Abstract
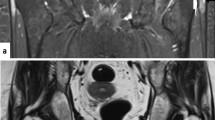
Background: A hyperdense line on the ilium that runs roughly parallel to the sacroiliac joint (we called it “iliac hyperdense line sign”) was frequently observed on pelvic radiographs of patients with gluteal muscle contracture (GMC). A literature search revealed no description of this sign. Objective: To determine the relationship between the iliac hyperdense line sign and GMC and to explore how this sign is formed. Materials and methods: Pelvic plain films of 103 cases of GMC and those of 200 control individuals were reviewed for the presence or absence of the iliac hyperdense line sign. Pelvic CT scans in 8 of 103 cases and 13 of 200 controls were analyzed with relation to the plain films. Results: The iliac hyperdense line sign was visualized in 85 of 103 (82.5%) cases of GMC and none of the 200 controls. In the GMC group, pelvic CT scans showed a deformity of the posterior ilium. The lateral cortex of the posterior ilium took on a partly or completely anteroposterior course, while in the control group the course appeared as an oblique orientation from posteromedial to anterolateral. Conclusion: The iliac hyperdense line on pelvic plain film can be used as a radiographic sign to suggest a diagnosis of GMC. This sign might be a result of the long and persistent pulling effect of the contracted gluteus maximus muscle, which deforms the lateral cortex of the posterior ilium from an oblique course to an anteroposterior course tangential to the X-ray beam.



Similar content being viewed by others
References
Lejman T, Sulko J, Michno P (1995) Surgical treatment of post injection contracture of the hip in children. Chir Narzadow Ruchu Ortop Pol 60:39–41
Liu G, Du J, Yang S, et al (2000) A retrospective analysis of the gluteal muscles contracture and discussion of the relative problems. J Tongji Med Univ 20:70–71
Chen SS, Chien CH, Yu HS (1988) Syndrome of deltoid and/or gluteal fibrotic contracture: an injection myopathy. Acta Neurol Scand 78:167–176
Chung DC, Ko YC, Pai HH (1989) A study on the prevalence and risk factors of muscular fibrotic contracture in Jia-Dong Township, Pingtung county, Taiwan. Gaoxiong Yi Xue Ke Xue Za Zhi 5:91–95
Sun X (1990) An investigation on injectional gluteal muscle contracture in childhood in Mianyang city. Zhonghua Liu Xing Bing Xue Za Zhi 11:291–294
Gao GX, Zheng YY (1985) Idiopathic contracture of the M gluteus maximus in children. Chin Med J (Engl) 98:803–806
Napiontek M, Ruszkowski K (1993) Paralytic drop foot and gluteal fibrosis after intramuscular injections. J Bone Joint Surg Br 75:83–85
Hang YS (1979) Contracture of the hip secondary to fibrosis of the gluteus maximus muscle. J Bone Joint Surg Am 61:52–55
Bowen JR, MacEven GD, Mathews PA (1981) Treatment of extension contracture of the hip in cerebral palsy. Dev Med Child Neurol 23:23–29
Shen YS (1975) Abduction contracture of the hip in children. J Bone Joint Surg Br 57:463–465
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, JH., Gan, LF., Zheng, HL. et al. Iliac hyperdense line: a new radiographic sign of gluteal muscle contracture. Pediatr Radiol 35, 995–997 (2005). https://doi.org/10.1007/s00247-005-1519-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-1519-2