Posthaemorrhagic ventricular dilatation
This affects approximately 36% of preterm infants with IVH, but resolves in 65% of affected infants [11]. The diagnosis is based on morphological imaging that demonstrates the onset of ventricular dilatation (Fig. 6) and determines its progression or resolution. It differentiates non-communicating tetraventricular dilatation with a rounded fourth ventricle and brainstem compression, from a communicating dilatation with a triangular-shaped fourth ventricle and clearly visible cisterna magna.
The pulsed Doppler scan provides additional information by demonstrating an increased RI in the presence of increased intracranial pressure (ICP). Intracranial hypertension is associated with reduced end-diastolic velocity and an increased RI that may exceed 1. Another cause of such an abnormal spectrum, such as patent ductus arteriosus, should be excluded first. Progressive hydrocephalus is highly correlated with a high RI but when the dilatation is only slowly progressive, clinical and haemodynamic assessments may be discordant. Some authors [20, 21] have proposed increasing the sensitivity of the Doppler investigation by applying fontanellar compression. Indeed, in a healthy infant, when pressure is exerted on the anterior fontanelle, ICP rises, end-diastolic velocity decreases and RI increases. But, when intracranial volume is already increased as in hydrocephalic infants, the pressure–volume relationship is altered and simple manual fontanelle compression induces excessive changes in CBF velocities. Taylor and Madsen [21] have proposed an index called deltaRI, defined as fontanelle compression RI−baseline RI/baseline RI. They found that deltaRI is less than 30% in infants who do not require shunt placement, contrasting with more than 45% in infants who require shunt placement. This procedure may be used for deciding on therapeutic intervention if correlated with other available data. Thus, the course of posthaemorrhagic dilatation may be followed by a pulsed Doppler scan especially when some treatments are considered. The determination of RI may guide CSF removal or the shunting procedure.
To summarize, in cerebral haemorrhagic injury, ultrasonography (1) permits the positive diagnosis of the damage and documents its severity, (2) demonstrates some haemodynamic disturbances at high risk of haemorrhage, and (3) plays a major role in the follow-up and management of posthaemorrhagic ventricular dilatation.
White-matter ischaemic damage
Early sonographic aspects of periventricular leucomalacia
The sonographic diagnosis of PVL lies in the detection of an abnormal periventricular parenchyma and is recognized as difficult. Parenchymal echo densities may be evident and show a variable pattern (Fig. 7): lateral extension with spiculated margins, high hyperechogenicity with sharp margins, organization in clusters, butterfly appearance, and extensive density with scattered punctate densities. The distribution of the lesion may be considered either bilateral and diffuse, or focal and nodular (Fig. 7). However, periventricular echodensities may be less obvious, with a hazy pattern, spiculated margins, or only punctate densities within white matter of normal echogenicity (Fig. 7).
These appearances should be distinguished from some features that are encountered in extremely preterm neonates, usually before 28 weeks of gestation (Fig. 8). Echogenic stripes may be observed, parallel to the external wall of the ventricles without other parenchymal abnormality. They remain unchanged during the first weeks of follow-up and are probably related to a layer of migrating cells.
In some situations, the echodensity of posterior white matter is difficult to appreciate, for example with posthaemorrhagic dilatation. Accessory windows should be investigated, such as the posterior or mastoid fontanelles.
Periventricular echodensities: PVL or not?
The first argument is development of cysts. When macrocysts appear, with their progressive confluent extension, the diagnosis is easy, but it is nowadays a rare situation. Most often, there are microcysts (Fig. 9), which are more difficult to detect even if surrounded by hyperechoic white matter. They appear between day 8 and day 25 after any type of echodensity. Their recognition is important since they are correlated with an abnormal clinical outcome [22, 23].
Preterm infant (29 weeks’ gestation) with periventricular echodensities on day 5 and day 11. Multiple bilateral tiny cysts (arrows) are apparent within the centrum semiovale on day 18 and confirmed on US imaging and MRI follow-up. This microcystic leucomalacia was correlated with spastic triparesis at 18 months of age
Usually, no cysts are detected. The severity and extension of echodensities may determine the diagnosis [24], as well as their pattern, especially the presence or absence of parenchymal distortion. However, the main criterion is the duration of echodensities [25, 26]. Early normalization (<7 days) is associated with a favourable outcome [27], while late persistence of an abnormal aspect is associated with motor sequelae. Nevertheless, there is widespread agreement that MRI is more sensitive than US imaging for evaluating white-matter damage.
Gangliothalamic involvement
This is easily diagnosed sonographically as it appears as rounded, well-defined hyperechogenicities (Fig. 10). It should be differentiated from the slight, thin lenticulostriate echodensity, characteristic of extreme prematurity. Usually, other parenchymal ischaemic damage is associated [28]. Isolated small lesions may be detected in the thalami, but their clinical significance is uncertain.
Cortical necrosis
Infrequent in preterm infants, it occurs mainly after a specific acute perinatal event [11]. The lesions appear (Fig. 11) as a hyperechoic ribbon along the interhemispheric fissure, or as small, round echogenic nodules, centered on a sulcus and contrasting with normal hypoechoic cortex. They are usually multifocal and bilateral, but asymmetrical, resulting in a patchwork aspect of brain parenchyma.
In rare cases, cortical necrosis is a focal superficial lesion, at first hyperechoic and round, but rapidly progressing to curvilinear liquefaction of its peripheral subpial area and heterogeneity of its central area. This lesion is attributed to thrombosis of pial vessels with underlying cortical necrosis.
Delayed ischaemic–haemorrhagic damage
This occurs mainly in unstable or extremely premature infants (<25 weeks of gestation) [29], especially after acute septic events. PVL, multifocal haemorrhagic infarcts (Fig. 12), ischaemic damage of the corpus callosum (with transient enlargement and subsequent volume reduction) (Fig. 12), and acute subarachnoid haemorrhage [30] with underlying parenchymal necrosis may all be encountered. Thus, sonographic follow-up of the preterm brain should be prolonged even if the neonatal period has not shown ischaemic–hemorrhagic damage [31], especially when there have been intercurrent acute events.
A 27-week premature infant with normal sonography on day 4. Acute severe sepsis on day 6; echodense periventricular white matter on day 9. a Routine scan on day 14 shows multiple hyperechoic nodules (arrows) within the white matter suggesting haemorrhagic infarcts. b–d Subsequent development of diffuse macrocysts. Concurrently there is callosal ischaemic damage. The corpus callosum is normal in size (2 mm) on day 4 (b), swollen (3.4 mm) on day 10 (c), and atrophic (1.1 mm) on day 30 (d)
Late sonographic examination
We routinely perform the final US examination when the infant reaches term [32, 33]. This is to detect persistent ventricular enlargement, pericerebral fluid effusion and decreased volume of the corpus callosum that may indicate white-matter damage and decrease in cerebral volume [20, 29].
In conclusion, we have presented the way we use brain US in preterm infants. First, accurate morphological examination remains essential. It is combined with Doppler analysis, the results of which are correlated with the clinical history, the systemic haemodynamic condition and blood gas concentrations. Second, is there a best time for sonography? If the diagnosis of established ischaemic–haemorrhagic lesions is the only goal then performing the first US scan on day 3 or 4 is appropriate. However, if detection of an at-risk situation is the priority then early examination on the first day of life is required. Third, sonography should be repeated, not only to confirm and follow a recognized abnormality, but also to detect previously undiagnosed injury or a newly established lesion, especially when there has been an acute clinical event.
References
Couture A, Veyrac C, Baud C (1994) Echographie cérébrale du foetus au nouveau-né. Imagerie et hémodynamique. Sauramps, Montpellier
Winkler P (1992) Color-coded echographic flow imaging and spectral analysis of CSF in meningitis and hemorrhage. Part I: clinical evidence. Pediatr Radiol 22:24–30
De Vries LS, Roelants-van Rijn AM, Rademaker KJ, et al (2001) Unilateral parenchymal haemorrhagic infarction in the preterm infant. Eur J Pediatr Neurol 5:139–149
Gould SJ, Howard S, Hope PL, et al (1987) Periventricular intraparenchymal cerebral hemorrhage in preterm infants: the role of venous infarction. J Pathol 151:197–202
Takashima S, Mito T, Anto Y (1986) Pathogenesis of periventricular white matter hemorrhage in preterm infants. Brain Dev 8:25–30
Couture A, Veyrac C (2001) Transfontanellar Doppler imaging in neonates. Springer, Berlin Heidelberg New York
Taylor GA (1995) Effect of germinal matrix hemorrhage on terminal vein position and patency. Pediatr Radiol 25:S37–S40
Kuban K, Sanocka U, Leviton A, et al (1999) White matter disorders of prematurity: association with intraventricular hemorrhage and ventriculomegaly. The Developmental Epidemiology Network. J Pediatr 134:539–546
Lou HC, Lassen NA, Tweed WA, et al (1979) Pressure passive cerebral blood flow and breakdown of the blood–brain barrier in experimental fetal asphyxia. Acta Paediatr Scand 68:57–63
Lou HC, Lassen NA, Friis-Hansen B (1979) Impaired autoregulation of cerebral blood flow in the distressed newborn infant. J Pediatr 94:118–121
Volpe JJ (1995) Neurology of the newborn, 3rd edn. Saunders, Philadelphia
Perlman JM, McMenamin JB, Volpe JJ (1983) Fluctuating cerebral blood flow velocity in respiratory distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med 309:204–209
Ahmann PA, Dykes FD, Lazzara A, et al (1983) Relationship between pressure passivity and subependymal intraventricular hemorrhage as assessed by pulsed Doppler ultrasound. Pediatrics 72:665–669
Perlman JM, Goodman S, Kreusser KL, et al (1985) Reduction in intraventricular hemorrhage by elimination of fluctuating cerebral blood flow velocity in preterm infants with respiratory distress syndrome. N Engl J Med 312:1253–1257
Meek JH, Tyszczuk L, Elwell CE, et al (1998) Cerebral blood flow increases over the first three days of life in extremely preterm neonates. Arch Dis Child Fetal Neonatal Ed 78:F33–F37
Pryds O, Greisen G, Lou H, et al (1989) Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 115:638–645
Winberg P, Sonesson SE, Lundell BP (1990) Postnatal changes in intracranial blood flow velocity in preterm infants. Acta Paediatr Scand 79:1150–1155
Blankenberg FG, Loh NN, Norbash AM, et al (1997) Impaired cerebrovascular autoregulation after hypoxic-ischemic injury in extremely low-birth-weight neonates: detection with power and pulsed wave Doppler US. Radiology 205:563–568
Meek JH, Tyszczuk L, Elwell CE, et al (1999) Low cerebral blood flow is a risk factor for severe intraventricular hemorrhage. Arch Dis Child Fetal Neonatal Ed 81:F15–F18
Taylor GA (1992) Effect of scanning pressure on intracranial hemodynamics during transfontanellar duplex Doppler examinations. Radiology 185:763–766
Taylor GA, Madsen J (1996) Neonatal hydrocephalus: hemodynamic response to fontanelle compression. Correlation with intracranial pressure and need for shunt placement. Radiology 201:685–689
De Vries LS, Eken P, Groenendaal F, et al (1993) Correlation between the degree of periventricular leukomalacia diagnosed using cranial ultrasound and MRI later in infancy in children with cerebral palsy. Neuropediatrics 24:263–268
Pierrat V, Duquennoy C, Van Haastert IC, et al (2001) Ultrasound diagnosis and neurodevelopmental outcome of localised and extensive cystic periventricular leucomalacia. Arch Dis Child Fetal Neonatal Ed 84:F151–F156
Van Wezel-Meijler G, Van der Knaap MS, Oosting J, et al (1999) Predictive value of neonatal MRI compared to ultrasound in premature infants with mild periventricular white matter changes. Neuropediatrics 30:231–238
Jongmans M, Henderson S, de Vries L, et al (1993) Duration of periventricular densities in preterm infants and neurological outcome at 6 years of age. Arch Dis Child 69:9–13
Lai FF, Tsou KY (1999) Transient periventricular echodensities and developmental outcome in preterm infants. Pediatr Neurol 21:797–801
Dammann O, Leviton A (1997) Duration of transient hyperechoic images of white matter in very-low-birthweight infants: a proposed classification. Dev Med Child Neurol 39:2–5
Leijser LM, Klein RH, Veen S, et al (2004) Hyperechogenicity of the thalamus and basal ganglia in very preterm infants: radiological findings and short-term neurological outcome. Neuropediatrics 35:283–289
Nwafor-Anene VN, DeCristofaro JD, Baumgart S (2003) Serial head ultrasound studies in preterm infants: how many normal studies does one infant need to exclude significant abnormalities? J Perinatol 23:104–110
Chamnanvanakij S, Perlman JM (1999) Extensive late-onset primary subarachnoid hemorrhage in a preterm infant. Pediatr Neurol 21:735–738
O’Shea TM, Counsell SJ, Bartels DB, et al (2005) Magnetic resonance and ultrasound brain imaging in preterm infants. Early Hum Dev 81:263–271
Ment LR, Bada HS, Barnes P, et al (2002) Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58:1726–1738
Townsend SF, Rumack CM, Thilo EH, et al (1999) Late neurosonographic screening is important to the diagnosis of periventricular leukomalacia and ventricular enlargement in preterm infants. Pediatr Radiol 29:347–352
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veyrac, C., Couture, A., Saguintaah, M. et al. Brain ultrasonography in the premature infant. Pediatr Radiol 36, 626–635 (2006). https://doi.org/10.1007/s00247-006-0202-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-006-0202-6